Non-alcoholic fatty liver disease (NAFLD) is becoming the most prevalent liver disease in western countries due to the outbreak of diabetes and obesity together with the successful antiviral therapy against hepatitis C and hep atitis B. NAFLD is strongly related to metabolic syndrome and insulin resistance seems to play a crucial role.1 Hepatitis C virus infection has been strongly related to insulin resistance and steatosis has been a hallmark in liver biopsies of patients with hepatitis C. The core protein of the virus seems to promote insulin resistance by inducing degradation of insulin receptor substrate-1. Epidemiological studies including cross-sectional and longitudinal studies together with in vitro studies and interventional studies demonstrated this interaction: hepatitis C virus promotes insulin resistance, steatosis and fibrosis progression and the clearance of the virus was associated with the improvement or disappearance of insulin resistance. However, no molecular relationship between hepatitis B viral cycle and insulin resistance has been reported. In recent years,2 some studies addressed the association between hepatitis B and NAFLD, emerging three ideas:
Hepatitis B virus infection seems to protect against steatosis, metabolic syndrome and insulin resistance.
In patients with hepatitis B the presence of metabolic syndrome has been associated with increased risk of disease progression to cirrhosis and liver cancer,3 and
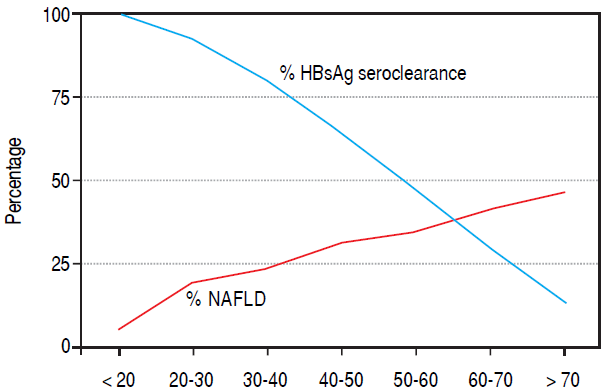
HBsAg clearance was more often seen in older age and advanced liver disease4 and it could be a confounding factor when analysing NAFLD and hepatitis B prevalence.
However, some aspects should be taken into account when interpreting data from the literature. Studies have been conducted on Asian population and the genetic background; the prevalence of NAFLD and the distribution of hepatitis B genotypes differ from the Caucasian population. Prevalence of NAFLD is lower in Easter patients and it appears in people with lower grade of obesity. Lastly, hepatocyte steatosis seems to be related to hepatitis B genotype. Mixed infections with genotype A and G promoted steatosis and fast progression of the disease. However, genotype B has been more often associated with spontaneous clearance of the infection, at least in comparison with genotype C. Nevertheless, a meta-analysis including 4100 patients from 17 studies demonstrated no influence of genotype on fat accumulation, but a negative association was found between viral load and steatosis in patients with chronic hepatitis B demonstrated by liver biopsy.5 Risk factors associated with NAFLD are similar in patients with hepatitis B (body mass index, abdominal perimeter, glycemia, HDL-cholesterol and ALT levels) than patients without hepatitis B (male sex, age, metabolic syndrome, insulin resistance and ALT levels), being obesity and type 2 diabetes key risk factors.1 An inverse relationship between steatosis and positive HBsAg status was found in obese patient, overweight or older than 50 years but not in younger patients.6 In the current study we are comment by Joo, et al., the authors addressed a longitudinal approach to analyse the relationship between hepatitis B and NAFLD. (7 The study included a large cohort of Asian patients with hepatitis B. Nevertheless, a few aspects require attention. Genetic background was restricted to Asian population and thus, these data require validation in external cohorts. Viral load and HBeAg were unknown in this large cohort in spite of they are well known risk factor for fibrosis progression. Education was high and bias related to greater access to health system could not be ruled out. We could not exclude active intervention of physicians improving health status of these patients promoting changes in life style to keep ideal weight and maintain physical activity that could be related with reduced rate of NAFLD in this population. No data about antiviral therapy, hypo-lipidemic or anti-diabetic drugs were recorded. Besides, more than 31,500 patients were excluded due to showing steatosis by ultrasound at baseline. It could be of worth to know how many patients were HBsAg positive in patients with data of liver fat infiltration. Hepatitis B infection correlated with obesity, high levels of high-sensitivity C-reactive protein and liver enzymes. A negative correlation was seen with alcohol consumption and hypertriglyceridemia. They observed a significant lower incidence of NAFLD in HBsAg positive patients, even after adjusting for HOMA-IR, age, triglycerides and other metabolic factors. Interestingly, HOMA-IR did not change over the time in a different manner between HBsAg positive or negative patients, and total cholesterol levels decreased over the time significantly in HBsAg positive in comparison with HBsAg negative. The stronger factors associated with incidence of NAFLD in HBsAg were male sex, HOMA-IR > 2.5 and ALT > 36 U/L.
A key aspect is spontaneous clearance of HBsAg that has been estimated around 1-3% per year. Several factors have been found associated with HBsAg clearance: people older than 40 years old, liver cirrhosis, co-infection by hepatitis D or C, lower levels of HBsAg. Nevertheless, in some populations, spontaneous clearance could reach two thirds of patients without apparent causes.5 Animal models infected by genotype B demonstrated that obesity and steatosis impact on the expression of hepatitis B antigens and HBV replication. Thus, NAFLD could modulate host immunity influencing on viral replication. In patients with low viral load and advanced liver disease the possibility of HBsAg clearance increases. Together with the damage promoted by viral infection, other liver diseases like NAFLD/NASH/Cirrhosis could facilitate HBsAg clearance. In cross-sectional studies the low prevalence of hepatitis B in patients with NAFLD-related advanced liver disease could also be explained, at least in part, by increased HBsAg clearance (Figure 1). Indeed, this phenomenon could be more often seen in Asian population with high prevalence of hepatitis B, mother-to-infant transmission and long-duration of the disease. Moreover, genetic background including PNPLA3 and TM6SF2 could influence the prevalence of NAFLD in general population and also in hepatitis B. The intimate relationship between hepatitis B virus and metabolism of cholesterol could also influence this association. Seroconversion rate after development of NAFLD was not addressed in the current study and it could be interesting to define in further ones. In conclusion, the authors demonstrated a weak relationship between hepatitis B virus infection and NAFLD combining in a vicious circle of crossed lives when hepatitis B protects against NAFLD and NAFLD progression promotes HBsAg clearance disguising the prevalence of NAFLD on hepatitis B.











 nueva página del texto (beta)
nueva página del texto (beta)