Introduction
Bronchiolitis is the most common viral respiratory infection in children under 2 years of age, followed by community-acquired pneumonia1; up to 30% of children with bronchiolitis have superimposed pneumonia2. The COVID-19 pandemic radically changed the epidemiology of other viral respiratory infections in children. In 2023, Guerrero del Cueto et al. described the incidence of bronchiolitis in the last 12 years and its epidemiologic changes3. These authors observed 2,138 admissions with a diagnosis of bronchiolitis during the 2010-2019 period3. In 2020, hospitalization reduced in 94.4%; however, in the summer of 2021, cases increased for 6 months, reaching a total of 171 cases, with a torpid evolution and requiring admission to the pediatric intensive care unit (PICU), similar to what had been reported by Moreno et al., where admission to the PICU was 9.4%4,5. Another study found that 33.4% of children with bronchiolitis were admitted to the PICU, 44.6% required supplemental oxygen with a conventional nasal cannula, and 10.6% required assisted mechanical ventilation (AMV) but with a low mortality rate6. Therefore, risk stratification of each patient is essential to intensify monitoring and tailor early initiation of ventilatory support. Lung ultrasound is a bedside tool that has proven helpful in early detection of the adverse course of these conditions. Several clinical scales assess these types of conditions, but none of them is accurate7.
Manzur-Sandoval et al. (2021) used the lung ultrasound score (LUS) in adults to predict in-hospital mortality in patients diagnosed with COVID-19; they found that the median score was 19 points, the overall mortality rate was 39.4%, and in cases above 19 points, mortality increased to 50%8.
The LUSBRO scale has been used in children with bronchiolitis. The investigators defined 6 points as a cut-off to indicate greater severity and to predict PICU admission, need for mechanical ventilation, duration of mechanical ventilation, and hospital stay; they reported that 55% of patients were admitted to the PICU, and 6.3% required invasive mechanical ventilation9.
In 2022, the LUS was used to assess 85 pediatric patients with acute respiratory infection (ARI): 5.4% were admitted to the PICU. Moreover, the association between the pediatric early warning score and days of hospital stay and oxygen use was not statistically significant10. However, there is limited literature on this scale in pediatric patients.
This study aimed to evaluate children under 3 years of age with pulmonary pathology of infectious origin using the LUS at the Hospital Infantil del Estado de Sonora (HIES).
Methods
We conducted a descriptive observational study of a consecutive case series of patients under 3 years of age with lower respiratory tract infection. This study was approved by the Research Ethics Committee of the HIES. The study group consisted of patients diagnosed with community-acquired pneumonia and bronchiolitis who were admitted to the Emergency Department of the HIES from January to February 2023.
All patients under 3 years of age admitted to the Emergency Department with a lower respiratory tract infection diagnosed with bronchiolitis and community-acquired pneumonia, according to the American Association of Pediatrics, were included. Bronchiolitis was defined as the first episode of wheezing in a child under 24 months of age, of viral etiology, with expiratory dyspnea and the presence of a catarrhal prodrome11. Community-acquired pneumonia was defined as an acute infection of the pulmonary parenchyma with systemic manifestations, causing acute respiratory symptoms, accompanied by an infiltrate on chest radiography, who had not been hospitalized for at least 1 week or whose symptoms appeared more than 48 h after hospital discharge12.
Neonates with < 37 weeks of gestational age, patients with chronic lung disease (bronchopulmonary dysplasia), bronchial asthma, and congenital heart disease were excluded.
Data were collected within the first 24 h after admission to the emergency department. The clinical score was defined by the Wood-Downes scale modified by Ferres, which was calculated considering the presence of wheezing and subcostal, intercostal, supraclavicular, suprasternal retractions; respiratory frequency and heart rate; symmetric, regular symmetric, or decreased ventilation; and the presence of cyanosis. Patients were graded as follows: mild, with the presence of 1-3 points; moderate, 4-7 points; and severe, 8-14 points13. Oxygen saturation was determined by pulse oximetry.
The etiologic agent was determined by real-time polymerase chain reaction for influenza A (H1N1) PDM09, seasonal influenza A/H3, influenza B, respiratory syncytial virus (RSV), metapneumovirus, adenovirus, and enterovirus. Blood tests and chest radiographs were obtained as part of the routine clinical practice. Respiratory support included invasive and noninvasive ventilation, such as low-flow nasal prongs, continuous positive airway pressure (CPAP), and high-flow nasal cannula. PICU admission was defined as patients requiring invasive mechanical ventilation.
Subsequently, lung ultrasound was performed by a pediatric resident trained in lung ultrasound and supervised by a pediatric intensivist and critical care sonographer during the first 24 h after admission to ED. A Sonoscape S2 portable color Doppler ultrasound unit with a 12 MHz linear probe was used. The lung ultrasound score was assessed using the LUS. Six areas of each lung were examined: anterior (superior and inferior), lateral (superior and inferior), and posterolateral (superior and inferior). Scoring for each area was 0-3 points: 0 points pleural sliding with A-lines and < 2 isolated B-lines per intercostal space; 1 point ≥ 3 isolated B-lines (not coalescing); 2 points: coalescing B-lines (white lung) with or without small subpleural consolidations; 3 points: extensive lung consolidation pattern (small subpleural consolidations are excluded); X lung zone not evaluated (patient could not be mobilized). The total score was the sum of the 12 lung zones assessed. The minimum score was 0 and was considered normal, with a maximum of 36 points14.
Statistycal analysis
Statistical analysis was performed using medians and interquartile ranges for quantitative variables and frequencies and percentages for qualitative variables. In addition, differences in distribution were evaluated using the Students t-test and Fishers exact test. All p-values ≤ 0.05 were considered statistically significant. The analysis was performed with the Statistical Package for Social Sciences version 22 for personal computers.
Results
During the study period, 19 patients with pulmonary pathology of infectious origin were identified, of whom 12 (63.1%) were young infants, four (21.1%) were old infants, and three (15.7%) were preschool children. Ten (52.6%) were males. Bronchiolitis was diagnosed in 14 (73.7%) patients and community-acquired pneumonia in five (26.3%) patients. The median hospital stay was 9 (1-37) days. The WoodDownes scale was moderate in 18 (94.7%) cases. Of the patients, 89.5% were admitted with intercostal retraction; 52.6% had chest radiographs with interstitial infiltrate, 15.8% had unilateral consolidation, and 31.6% had bilateral consolidation. Laboratory tests revealed the presence of RSV in 14 (73.6%) cases, HADV in one case (5.2%), and negative results in four (21%); 12 (63.1%) patients had a positive procalcitonin. The type of ventilatory support on admission to the emergency department was as follows: nine (47.36%) cases with low-flow nasal prongs, seven (36.84%) with invasive mechanical ventilation, two (10.5%) with a high-flow nasal cannula, and one (5.3%) with CPAP; 12 (63.2%) cases required admission to the PICU (Table 1).
Table 1 Clinical characteristics of patients with lower respiratory tract infections in children under 3 years of age, Hospital Infantil del Estado de Sonora
| Variable | n = 19 | % |
|---|---|---|
| Age | ||
| Young infants | 12 | 63.1 |
| Old infants | 4 | 21.1 |
| Preschoolers | 3 | 15.78 |
| Sex | ||
| Male | 10 | 52.6 |
| Female | 9 | 47.4 |
| Disease | ||
| Bronchiolitis | 14 | 73.7 |
| Community-acquired pneumonia | 5 | 26.3 |
| Type of ventilatory support | ||
| Nasal prongs | 5 | 26.3 |
| High flow | 1 | 5.3 |
| CPAP | 1 | 5.3 |
| AMV | 12 | 63.2 |
| PICU | ||
| Yes | 12 | 63.2 |
| No | 7 | 36.8 |
| Chest X-ray | ||
| Interstitial infiltrate | 10 | 52.6 |
| Unilateral consolidation | 3 | 15.8 |
| Bilateral consolidation | 6 | 31.6 |
| Wood-Downes scale | ||
| 4-7 | 18 | 94.7 |
| 8-14 | 1 | 5.3 |
| Intercostal retraction | ||
| Yes | 17 | 89.5 |
| No | 2 | 10.5 |
AMV: assisted mechanical ventilation; CPAP: continuous positive airway pressure; PICU: pediatric intensive care unit.
All patients underwent lung ultrasound and were scored according to the LUS. The median LUS was 7 points, the IOR 25% received a value of 5, the IOR 75% of 8 (range 4-11). According to the analysis, scores ≥ 7 points were considered less severe, and scores of 7 or more points were considered more severe. Of the 19 hospitalized patients, six (31.6%) had a score of 6 or less, of which five (83.3%) received nasal prongs and one (16.7%) required a high-flow nasal cannula (Table 2).
Table 2 Evolution of ventilatory therapy evaluated by LUS in patients under 3 years of age with lower respiratory tract infection, Hospital Infantil del Estado de Sonora
| Patient | Ventilatory therapy on admission | LUS | Days for failure | Rescue ventilatory therapy |
|---|---|---|---|---|
| 1 | Nasal prongs | 9 | 1 | AMV |
| 2 | Nasal prongs | 7 | 1 | AMV |
| 3 | Nasal prongs | 6 | 2 | High flow |
| 4 | Nasal prongs | 5 | 1 | CPAP |
| 5 | High flow | 5 | 1 | AMV |
| 6 | High flow | 8 | 3 | AMV |
| 7 | CPAP | 8 | 3 | AMV |
AMV: assisted mechanical ventilation; CPAP: continuous positive airway pressure; LUS: lung ultrasound score.
Thirteen (53.8%) patients scored ≥ 7 LUS points and required AMV; however, in seven (36.8%) cases, ventilation therapy failed on admission (Fig. 1). In contrast, only one patient (8.3%) required invasive mechanical ventilation on admission with an LUS score of 6 or less, compared to 91.7% with invasive mechanical ventilation and LUS scores > 7 (Fishers´ exact test; p = 0.010). When we analyzed LUS and days of hospital stay of patients, we found that those with ≤ 6 points had a mean length of stay of 5.3 (± 2.3) days, compared to patients with LUS > 7 points in which the mean was 20 (± 13.3) days (p = 0.017).
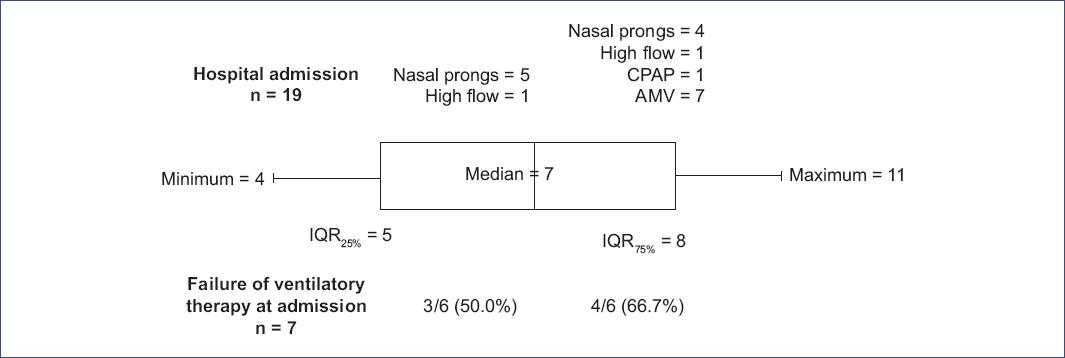
Figure 1 LUS values in 19 children with lower respiratory tract infection and ventilatory management on admission to the Hospital Infantil del Estado de Sonora. AMV: invasive mechanical ventilation; CPAP: continuous positive airway pressure; LUS: lung ultrasound score.
Of the patients admitted to the PICU, 91.7% had a score > 7 points, and 71.4% of the cases not admitted to the PICU had a score of ≤ 6 points, with a statistically significant difference (Fishers exact test; p = 0.010) (Table 3). Mortality occurred in one patient (5.3%) who required mechanical ventilation since admission, with a LUS of 11 points.
Table 3 LUS according to score by severity variables in children with lower respiratory tract infection
| Variable | LUS | p | |||
|---|---|---|---|---|---|
| ≤ 6 points | ≥ 7 points | ||||
| n | % | n | % | ||
| Assisted mechanical ventilation | 0.010* | ||||
| Yes | 1 | 16.7 | 11 | 84.7 | |
| No | 5 | 83.3 | 2 | 15.3 | |
| PICU admission | 0.010 | ||||
| Yes | 1 | 16.7 | 11 | 84.7 | * |
| No | 5 | 83.3 | 2 | 15.3 | |
| IHDS average | 5.3 | ± 2.3 | 20 | ± 13.3 | 0.017† |
*Fisher´s exact test.
†Student´s t-test. IHDS: in-hospital days of stay; LUS: lung ultrasound score; PICU: pediatric intensive care unit.
Discussion
In this study, LUS was found to identify patients with an unfavorable course who required early ventilatory support. Various clinical scales have been proposed to determine the severity of the disease, such as the Downes scale modified by Ferres. However, none of them has shown to identify those patients with an unfavorable outcome7.
The performance of lung ultrasound in these patients represents a diagnostic and staging tool for predicting early ventilatory support and admission to the PICU; performing early interventions by noninvasive ventilatory therapy could improve the patient outcome. Several lung ultrasound scales have been described, such as the LUS for adult patients hospitalized with a diagnosis of COVID-19, the LUSBRO scale for patients with bronchiolitis, and in neonatology, lung ultrasound has been used for the administration of surfactant in premature infants, among other scales in different age groups8,15.
The scale used in this study to analyze pediatric patients with ARI was LUS. The median of the scale was 7 points; it was observed that 91.7% of the patients were admitted to the ICU, similar to what has been reported in other studies. In the study by Bobillo et al. in 2021, they used the LUSBRO scale and found that 55% of the cases admitted to the PICU received ≥ 6 points9.
In this study, high LUS values were significantly associated with the use of invasive ventilatory support; more than half of the cases with ≥ 7 points required this therapy. Bueno et al., in 2019, observed that 2/3 of the patients eventually required AMV; in addition, they presented anteroposterior consolidation in the lung and more than 3 confluent B-lines bilaterally16. In 2021, 59% of adult patients with COVID-19 with LUS ≥ 19 required mechanical ventilation8.
Concerning hospital stay, this study found a correlation between greater lung parenchymal involvement (as observed on lung ultrasound) and more days of hospital stay, as reported in the literature. A study published in 2018 found that for every 5-point increase in the global lung ultrasound score, there was a 1.2-day increase in hospital length of stay, which was statistically significant17.
More than half of the patients with ventilatory failure on admission had a LUS score ≥ 7. Krishna et al., in 202218, found an association between high values of the lung ultrasound USS scale and the type of ventilatory support. The authors observed that 13.2% of patients with posterior subpleural consolidation presented failure of noninvasive ventilatory support (low-flow nasal prongs) and required upper respiratory support, CPAP in 71.4% and 14.2% other methods with a high-flow nasal cannula.
In adult patients with COVID-19, in-hospital mortality was observed to be 50% in patients with LUS score ≥ 19. However, in our study, only one patient obtained the highest score. Mortality correlated with greater parenchymal involvement documented on the LUS, suggesting the need for more aggressive ventilatory therapy upon admission to the ED8.
One situation that needs to be reviewed is the comparison between LUS and chest computed axial tomography (CT), as the results are contradictory in adults. On the one hand, Tung-Chen et al. (2019) described a significant correlation between the results, highlighting a similar accuracy in detecting lung abnormalities19. On the other hand, Colombi et al. (2020) showed that CT performed better than LUS in patients with COVID-19 and that LUS was highly sensitive but not specific20.
Furthermore, studies in pediatric patients have shown that LUS is highly sensitive for detecting normal lung tissue and highly reliable for detecting consolidations. At the same time, CT has a high specificity for excluding pleural effusion and interstitial disease21. Carrard et al. (2022) reported that LUS was superior in diagnosing pneumonia in children with pleural effusion and allowed adequate differentiation of consolidations. However, CT showed better visualization of hydroaerial cavities and atelectasis22. The study by Musolino et al. in 2022 showed that lung ultrasound was better to CT in detecting small subpleural parenchymal consolidations23. However, another study compared the diagnostic performance of LUS and chest CT, and the results were similar. Lung ultrasound was better than chest radiography in identifying consolidations24. However, an important consideration is that chest radiography involves radiation, which increases the risk of developing cancer in children25.
Strengths of the study include the homogeneity of the population studied, which allows for objective ultrasound evaluation in previously healthy lungs. An intensive care physician performed the ultrasound examination. An analysis of the lung regions was performed, allowing a broader assessment of the parenchyma compared to chest radiography. In addition, the portable ultrasound device provided a tool for bedside patient assessment.
Limitations of the study include the sample size, the fact that the interpretation of lung ultrasound is operator-dependent, and that the patients studied were those requiring supplemental oxygen support. Further studies with larger sample sizes and patients with mild respiratory pathology are needed.
In conclusion, this study demonstrated that the use of the LUS in lower respiratory tract infections predicts the need for invasive ventilatory support, PICU admission, and prolonged hospital stay.











 nueva página del texto (beta)
nueva página del texto (beta)


