Introduction
Robinow syndrome is a rare heterogeneous genetic syndrome characterized by short stature, craniofacial, genital, and musculoskeletal anomalies, and normal intellectual ability in most cases. It is also known as fetal face syndrome because the face resembles that of an 8-week-old fetus: small face, laterally displaced eyes, and forward-facing nostrils. The syndrome was first described in 1969 by Dr. Meinhard Robinow, who noticed these phenotypic characteristics in a family of four members1-4.
Approximately 200 cases have been reported worldwide, with an incidence of 1 in 500,000. No sex predilection has been observed (male-to-female ratio 1:1)1-3,5.
Growth hormone deficiency has been identified as a possible etiology of short stature, resulting in lower bone age than chronological age, shortening of limbs, and slower growth rate compared to healthy children of the same age6.
Clinical case
We present the case of a 13-year and 1-month-old male patient who came to the pediatric endocrinology office for a consultation concerning short stature at 3 years.
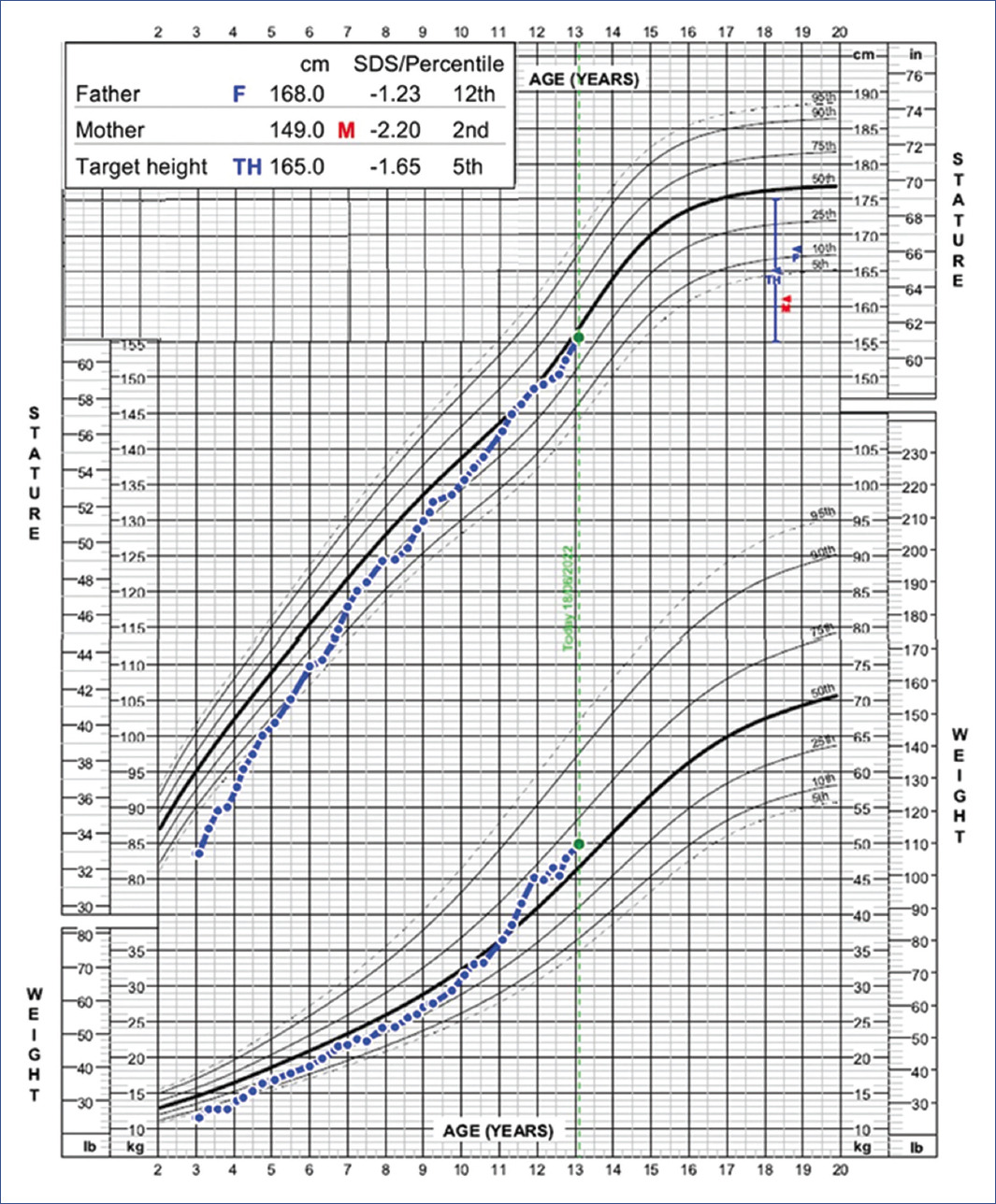
The patient was the product of the mother's third gestation (two previous pregnancies with loss of the product secondary to an unknown cause), in which she presented gestational diabetes. The patient's mother was also diagnosed with Robinow syndrome, with a height of 149 cm (-2.20 SDS, 2nd percentile). The patient's father is healthy, with a height of 168 cm (-1.23 SDS, 12th percentile), resulting in a target height of 165 cm (-1.65 SDS, 5th percentile). The family tree is shown in Figure 1.
At birth, the following congenital defects were reported: systolic murmur, hiatal hernia, bilateral inguinal hernia, ventricular septal defect (VSD), patent ductus arteriosus (PDA), pulmonary valve insufficiency, and bilateral cleft palate. Surgical correction of all these findings was performed with the additional placement of an epicardial pacemaker. Although he presented normal psychomotor development, a delay in language development was observed secondary to a cleft palate.
At the first consultation, the patient presented midface hypoplasia, upslanting palpebral fissures, long eyelashes, wide and depressed nasal bridge, short nostrils with anteversion and discrete bifid nose, long philtrum, downturned corners of the mouth, dysplastic uvula, palate with a bilateral scarring, hypoplastic teeth, micro and retrognathia, low-set ears, short neck, mesomelic and rhizomelic limb shortening, brachydactyly, clinodactyly of the fifth finger and clinodactyly on the second toe, micropenis, transient hypothyroidism, growth hormone deficiency (IGF1 27 ng/ml -1.69 SDS), and growth hormone stimulation test with values < 3.6 ng/mL. As Robinow syndrome was suspected, molecular studies were performed on the patient and his parents. Massive Illumina sequencing studies of the DVL1, DVL3 (disheveled segment polarity proteins 1 and 3), ROR2 (receptor tyrosine kinase-like orphan receptor 2), and WNT5A (Wnt family member 5A) genes were performed with the finding of an unreported variant, c.490T>C, exon 4 of the WNT5A gene. Sanger sequencing showed that the mother was the variant carrier (Figure 2).
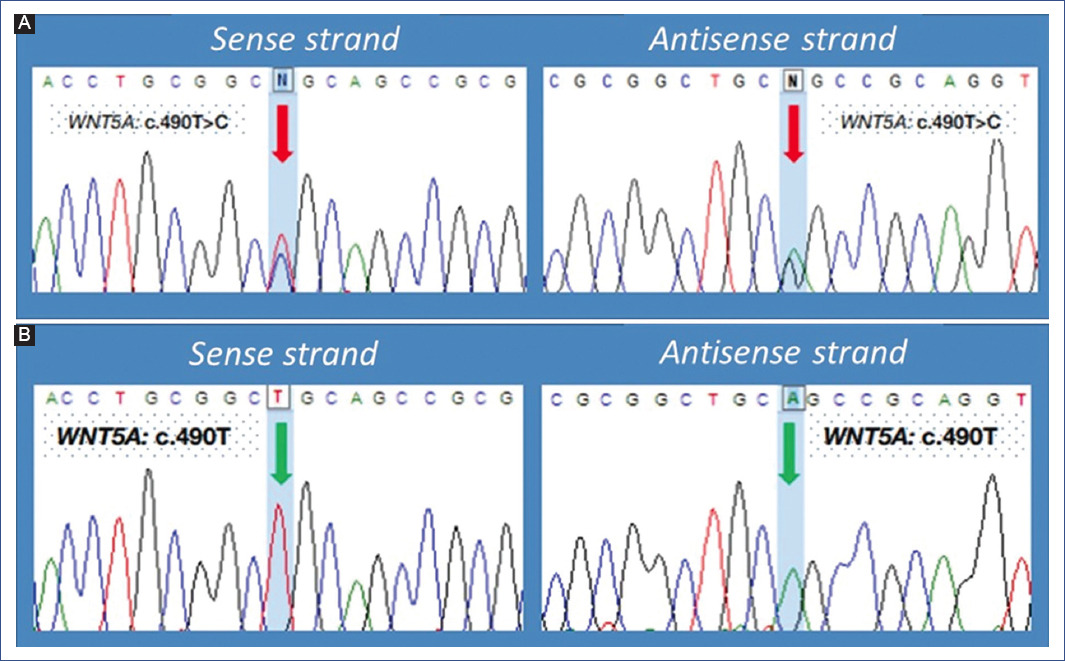
Figure 2 Partial electropherogram of WNT5A gene sequencing in the patient's parents. A: genetic variant c.490T>C, exon 4 of WNT5A gene in the mother. B: normal WNT5A gene in the father.
The patient began treatment with growth hormone at a dose of 0.7 U/kg/week at 4 years. He has shown favorable outcomes, increasing his height from < 1st percentile to the 44th percentile.
Discussion
Genetics
The severity of signs and symptoms and the pattern of heritability distinguish the types of Robinow syndrome. Biallelic variants in the ROR2 and the Nucleoredoxin (NXN) genes have been implicated in the recessive forms of the syndrome. ROR2 protein is essential in embryonic development, contributing to the early formation of chondrocytes and the development of cartilage and growth plates; also, it has been reported to be necessary for normal skeletal, heart, and genitalia formation. Patients with the NXN variant have milder skeletal anomalies than those with the ROR2 variant. Dominant forms of the syndrome have been associated with multiple genes, including variants and deletions of WNT5A on chromosome 3p14.3, as in the present case; however, we identified a new mutation (Figure 2). Other variants described include the DVL1 gene, variants in DVL3, and frizzled class receptor 2 (FZD2). Recently, variants have been described in glypican 4 (GPC4), suggesting a form of X-linked Robinow syndrome3,5,7,8.
Phenotype
The phenotypic presentation of the syndrome is variable. Certain features have been observed to be more prevalent in some genetic variants. However, they have yet to be reported as variant-specific because of discrepancies due to small study populations and global incidence of the syndrome1. The autosomal dominant variant (ADRS) is rare and has been reported with milder craniofacial and musculoskeletal anomalies than the ROR2 variant. The musculoskeletal system is minimally affected, with the possibility of the patient having average stature with little or no limb shortening3,7,8.
Conversely, the autosomal recessive variant (ARRS), especially with ROR2 gene mutations on chromosome 9q22, presents dysmorphism, multiple facial anomalies, limb, and thoracic malformations, rib and vertebral abnormalities, mesomelic short stature and genital malformations2.
Craniofacial alterations. The most frequent malformations are macrocephaly, broad and prominent forehead, low ear implantation, ocular hypertelorism, prominent eyes with deficient lower eyelid, midfacial hypoplasia, short upturned nose with depressed nasal bridge and anteverted nares, large triangular mouth with tent-like upper lip, long philtrum, gingival hypertrophy, misaligned teeth, ankyloglossia, bifid tongue, and micrognathia. Other less frequent findings are cleft lip and palate. Asymmetric exophthalmos was found only in patients with DVL1 and NXN variants, while a saddle nose deformity in DVL1, ROR2, and NXN variants. Typical craniofacial anomalies were observed in this patient (Figure 3A), macrocephaly, low ear implantation, ocular hypertelorism, prominent eyes with deficient lower eyelids, depressed nasal bridge, long philtrum, tent mouth, and micrognathia3,4,9.

Figure 3 A: frontal and lateral phenotypic features of Robinow syndrome. Macrocephaly, low ear implantation, ocular hypertelorism, prominent eyes with deficient lower eyelids, long philtrum, and tent mouth (left panel). Low ear implantation, depressed nasal bridge, and micrognathia (right panel). B: patient at age 10 years. Mesomelic limb shortening (left panel). Low ear implantation, depressed nasal bridge, and micrognathia (upper right panel). Low ear implantation and ocular hypertelorism (lower right panel).
Musculoskeletal alterations. Abu-Ghname et al. found that 100% of the patients had short-limb skeletal dysplasia and, in most cases, mesomelia, followed by micromelia and rhizomelia7. Patients with ROR2 and GPC4 variants had exclusively mesomelic skeletal dysplasia, not found in the NXN variant. Other limb anomalies documented were the radial arch and radial head dislocation and diminished arm rotation. The most prevalent hand anomalies were brachydactyly, clinodactyly, and broad thumb. Genu valgum was a common finding in the lower extremities. Spinal anomalies were directly related to the type of variant: on the one hand, single butterfly vertebra with the autosomal dominant variant; on the other hand, hemivertebra, vertebral fusion, and narrow interpedicular space with the autosomal recessive variant. However, this patient presented only one musculoskeletal anomaly: short limb skeletal dysplasia (Figure 3B). No other anomalies were reported at this level1,2,4,10.
Genital alterations. The most frequently observed anomaly is micropenis, as in the present case. Other anomalies found are penile transposition, cryptorchidism, testicular atrophy, hypospadias, and an elongated penopubic gap in males. In females, the reduced size of the clitoris and hypoplasia of the labia majora predominate. In 1997, Wilcox et al. described the possible etiology of micropenis as secondary to inferior-posterior insertion of the penis on the medial part of the ischial tuberosity, as its normal insertion is on the anteromedial portion of the pubis. Therefore, the penis is buried in the scrotum, resulting in a short appearance of a normal-sized penis. Consequently, many patients should not be classified with a micropenis (stretched penis length < 2.5 SD below the average penis length for age)8,9,11.
Urinary system alterations. Although the most prevalent finding is hydronephrosis, cystic dysplasia of the kidney and renal duplication have also been described. Cases of renal failure of unknown origin have also been reported, but this has not been directly related to Robinow syndrome. This anomaly was not observed in this patient8,9.
Cardiac and pulmonary alterations. Defects at these levels are frequent, causing premature death in childhood and adolescence in 5-10% of patients. Cardiac anomalies are present in approximately 15% of published cases (< 25% of patients with ADRS). The most often reported is pulmonary valve stenosis or atresia. Atrial septal defect, VSD, coarctation of the aorta, tetralogy of Fallot, and tricuspid atresia have also been described. Our patient presented with a systolic murmur at birth, showing VSD, PDA, and pulmonary valve insufficiency. He was treated with surgical correction of these anomalies, and an epicardial pacemaker was placed. He is currently awaiting a new valve replacement; he has no cardiac decompensation and is being treated with diuretics4,8,10,12.
In most cases, no deficit in intellectual functions has been found. However, mental retardation and developmental delay have been observed in up to 20% and 10-15% of the disease carriers, respectively. A frequent finding is the presence of an empty sella turcica. However, it does not seem to be related to GH deficiencies or to predispose to a negative response to hormonal treatment. Developmental brain dysplasia and communicating hydrocephalus have been reported in very few cases, but no distinction has been made between dominant and recessive variants. Hearing loss has also been described in some cases due to cranial osteosclerosis. This patient has no neurological defects, has developed adequately, and attends school with no apparent impairment4,8,10,12-14.
Endocrinology
The characteristic findings in this syndrome are short stature and slow growth velocity (GV). Soliman et al. observed short stature at birth, with a length of 41.1 ± 2.1 cm (-3.7 ± 0.35 SD) and slow GV during the first year of life (13.1 ± 3.1 cm per year). At the end of the first year, the mean height was 57.4 ± 4.9 cm (-5.8 ± 0.9 SD), reflecting a low growth potential14.
In several studies, overall growth was found to be -2.17 SD below the mean. It persists into adulthood but is usually not severe, with a mean final height of –2 SD. Adult height has been reported to range from 161.7 to 170 cm14.
Children with Robinow syndrome display growth hormone deficiency, although normal insulin-like growth factor-1 (IGF-1) concentrations have been described. This patient's low growth deficiency was corroborated with a growth hormone challenge test. Thyroid function tests and morning cortisol concentrations are usually not affected in these patients14.
Diagnosis
Diagnosis is based on clinical suspicion due to craniofacial, musculoskeletal, and genital characteristics of the syndrome. Imaging tests are needed to observe bone anomalies in the extremities, skull, and spine. Subsequently, a genetic panel should be performed to confirm the diagnosis, consisting of DVL1, DVL3, FZD2, NXN, ROR2, WNT5A, and GPC43. It is essential to detect congenital heart defects at birth, as these are the leading cause of mortality in the first year of life4.
In cases with genetic risk, prenatal diagnosis can be performed from 19 weeks of gestation by ultrasound to determine the length of different bone components8.
Differential diagnosis
Aarskog syndrome and achondroplasia should be considered possible differential diagnoses when Robinow syndrome is suspected.
Aarskog syndrome is an X-linked genetic syndrome caused by an FGD1 mutation. This syndrome is characterized by short stature, short hands and feet, craniofacial dysmorphism, genital anomalies, and intellectual disability10,12,15,16.
Achondroplasia is an autosomal dominant genetic syndrome caused by an FGFR3 mutation. This syndrome is characterized by short rhizomelic stature, hyperlordosis, brachydactyly, macrocephaly with frontal prominence, and midface hypoplasia10,12,15,16.
Treatment
There is no cure for Robinow syndrome. Treatment focuses on decreasing clinical manifestations and reducing complications. Musculoskeletal symptoms may improve with physical therapy or prosthesis placement; if these fail, treatment would be surgical. Cardiac anomalies require surgical correction and, in some cases, long-term pharmacological treatment2.
Surgical treatment is performed to correct certain anomalies, such as syndactyly, severe scoliosis secondary to hemi-vertebral or costal anomalies, cleft lip or cleft palate, and anomalous penile insertion9.
Hormonal therapy with human chorionic gonadotrophin and testosterone has improved penile length and testicular volume. This patient was treated with testosterone from the age of 4 years due to micropenis. He responded well to treatment with increased penile length and started puberty at 12.5 years4,9.
An increase in GV has been described following recombinant growth hormone (rhGH) administration; however, an increase in bone age occurs. Consequently, Kawai et al. concluded that rhGH therapy accelerates bone age without significantly increasing final height. Luteinizing hormone supplementation has been reported to improve final height in patients with precocious puberty. We observed an increase in our patient's growth rate, improving his adult height prediction. He started growth hormone replacement at 4 years and consistently improved, reaching the 44th percentile in height (Figure 4). To date, his height is 155.6 cm (-0.14 SDS)2,6,9,12,17. The patient's last bone age reported was 13.16 (Greulich & Pyle), with a chronological age of 12.6 years.
Surveillance
Head circumference should be measured regularly during infancy and childhood. Development assessment should be performed periodically every three months in infants and then every six months to one year. More frequent examinations may be performed if necessary due to identified cognitive delays10.
Dental evaluation is recommended every six to twelve months or as needed. During childhood, a periodic hearing evaluation is also recommended. If cardiac or renal abnormalities are detected, an assessment of these is also required. The patient is currently undergoing treatment with an orthodontist as he needed treatment for micrognathia: mandibular advancement with an intraoral device10.











 nueva página del texto (beta)
nueva página del texto (beta)