Introduction
Stroke occurs when blood perfusion is reduced, leading to neuron death; ischemic events present around 85% and hemorrhagic in 15%. Ischemic events are classified into embolic, thrombotic, or lacunar1. Although hypertensive decontrol is the main etiology, some others as clotting disorders, carotid dissection, or drugs must be investigated2.
Chronic inflammation led to higher platelet levels and lower lymphocytes levels, increasing the risk of stroke events3. Platelets reflect inflammation, and the mean platelet volume (MPV) express platelet activation, this marker is elevated in stroke and is associated with poor outcome; on the other hand, the level of platelet count (PC) is inversely proportional to MPV in stroke, this might be related to the increasing consumption in the process of thrombus formation4.
The MPV/PC index is a better indicator of inflammation and platelet activation compared to MPV or PC alone5. This inflammation is even found in some tumors, including hepatocellular carcinoma, pancreatic cancer, and lung cancer, increasing the MPV/PC index6.
High levels of MPV and neutrophils lymphocytes ratio (NLR) are found in carotid artery stenosis and cardiac arrest7. However, NLR and MPV are higher when carotid artery stenosis is between 70 and 99%7.
Platelet size plays an important role as a cardiovascular risk factor, while NLR and platelet/lymphocyte index express systemic inflammation8. Low platelets levels are related to thrombosis events, increasing cardiac events and mortality9. Furthermore large platelets are more reactive than small platelet10.
Previously some other indexes were studied, specially the MPV, NLR, and erythrocyte sedimentation rate (ESR) which are related with C-reactive protein (CRP) in stroke events; males keep better relation between CRP/NLR and ESR indexes, while females have a good relation between CRP/MPV and NLR/ESR indexes11.
The MPV expresses platelet production and inflammation, increasing the prothrombotic events12. However, there is a direct relation between platelet size in cardiovascular events, increasing the cardiovascular risk in patients with large platelets8.
The MPV and MPV/PC are higher in stroke events, even in patients who suffered cardiac arrest or post-AMI stroke13. Opposite to acute inflammation, lower levels of MPV express chronic inflammation and rheumatic diseases14. The increase in MPV and NLR/PLT predicts severity of stroke and TIA at admission and after 3 months15.
Despite the fact that MPV increases in stroke events, this may be increased in other diseases such as hypertension, diabetes, and atrial fibrillation, increasing the risk of stroke16. The MPV predicts outcomes in stroke events, and even during the following 90 days after thrombolysis events17. The MPV is higher in acute non-lacunar than lacunar ischemic strokes, and this is directly related to the MPV and lesion size18.
The high platelet levels are increased in all cardiovascular events, especially in myocardial infarction and ischemic stroke, this fact increases mortality in all stroke events19. The MPV, as an expression of platelets activation, is useful for prognosis of cardiovascular and stroke20. On the other hand, platelets activation expresses inflammation which produces brain damage and leads to spread microvascular dysfunction, edema enlargement, and eventually worsen functional outcomes21; this is reflected with higher MPV levels, which are found in all stroke types22.
Methods
This is a cross-sectional study that was done during the period from April 2020 to January 2022. Patients with ages over 18 years old were included into the analysis, including all types of strokes, demonstrated with imaging study (brain tomography or brain magnetic resonance) during the first 48 h of the event, with hematic cytometry at hospital admission, and interned into any hospital service. Hemorrhagic events were considered as stroke; however, just ischemic events were considered in the final analysis. We collect laboratory parameters from all hematic cytometry of WBC, MPV, neutrophils, lymphocytes, platelets; demographic parameters, sex, age; and stroke events, type of stroke, hospital stay days, hospital stay until discharge, die, or alive. All these parameters were analyzed and we obtained a relation between number of neutrophils and lymphocytes (N/L), which were considered normal with values between 0.78 and 3.53, and was divided into three three groups, low risk < 1.5, intermediate risk 1-5-3, and high risk > 3. The VPM was considered normal with values from 7 to 10 fl, a relation between VMP and platelets count was obtained, with a VPM/PC index was normal if the relation was lower than 0.031. Hematic cytometry was collected at admission and during hospitalization. Kaplan–Meier survival statistics and the log-rank test were used to compare stroke events according to sex, N/L, and MPV/PC index and type of stroke. A plot for comparison of receiver operating characteristic curve (ROC) curves among MPV/PC and N/L index was done. All the tests were two-sided and p-value < 0.05 was considered significant. All analyses were done using SPSS 20.0 (SPSS, Inc., Chicago, IL, USA).
Results
We collected 236 patients including 137 males (74-78 years) and 81 females (64-72 years); with 58 hemorrhagic cases, including 44 parenchymal, eight subarachnoid, and six subdural; and 160 ischemic cases, including 149 ischemic, 2 lacunar, and 9 TIA. Only 18 patients were discharged to other health-care centers, excluding these patients from final analysis. A neutrophils/lymphocytes index lower than 3 (p 0.015) had a 68.4% of sensitivity and 83.2% of specificity, with a PPV of 72% and NPV of 89%; and a MPV/PC index higher than 0.031 (p = 0.001) with a 71.2% of sensitivity and 84.9% of specificity, with a PPV of 62% and NPV of 94%; both indexes increased significantly in stroke patients during the first 48 h from the event, increasing hospital stay days at medium of 15 days (13-18 days). The correlation between serum parameters and mortality in stroke according to sex group is presented in Kaplan–Meier graph (Fig. 1). Values > 10 fl of MPV were found to increase significantly in dead patients (p = 0.014); considering all strokes, a total of 37 patients died (63.7%) because of a hemorrhagic event, and 92 (57.5%) because ischemic event, this mainly related to complications of long hospital stay. However, both indexes had a good specificity to predict mortality and long stay days in ischemic events, being useless in hemorrhagic events; ROC analysis showed that areas under the curve (AUC) values were MPV/PC 0.822 (0.760-0.885) (p = 0.001) and N/L 0.661 (0.579-0.742) (p = 0.001) with a significant difference between AUC values (p = 0.001).
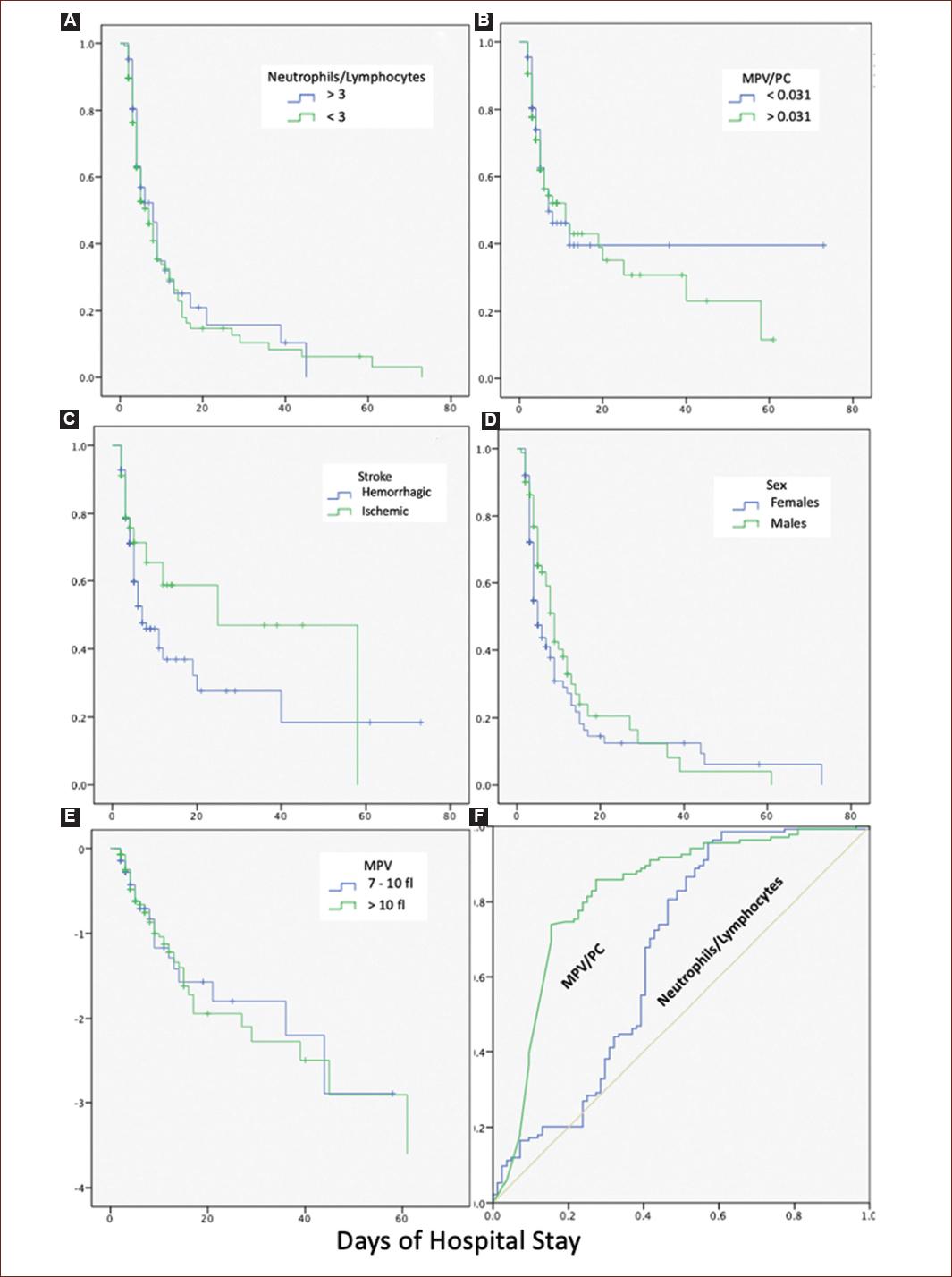
Figure 1 A: Kaplan–Meier plots showing. Increase in mortality in patients with neutrophils/lymphocytes index lower than 3. B: increase in mortality in patients with MPV/PC index higher than 0.031. C: increase in mortality in patients with hemorrhagic stroke, compared to ischemic stroke. D: mortality according to sex. E: increase in mortality of patients with levels higher than 10 fl of MPV. F: ROC curve comparing MPV/PC and neutrophils/lymphocytes indexes predicting mortality.
Discussion
The relation between platelets and thrombotic events is well studied; however, platelets play an important role in inflammation, it has been reported that MPV is a good indicator of platelet size and activity, helping as an inflammatory marker in cardiovascular events and stroke23. However, the MPV values are useful as the severity index of stroke, while the N/L index helps to express systemic inflammation24. Thereby leukocytes help into the atheroma formation; while leukocytosis is involved into plaque destabilization, inducing acute thrombotic events as stroke events, so lower N/L index could be related with a good prognosis. We found that the N/L index was significantly lower, while the MPV/PC index was higher during the first 48 h of stroke; these indexes can help to distinguish between systemic inflammation and local thrombosis mainly during the first 48 h of the event; however, both indexes are an independent predictor of long hospital stay and morality in stroke patients, even ischemic events had a high mortality, the hemorrhagic events are still the more lethal events, so MPV/PC and N/L indexes are useless to predict mortality in those events.
The clinical data showed that patients with in-hospital strokes were more likely to have long hospital stay days and high mortality; this is directly related to high MPV levels, as well as, high MPV/PC index, and lower N/L index, which were found in our study population during stroke events. The main finding of our study relates to the association of N/L index and MPV/PC index as accessible and non-invasive indexes of prognosis in stroke patients.











 nueva página del texto (beta)
nueva página del texto (beta)


