Introduction
In December 2019, the emergence of a new coronavirus, SARS-CoV-2, responsible for causing severe pneumonia in China, was confirmed1,2. Subsequently, on March 11, 2020, the World Health Organization declared the resulting disease, named COVID-19, a pandemic3. Although initial data indicated that adults and older adults were the most affected population, within weeks, cases were reported in children under 18 with symptoms of acute respiratory infection. In addition, an unusual increase in cases of Kawasaki disease associated with COVID-19 was observed4.
In Mexico, the first case of COVID-19 was reported in February 2020. As of August 30, 2022, the Dirección General de Epidemiología del Gobierno de México had confirmed 7,329,493 cases of SARS-CoV-2 infection. Of these, 594,420 (8.1%) were patients under 19 years5 (Fig. 1).

Figure 1 Cases of COVID-19 in children under 18 years in Mexico and the State of Mexico. From March 2020 to December 2021, cases of COVID-19 occurred in children under 19 years, with the highest frequency in the 15-19 age group, followed by the 10-14 age group at the national and state levels. In addition, an increase in the number of cases is observed in 2021 compared to 2020, although there was stability in infection rates at the state level. Source: Dirección General de Epidemiología del Gobierno de México.
Worldwide reports indicate low rates of moderate and severe disease in the pediatric population, in contrast to mild disease, characterized primarily by symptoms of fever and cough, followed by rhinorrhea, vomiting, diarrhea, headache, and myalgias1,6-12. Although this age group generally has a favorable prognosis, severe cases have been documented with severe respiratory compromise requiring ventilatory support and, in some cases, resulting in death, especially in individuals with risk factors for developing complications13.
For this reason, the role of children as potential spreaders of infection in the community and schools became one of the most debated issues during the COVID-19 pandemic14,15. This is because the transmission of respiratory pathogens such as SARS-CoV-2 depends on contact patterns and interactions between populations. Therefore, understanding these dynamics in closed environments is critical to ensure the effectiveness of efforts to avoid mass infections16. Contagion in the school environment has been a topic of debate with mixed opinions, largely due to the limited evidence available17. As a result, the decision to reopen schools has been left to governments in various geographical regions and to parents, despite the limited evidence of the spread of SARS-CoV-2 among the student population18.
In Mexico, this issue became relevant in August 2021, during the fourth week of the third wave of SARS-CoV-2 infections when the resumption of classes was announced after several months of suspension of classroom activities. The main concern was the risk of contagion in the exposed group, which intensified the debate on the need to vaccinate this age group19.
The State of Mexico has a population density of more than 15 million inhabitants, the highest in the country. Of these, about 5 million are children. In 2021, a total of 103,023 cases of COVID-19 in children aged 5-14 years were registered in Mexico, of which 7,079 (6.8%) were reported in the State of Mexico20.
In order to evaluate the impact of the reopening of schools in our country, the "Programa Regreso Seguro a Clases para el control de contagios de la COVID-19" ("Safe Return to School Program for the Control of COVID-19 Contagions") has followed the student population. In this program, a continuous analysis was made on the fluctuations in the number of cases reported in the school environment.
Methods
Through a prospective study based on a population-based cohort, students from 18,988 public and private primary and secondary schools in the 19 health jurisdictions of the State of Mexico were followed. This follow-up was carried out for a period of 20 weeks, corresponding to epidemiological weeks 31 to 50 of the year 2021, when these students started the mixed educational modality, combining online and face-to-face classes. In the school year 2021-2022, the total enrollment in the State of Mexico reached 4,251,599 students, 2,149,984 (50.6%) female and 2,101,615 (49.4%) male.
Procedures performed in the Safe Return to School Program
Intersectoral coordination was first established between the Secretariats of Health and Education of the Government of the State of Mexico to conduct epidemiologic surveillance in schools. This was achieved through the regional coordinators of the education system and the jurisdictional directors of the health system, with the objective of keeping a daily record of suspected cases identified in schools or reported to the educational institution by parents or guardians.
For this purpose, daily sanitary filters were established in each school. These filters included the presence of trained teachers responsible for monitoring the temperature and detecting suspicious symptoms such as rhinorrhea, fever, cough, headache, or general malaise at the school entrance for the student population and the teaching and administrative staff.
Daily, the education liaisons sent the health liaisons a negative network format (a method of tracking and maintaining continuous surveillance to help identify suspect cases by notifying units, in this case, schools, of the absence of cases), which was reinforced with active surveillance when cases occurred. Identified cases were referred to health units for confirmation or exclusion by RT-PCR (reverse transcriptase-polymerase chain reaction) and for advice on hygiene measures in the affected homes, classrooms, and schools to break the chain of transmission.
Jurisdictional health personnel followed up with each reported patient by telephone and maintained daily contact until discharge to monitor progress.
Operational definitions
This study included subjects using the following operational definitions as inclusion or exclusion criteria:
- Laboratory-confirmed case of COVID-19: Refers to a person who meets the operational definition of a suspected case and has received a confirmed diagnosis by RT-PCR testing at the ISEM Molecular Biology Laboratory. This laboratory is part of the National Network of Public Health Laboratories recognized by the Instituto de Diagnóstico y Referencia Epidemiológicos "Dr. Manuel Martínez Báez" (InDRE).
- Laboratory-confirmed COVID-19 death: Refers to a deceased person who met the operational definition of a suspected case and received a diagnosis confirmed by the Molecular Biology Laboratory of our institution. This laboratory is a member of the National Network of Public Health Laboratories recognized by the Institute of Epidemiological Diagnosis and Reference "Dr. Manuel Martínez Báez" (InDRE, for its Spanish acronym).
Sources of information
A review of epidemiologic reports was performed to compare the epidemiologic behavior of COVID-19 in the student population of the State of Mexico with that reported at the national level. These reports were obtained through the negative/active network registered by the Subdirección de Epidemiología del Instituto de Salud del Estado de México (ISEM) and were compared with the data published in the Epidemiological Bulletin of the Dirección General de Epidemiología de la Secretaria de Salud (SSA), specifically regarding the weekly report of cases of COVID-19.
Statistical analysis
For statistical analysis, frequencies, percentages, and incidences of COVID-19 per 100 monthly school discharges were calculated. State incidences were compared with the national incidence, with 95% confidence intervals. Microsoft Excel was used for the preparation of tables and graphs and for data analysis.
Results
Demographic characteristics
A total of 3,586 cases were detected and confirmed in schools in the State of Mexico. Of these, 2,048 (57.1%) were children, 1,312 (36.5%) were teachers and 226 (6.3%) came from the administrative staff.
The mean age of the students was 12 ± 3 years, the mean age of the teachers was 52 ± 6 years, and the mean age of the administrators was 43 ± 8 years. 1,115 (48%) of the students were female, 961 (67%) of the teachers were female, and 155 (62%) of the administrators were female. Of the 3,586 individuals who tested positive for SARS-CoV-2, 24 (0.6%) required hospitalization due to clinical data of moderate to severe COVID-19, of whom nine (37.5%) died. Additional details on demographic characteristics are shown in Table 1.
Table 1 Characteristics of individuals testing positive for SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) during epidemiologic surveillance
| Variable | Students, n = 2,048 (%) | Teachers, n = 1,312 (%) | Administrative staff, n = 226 (%) |
|---|---|---|---|
| Mean age of hospitalized patients | 12 | 52 | 52 |
| Type of school | |||
| Public | 1211 (59.1) | 700 (79,7) | 116 (51.3) |
| Private | 837 (40.8) | 267 (20.3) | 110 (48.6) |
| Clinical picture | |||
| Mild | 2023 (98.7) | 1005 (76.6) | 162 (71.0) |
| Moderate | 15 (1.1) | 285 (21.7) | 60 (26.3) |
| Severe | 10 (0.09) | 22 (1.6) | 4 (1.7) |
| Deaths | 1 (0.04) | 7 (0.5) | 1 (0.44) |
| Hospital admissions | 4 (0.19) | 17 (1.2) | 3 (1.3) |
| Hospitalized with vaccination scheme | 0 (0) | 11 (64) | 2 (66) |
| Vaccination | 0 (0) | 967(73.7) | 138 (61.0) |
Epidemiological behavior
The Safe Return to School Program began in 31st epidemiological week of 2021, with a national infection rate of 5.0 and a state rate of 3.79, a difference of 1.21 between the two rates. An increase in the number of cases was observed in both curves for week 33, with a national rate of 10.1 and a state rate of 6.87, a difference of 3.27. However, no school detection cases were reported during weeks 31 to 36.
From epidemiological week 36, school detection cases began to be reported, with an average rate of 0.36 during follow-up until epidemiological week 51. In epidemiological week 40, the highest rate in schoolchildren was recorded, reaching 1.01. From this week on, a decrease in cases was observed, which was maintained until week 50 (Fig. 2). During the surveillance period, 32 schools were closed, representing 0.16% of the total number of schools.
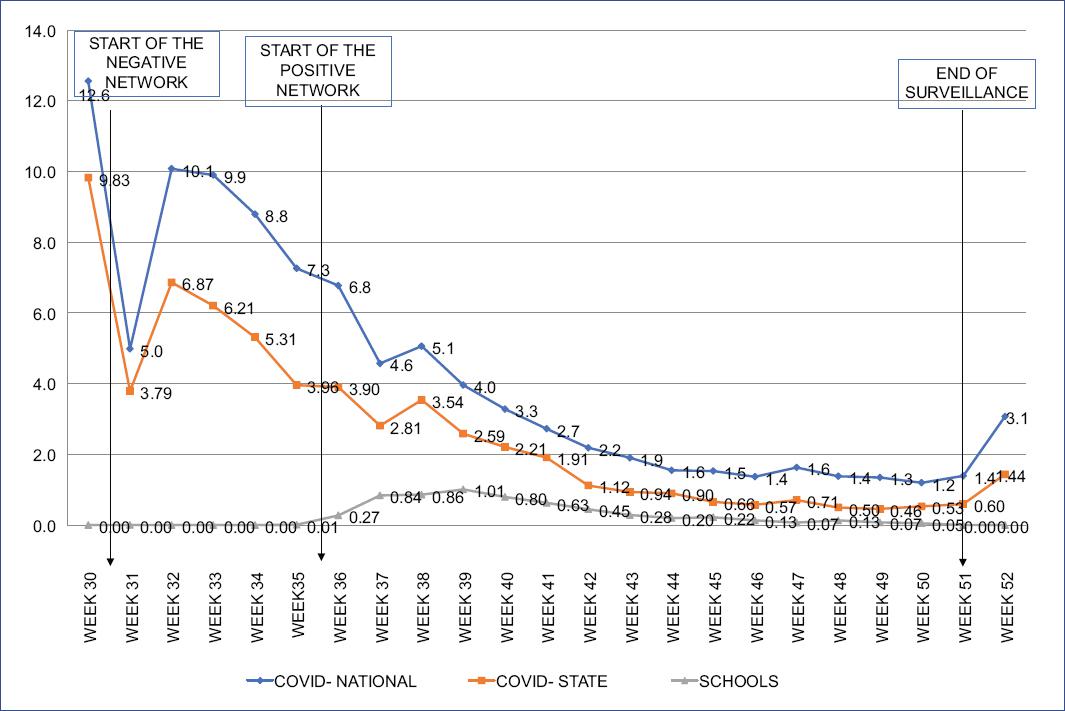
Figure 2 Cases of COVID-19 in children under 18 years in Mexico and the State of Mexico. A comparison of COVID-19 infection rates during epidemiological weeks 31 to 52 is presented. It is important to note that the behavior of the follow-up curve in schools was different from that observed at the national and state levels. The increases did not exceed rate 1.
Mortality
Before returning to school, during the first 30 epidemiological weeks, 8,921 deaths due to COVID-19 were recorded in the state population, with a weekly average of 53.5 deaths. After the return to school, 1,607 deaths were recorded, with a weekly average of 76.5. This resulted in a change in the mortality rate from 52.4 to 9.4 deaths per 100,000 inhabitants in the State of Mexico.
In the cohort studied, of the 3,586 persons with positive SARS-CoV-2 test results, 0.6% (24 persons) required hospitalization due to moderate to severe clinical symptoms of COVID-19. Of these hospitalized patients, nine (37.5%) died, and only one of the deaths was a student (11%). This translates to a mortality rate of 0.02 deaths per 100,000 students in the state during this period, compared to 0.021 deaths in the pre-return to school period (p > 0.5).
A similar pattern was observed for hospitalizations, with a pre-return to school rate of 0.30 per 100,000 students compared to 0.27 after the return to school surveillance period (p > 0.05).
The highest number of cases was recorded during epidemiological week 40, after which a decrease was observed until week 45. When comparing the national and state rates with school rates, the latter was always less than 1, with a linear pattern and a brief plateau during the weeks with the highest number of cases. When the maximum number of cases occurred at both the national and state levels (the outbreaks peak), the negative network strategy proved effective as part of the subsequent containment measures in schools. Comparatively, the behavior of the curves were different. During the monitoring period, 32 (0.16%) schools were closed.
Discussion
The pandemic SARS-CoV-2 infection has had a predominant impact on the adult population14, although it has also affected the pediatric population. One of the main concerns regarding reopening schools was the possibility of an increase in cases in children, with consequent complications, including death21. Schools play a critical role in the functioning of society, and their closure during the SARS-CoV-2 pandemic sparked a global debate. Therefore, the development of strategies that would allow the safe reopening of these institutions became a matter of great urgency at international level. Monitoring by the ISEM shows that implementing timely containment and detection measures and adequate epidemiologic surveillance helps limit the spread of COVID-19 in educational settings.
Our analysis showed an increase in cases in the sixth week after reopening, but these cases did not exceed the increase observed in the community. These findings are consistent with those observed in Canada, where a 0.13 percentage point (95% CI: -0.15, 0.41) increase in COVID-19 cases was also reported in the 30 days following the resumption of face-to-face classes22. This pattern suggests that the increase in positive cases is more pronounced in adult staff than in the student population despite implementing non-pharmacological prevention measures. However, this increase is not considered significant, which is consistent with findings from schools in China23. Through epidemiological surveillance and proper implementation of measures, we are helping to make schools a low-risk environment for disease transmission. A study conducted in Greece suggests that the young population did not contribute significantly to the spreading of the SARS-CoV-2 virus because they tend to have milder symptoms24. However, this conclusion must be treated with caution because children may have risk factors that complicate the disease.
Theoretically, we expected to find more cases in the student population due to their greater interaction with each other compared to teachers and administrative staff. This assumption was confirmed when we observed that the percentage of positive cases among students was up to 20% higher than among teachers and 50% higher than among administrators. A similar situation has been observed in the United States and other countries that have opted to resume face-to-face classes. The researchers found an incidence of 16.1 (95% CI: 14.4 to 17.9) on the first day after schools reopened. However, these cases should be considered community-acquired because of the incubation period. In addition, a 1.3-fold higher incidence of 20.5 (95% CI: 18.5 to 22.5) cases was observed in the 14- to 17-year-old age group on the 20th day after school reopening. In contrast, a lower transmission rate was observed in the group of teachers and administrative staff.
In a study conducted in Israel, conflicting data were observed as a significant school outbreak was recorded only ten days after the resumption of face-to-face activities in educational institutions. This study reported an infection rate of 13.2% in students and 16.6% in staff. In this country, the distancing of students and staff could not be effectively implemented due to a heat wave that coincided with the reopening of schools6. These findings clearly highlight the essential role of community interventions and epidemiologic surveillance in reducing SARS-CoV-2 transmission. They also confirm what we postulated in our study: schools can reopen without a significant increase in community spread if appropriate preventive measures are implemented.
The low case mortality rate among schoolchildren, even in a period when they had not yet received the vaccine, is consistent with that reported in European Union countries and the United Kingdom, where the proportion of hospitalized cases was lower in the age groups of 5 to 11 years and 12 to 18 years (3% and 4%, respectively)25. The situation was different in prisons, orphanages, and nursing homes in the United States, where up to 25% of positive cases were detected within the same community. This underscores the urgency of implementing timely epidemiologic surveillance programs26,27.
Consistent with these findings, low SARS-CoV-2 transmission has been observed in other settings, such as the resumption of social events, as long as disease prevalence remains low and risk reduction strategies are implemented28. The implementation of non-pharmaceutical interventions offers more advantages than disadvantages as long as the strategies are applied consistently and appropriately, ensuring effective infection control. In the case of school reopening, there was no increase in the rate of COVID-19 infection or mortality in the pediatric population.
Finally, although there are uncertainties in our epidemiologic projections, our results are consistent with previous studies that conclude that the implementation of non-pharmaceutical interventions offers more advantages than disadvantages as long as the strategies are applied uniformly and appropriately29. Some questions remain to be evaluated, such as the behavior of prolonged COVID-19 in identified pediatric patients and the impact of vaccination on school dynamics30.
Limitations
Diagnostic testing of the entire school population was not feasible due to the high costs associated with this procedure. Therefore, this study focused only on confirmed cases, which may have resulted in a potential underestimation of the prevalence of SARS-CoV-2, especially in the pediatric population, due to the presence of milder symptoms.











 nova página do texto(beta)
nova página do texto(beta)


