Introduction
Teenage pregnancy (also referred to as adolescent pregnancy) is one of Mexicos current significant public health issues; nationwide, its prevalence has been estimated around 18.8% in 2010, 19.4% in 2013, and 15.3% in 20211,2. In a retrospective analysis, from 1992 to 2016, other authors found that, although the birth rate for teenage pregnancies for this period was 17.6%, this percentage was exceeded in at least three of the 32 states in Mexico, reaching 19.93%3. The official adolescent pregnancy rate in our state, Nuevo León, in the Northeast of Mexico, was 16.9% in 2010, 15.2% in 2018, and 12.7% in 20211. However, it may be even higher in the lower socio-economical strata and has been a government concern since 2002.
Poverty, discrimination, violence against women, inadequate schooling, difficulty in accessing health services, and poor knowledge about reproductive planning methods have increased the number of unplanned pregnancies during adolescence2,4. In 2015, these factors gave origin to a government strategy , known as ENAPEA (for its Spanish acronym), aimed at diminishing births from teenagers between 10 and 14 years of age and halving by 50% the fecundity rate of those teenagers between 15 and 19 years of age by the year 2030, which is still ongoing5.
Another problem affecting Mexican teenagers is the increase in alcohol, tobacco, and illicit drug use during pregnancy, which, unfortunately, has scarcely been addressed in scientific studies. In 1988, the Mexican General Directorate of Epidemiology and the Mexican Institute of Psychiatry carried out the first National Survey on Addictions. Through a multistage probabilistic sample from 5234 women from the urban population (ages 12-65 years), who reported having ever been pregnant, alcohol consumption during pregnancy was estimated by self-reporting: they found a percentage of consumption between 9.7% and 17.2%, the last figure associated with low-birth weight in the offspring6. However, age-related differences were not explored. A retrospective study in a big metropolitan area, which included 78,871 births from 1991 to 1998, revealed a self-reported prevalence of alcohol consumption during pregnancy of 2.42%, with an apparent increase from 1.97% in 1991 to 2.8% in 19987. Another retrospective, descriptive, and observational study in 2016, which included 608 teenage pregnancies cared for during an 18-month period, reported that 60.2% had consumed alcohol, 53.6% had consumed tobacco, and 1.8% had consumed illicit drugs during pregnancy8. Due to insufficient information on the current prevalence of use of alcohol, tobacco, and illicit substances in the pregnant adolescent population in Mexico, we conceived an observational, prospective, cross-sectional study aimed at determining the self-reported prevalence and calculating relative risks for these exposures in a public third-level hospital in Northeast Mexico. We focused on estimating the prevalence of alcohol use by pregnant adolescents seen at the study hospital and exploring potentially predictive variables for substance use during pregnancy in this population. As a secondary objective, we aimed to establish the prevalence of tobacco and illicit drugs in the same population.
Methods
The study cohort included 420 pregnant adolescents. Inclusion criteria were maternal age between 12 and 18 years, signing the informed consent or assent document, not being currently under legal prosecution, and not having any cognitive or psychiatric limitation that would limit their free will to participate. The study protocol was reviewed and approved by Institutional Review Boards at Escuela de Medicina y Ciencias de la Salud del Instituto Tecnológico y de Estudios Superiores de Monterrey, registered at CONBIOETICA-19-CEI-011-20161017, as well as at the study site. Recruitment was done while the eligible participants were attending the Perinatal High-Risk Clinic for prenatal evaluation (all teenage pregnancies are referred to this clinic by local health policy), and the participants were followed through delivery care until discharge at Hospital Regional Materno-Infantil of the State of Nuevo León in Mexico, from March to August 2018. Upon acceptance, we applied a questionnaire created by the WHO Research and Reporting Project on the Epidemiology of Drug Dependence, further validated by the Comisión Nacional Contra Adicciones, Centro Nacional para la Prevención y Control de las Adicciones and Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz, to all the participants9,10. This instrument has been used in previous surveys in the Mexican adolescent population and was adopted for assessing the use of illicit substances, alcohol, and tobacco consumption. We also collected sociodemographic and anthropometric data, as well as APGAR and Capurro neonatal assessment, and data on the intra-hospital destination of the neonate once he/she was born.
Statistical analysis
We used IBM® SPSS® Statistics v26 for the statistical analysis. The information was initially tabulated in Excel and further imported into SPSS. Continuous variables with normal distribution were expressed as means and standard deviations and analyzed with the t-test. Continuous variables with non-normal distribution were expressed as medians and interquartile ranges (IQR) and analyzed with the Mann-Whitneys U test. Categorical variables were expressed as frequencies and proportions and analyzed with the χ2 test. We explored Kendall´s tau b correlations among a set of independent variables and the dependent outcome variables and for those with a statistically significant association (Supplementary Table 1). Those independent variables with a statistically significant association to any of the main study outcomes and an Event Positive Value >10 in the outcome group with the lowest frequency were included in a binary logistic regression model analysis to obtain the most stable model, as previously published recommendations11,12.
Table 1 Sociodemographic characteristics of the study population of pregnant teenagers
| Characteristics (n = 420) | Median | IQR |
|---|---|---|
| Age (years)* | 17 | 16-18 |
| Sexually active since (years)* | 15 | 14-16 |
| Number of sexual partners* | 1 | 1-2 |
| Age of current partner (years)* | 19 | 18-21 |
| Main occupation | ||
| Housewife† | 376 | 89.4 |
| Student† | 29 | 6.9 |
| Employee† | 7 | 1.7 |
| Independent† | 4 | 1.0 |
| None† | 4 | 1.0 |
| Marital Status | ||
| Unwed† | 320 | 76.2 |
| Single† | 95 | 22.6 |
| Married† | 4 | 1.0 |
| Separated† | 1 | 0.2 |
| Perinatal history | ||
| Molar pregnancy† | 1 | 0.25 |
| Stillbirth† | 4 | 0.95 |
| Born alive, preterm† | 48 | 11.4 |
| Born alive, term† | 370 | 87.4 |
*Values expressed as median and interquartile range.
†Values expressed as frequencies and percentages.
The outcome variables selected for the logistic regression analysis were "Substance consumption during pregnancy," coded as "Yes" or "No"; "Exclusive alcohol consumption during pregnancy," coded as "Yes" or "No", and "Consumption of other substances (except alcohol) during pregnancy," coded as "Yes" or "No." The logistic regression approach was based on the conditional backward method. We considered statistical significance when the p-values of the applied tests were < 0.05, and, for the odds ratios or Exp[β], as long as the corresponding 95% confidence interval (CI) did not contain or cross 1.
A sample of 420 subjects would give our study a power of 90%, with an alpha error of 0.05, to detect a 5% difference with the published prevalence of alcohol use in adolescents in Mexico9. The decision not to attempt an estimation of sample size regarding the prevalence of tobacco and illicit drug use was made since no reliable data were available for these outcomes involving the study population.
The flowchart of the study population is outlined in figure 1. We report results for the group of 420 subjects recruited. Table 1 reports the sociodemographic data of the study participants.
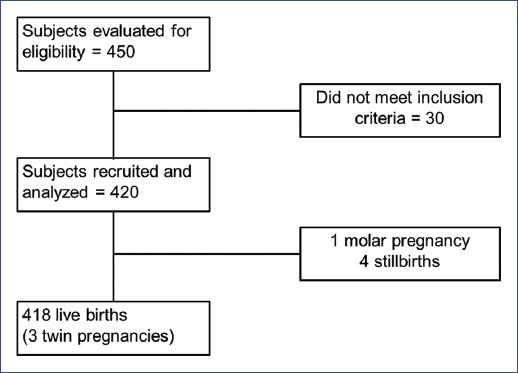
Figure 1 Study flow diagram for prevalence of alcohol, tobacco, and drugs consumption during teenage pregnancy.
Most of the interviewees, 376 (89.5%), reported being dedicated to housekeeping activities; 29 (6.9%) declared being students; 11 (2.7%) were working, and four (1%) reported being unemployed, not working, and not in school. Regarding schooling of 136 participants, almost one-third (32.4%) had completed only grade school; most of our study population, 249 (59.3%) had graduated from high school; 20 (4.8%) had already finished their baccalaureate, 3 (0.7%) had a technical degree, and only 12 (2.9%) reported having dropped-out before finishing primary school. During the year before giving birth, 305 (72.6%) were not attending school, while 115 (27.4%) were still attending school despite being pregnant. A third of the study subjects (142, 33.8%) reported having paid work during the year before giving birth, while the majority (278, 66.2%) did not have paid work during the referred period.
Sexually transmitted infections (STI) occurred in 17 participants during pregnancy, for an overall prevalence of 4%. The most frequently reported STI was human papillomavirus (9 cases, 2.1%), followed by cervicitis and vaginitis (5 cases, 1.2%), and syphilis, HIV infection, and trichomoniasis (one report each, 0.2% each). We did not find any association between the occurrence of STI and the reported number of sexual partners.
Slightly over one-third of the study population (152, 36%) reported living with their partner as a couple, although most of them remained unwed; 126 (30%) were living with a consanguineous relative, while 71 (16.9%) were living with both a consanguineous relative and their partner, and 69 (16.4%) were living with their partner and his family. Only 3 (0.7%) had been relocated to a state-managed refuge.
Table 2 provides a comparative description of the sociodemographic characteristics of participants who self-declared as non-consumers and those who declared themselves as consumers of any substance during pregnancy. The only sociodemographic characteristic that exhibited a statistically significant difference between non-consumers and consumers was the median and range of the number of sexual partners.
Table 2 Comparative of sociodemographic characteristics of the participant pregnant teenagersaccording to substance consumption (n = 420)
| Variables | Non consumers, n = 103 (24.5%) | Consumers, n = 317 (75.5%) | ||
|---|---|---|---|---|
| Age (years)* | 17 | 16-18 | 17 | 16-18 |
| Sexually active since (years)* | 15 | 14-16 | 15 | 14-16 |
| Number of sexual partners* | 1 | 1-1 | 1 | 1-2‡ |
| Age of current partner (years)* | 19 | 17-21 | 19 | 18-22 |
| Main occupation | ||||
| Housewife† | 95 | 92 | 281 | 88.6 |
| Student† | 6 | 6 | 23 | 7.3 |
| Employee† | - | - | 7 | 2.2 |
| Independent† | 2 | 2 | 2 | 0.6 |
| None† | - | - | 4 | 1.3 |
| Marital Status | ||||
| Unwed† | 78 | 76 | 242 | 76.3 |
| Single† | 24 | 23 | 71 | 22.4 |
| Married† | 1 | 1 | 3 | 0.9 |
| Separated† | - | 1 | 0.3 | |
| Perinatal history (418 born alive) | 105 | 100 | 313 | 100 |
| Molar pregnancy† | - | - | 1 | 0.35 |
| Stillbirth† | 1 | 1 | 3 | 0.95 |
| Born alive, preterm† | 16 | 15.2 | 35 | 11.2 |
| Born alive, term† | 88 | 83.8 | 274 | 87.5 |
*Values expressed as median and interquartile range.
†Values expressed as frequencies and percentages.
‡Groups were statistically different, as per Mann-Whitneys U test = 11493.00, Z = −5.124, p = 0.0000003; and Kolmogorov-Smirnov Z test Z = 2.319, p = 0.00004.
Substance use during pregnancy
Overall, 317 (75.5 %) of the 420 participants reported having consumed at least one substance during their pregnancy. As shown in figure 2, 103 (24.5%) participants were not exposed to addictive substances during pregnancy, and of the 317 that self-reported as consumers, 120 (28.6%) participants reported having never consumed alcohol (data not shown). Alcohol, either alone or in combination with other substances, was the most frequently consumed substance (more than two-thirds of the population). Thus, 300 out of 420 participants (71.4%) reported consumption of alcohol during pregnancy, alone or in any combination. According to published definitions applicable to the study population, they may be classified as heavy drinkers13. Of those 300 participants who consumed alcohol during pregnancy, 59 (19.7% of the whole study population) participants may be qualified as binge drinkers. Eight subjects (0.03% of all participants) met the above-mentioned published criteria to be considered heavy drinkers.
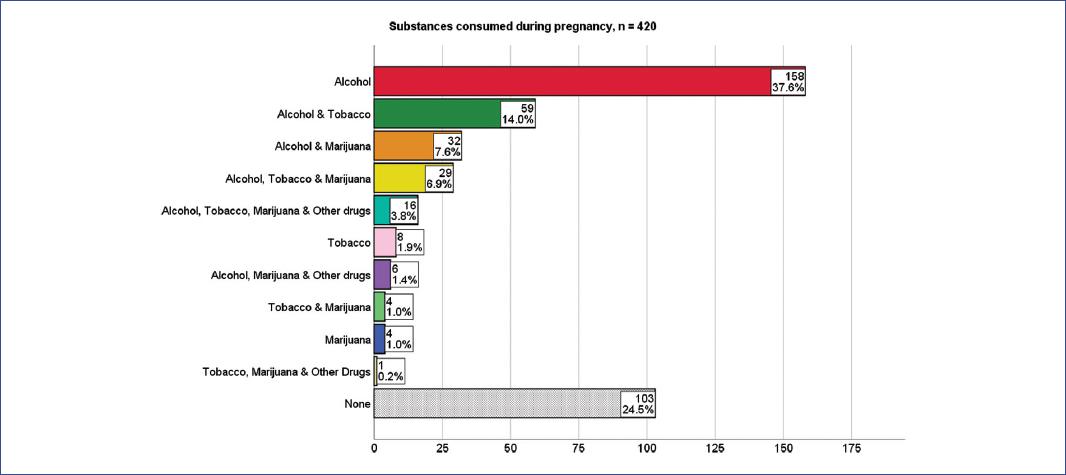
Figure 2 Frequencies and percentages of the different substances consumed during pregnancy in 420 consecutively enrolled pregnant teenagers.
Exclusive alcohol consumption was the third most prevalent outcome (158, 37.6% of the participants), followed by combinations of alcohol with tobacco, alcohol, marijuana, and other drugs (Fig. 2 and Table 3).
Table 3 Bivariate analysis, Pearson´s χ2 with asymptotic two-sided significance, and odds ratio (95% CI) estimation, for independent variables potentially predictive for the specified outcomes, from a study of 420 pregnant adolescents (100%)
| Outcome | Independent variables | χ2 | p-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| Consumers of any substance during pregnancy, n = 317 (75.5%) | Having ever had two or more sexual partners | 22.360 | < 0.001 | 3.420 | 2.02-5.80 |
| Substance use by partner | 9.549 | 0.002 | 2.15 | 1.31-3.51 | |
| Living with someone who smokes | 10.776 | 0.001 | 2.194 | 1.36-3.53 | |
| Exclusive alcohol consumption during pregnancy, n = 158 (37.6%) | Onset of sexual intercourse at 15 years and over | 6.728 | 0.006 | 1.800 | 1.15-2.81 |
| Exclusive alcohol consumption by partner | 7.840 | 0.005 | 2.271 | 1.27-4.06 | |
| Consumption of other substances (except alcohol) during pregnancy, n = 159 (37.9%) | Onset of sexual intercourse at or before 14 years of age | 11.800 | < 0.001 | 2.085 | 1.36-3.18 |
| Having ever had two or more sexual partners | 22.306 | < 0.001 | 2.638 | 1.76-3.96 | |
| Substance use by partner | 22.299 | < 0.001 | 3.547 | 2.05-6.12 | |
| Living with someone who smokes | 16.367 | < 0.001 | 2.279 | 1.52-3.40 |
CI: confidence interval.
The median age at first alcohol ingestion was 15 years (range 10-18 years); the median age at onset of sexual activity was 15 years (range 11-18 years). No differences were found between these variables concerning alcohol consumption.
The exclusive use of tobacco was reported by eight (1.9%) participants, while 117 (27.8%) of the total cohort admitted using tobacco during pregnancy, alone or in diverse combinations with alcohol and drugs. Details on tobacco use alone and tobacco use associated with other substances can be seen in figure 2. The median (IQR) age at first cigarette for the entire cohort who admitted to having ever smoked (n = 255, 60.7%) was 15 (13-15) years) and the median age (IQR) at first cigarette was lower, 14 (13-15) years, in those who continued smoking during pregnancy, (n = 117, 27.8%). However, this difference was not statistically significant.
Exclusive use of marijuana during pregnancy was reported by four subjects (1%), and there were no cases of exclusive use of other drugs not associated with concurrent marijuana use. Marijuana use in combination with another illicit drug was reported by 92 of the 420 participants (21.9%). The different frequencies of marijuana and other illicit drugs during pregnancy are detailed in figure 2. The median age (IQR) of first marijuana use for the entire subcohort who reported this practice was 15 (14-15) years; all marijuana users continued to use marijuana during pregnancy. The most common substance associated with marijuana use was alcohol, followed closely by concurrent use of alcohol, tobacco, and marijuana, and alcohol, tobacco, marijuana, and other drugs. The absolute and relative frequencies of each type of use are detailed in figure 2.
Participants who referred using substances other than alcohol during pregnancy were the second most common group, with 159 (37.9%); this is one of the main outcomes reported in Table 3.
Bivariate analysis and construction of regression models
To investigate the relationship between the main study outcome and independent variables, we conducted a bivariate analysis using χ2, Kendalls tau-b correlation coefficients, and odds ratio estimation with 95% CIs. The results of this analysis are provided in supplementary tables 1 and 2. We performed a binary logistic regression analysis for the three outcomes presented in Table 3 to explore the relationship between the variables further. For the regression analysis, these outcomes were expressed as dichotomous variables. Supplementary table 2 contains the details of the binary logistic regression process.
Briefly, for the outcome "Substance consumption during pregnancy", which was positive in 317 (75.5 %) of the study participants, the intercept model (with no added predictors) correctly identified the outcome in 76.3% of the instances, a minor increase from the previous percentage due to missing data. Among the three potentially predictive variables identified, two remained significant in the model, "Having ever had two or more sexual partners," Exp(β) = 3.173, 95 % C.I. 1.837- 5.482, p < 0.0001, whenever present would increase by 3.2 times the odds of substance consumption in pregnancy; "Living with someone who smokes," Exp(β) = 1.872, 95% C.I. 1.131-3.099, p = 0.015, if present, would increase by 1.9 times the odds of the outcome. Another potentially predictive variable, "Substance use by partner", lost statistical significance in the model, and its 95 % CI for Exp(β) included 1. Thus, it does not contribute to identify the outcome. However, both significant variables in the model have a negligible contribution to further identifying the outcome, so this model is useless in the clinical setting. Perhaps these variables were affected by a collinearity issue.
For the outcome "Exclusive alcohol consumption during pregnancy", the intercept model correctly identified the outcome in 50% of instances. Among the two potentially predictive variables identified, both remained significant in the model: "Onset of sexual life at or above 15 years", Exp(β) = 2.240, 95% CI 1.364-3.678, p = 0.001, whenever present would increase by 2.24 times the odds of the outcome; "Substance use by partner", Exp(β) = 2.861, 95% CI 1.588 to 5.156, p < 0.0001, when present, would increase by 2.9 times the odds of exclusive alcohol consumption during pregnancy. This model also had an acceptable goodness of fit, in accordance with the Hosmer and Lemeshow test. The proposed model would explain at least 10% of the variation in the outcome variable, and it would increase the correct identification of the outcome by 8.9% among pregnant teenagers.
For the outcome "Consumption of other substances (except alcohol) during pregnancy," the intercept model correctly identified the outcome in 50.2% of instances. Among the four potentially predictive variables identified, all remained significant in the model, "Onset of sexual life at or before 14 years", Exp(β) = 1.953, 95% CI 1.172-3.255, p = 0.010, whenever present would increase almost twice the odds of the outcome; "Having ever had two or more sexual partners", Exp(β) = 1.710, 95% CI 1.066-2.744, p = 0.026, when present, would increase by 1.7 times the odds of the outcome; "Substance use by partner," Exp(β) = 2.692, 95% CI 1.466-4.945, p = 0.001, whenever present would increase by almost 2.7 times the odds of the outcome; and "Living with someone who smokes," Exp(β) = 1.620, 95% CI 1.010-2.600, p = 0.046, if present, would increase by 1.6 times the odds of the outcome. This model also had an acceptable goodness of fit, in accordance with the Hosmer and Lemeshow test. The proposed model would explain at least 13.8% of the variation in the outcome variable, and it would increase the correct identification of the outcome by 12%, so it may be useful to identify the consumption of substances other than alcohol during pregnancy in a population akin to ours.
The partners use of alcohol, tobacco, or illicit drugs was documented in 313 cases (74%), while in 103 cases, the partner did not consume any substance (24.3%), and in six cases (1.4%), these data were unknown for various reasons (non-cohabitation, partner not involved). The substances consumed by the partner are detailed in table 4. The most frequently consumed substances among partners was the combination of tobacco and alcohol, followed by exclusive alcohol and, to a lesser extent, tobacco consumption. A statistically significant coefficient of agreement was observed regarding consumption of toxic substances by the study individuals and their partners (kappa = 0.152, p = 0.002).
Table 4 Distribution of the substances consumed by the partners of the pregnant teenagers, (n = 420)
| Substance consumed | Frequency | % |
|---|---|---|
| None* | 103 | 24.5 |
| Tobacco and alcohol* | 147 | 35.0 |
| Alcohol* | 83 | 19.8 |
| Tobacco* | 27 | 6.4 |
| Marijuana* | 12 | 2.9 |
| Tobacco and marijuana* | 5 | 1.2 |
| Tobacco, alcohol, marijuana, and drugs* | 5 | 1.2 |
| Alcohol and marijuana* | 4 | 1.0 |
| Marijuana and drugs* | 3 | 0.7 |
| Tobacco, alcohol, and drugs* | 2 | 0.5 |
| Alcohol, marijuana, and drugs* | 1 | 0.2 |
| Alcohol and drugs* | 1 | 0.2 |
| Unknown* | 6 | 1.4 |
| Total | 420 | 100 |
*Values expressed as frequencies and percentages.
All identified cases of substance exposure during pregnancy were followed by brief intervention and referral to treatment, as recommended14.
Discussion
The main objective of this study was to estimate the prevalence of alcohol consumption during teenage pregnancy in our region. Our findings allowed to identify this behavior as a significant problem since it was reported by 300 out of 420 participants (71.4%). This percentage is higher than we would have expected based on previous estimates. Previous studies have been conducted in the vicinity of our geographic location. In 2008, Galván González et al. conducted a comparative prevalence estimate by directly interviewing 873 participants under the age of 19 who lived in one of two communities on the US-Mexico border. They reported that 15.3% of pregnant adolescents in the Mexican community referred using alcohol, compared with 38.4% of participants in the US county15. Chang et al. surveyed a group of 30 young pregnant women and found that nearly one-third of them self-reported using alcohol during pregnancy16.
Other groups have reported the prevalence of alcohol use during adolescence as a group, and excluding pregnancy status, their prevalence figures are also lower than those found in our study17.
The prevalence found in the present study also exceeds that reported for pregnant young adults in other countries in our continent18,19. It also exceeds the rate of alcohol consumption reported in the general adolescent population in our country8,20-23 and other American countries24.
However, a detailed comparison between the studies mentioned above and our results is not possible due to the heterogeneity in the measurement tools used in the studies.
According to the CDC definition, any amount of alcohol consumption during pregnancy can be considered as excessive drinking13; the same source defines binge drinking for women as consuming four or more drinks in a short period (2 h), while heavy drinking is defined as consuming eight or more drinks per week. Using these measures, our binge drinking rate was 59 out of 300 (19.6%), while 8 of these 300 (0.03%) were classified as heavy drinkers. These figures are similar to those reported for adolescents as a group in both Mexico22,23 and the United States24,25.
It should be noted that comprehensive comparisons of alcohol consumption, binge drinking or heavy drinking rates, tobacco use, or drug use rates between our study and previous reports were beyond the scope of our study.
In our study, risk determinants were assessed for substance use during pregnancy, exclusive alcohol intake during pregnancy, and use of other substances except alcohol during pregnancy. The identified risk factors are detailed in table 3. We did not attempt to screen for risk factors for tobacco or other substances, as these were not our primary objectives, and our study design was not adequately powered for these purposes.
The risk factors that remained significantly associated with the outcome "Substance consumption during pregnancy" in the logistic regression analysis (see Supplementary Tables 1 and 2) may all be related to lack of information about sexuality, promiscuity, poor family support, family tolerance, and peer pressure26,27, the last of which has been previously reported as a risk factor for tobacco use28 but not for alcohol use. This difference may be due to study methodology rather than other reasons.
About "Exclusive alcohol consumption during pregnancy," again, lack of information on sexuality, promiscuity, poor family support, and peer pressure may be involved26,27 as well as family tolerance28.
For the outcome "Consumption of other substances (except alcohol) during pregnancy", promiscuity, lack of information on sexuality, peer pressure, and family tolerance appeared as consistent risk factors, as previously reported in other countries26,27 and in Mexico29.
Regarding tobacco use during pregnancy, our study found a rate of 27.86%, which contrasts with previously reported prevalence rates in Mexico. In an unpaired cases and controls study done in a public hospital in Guadalajara, Jalisco, Mexico, between 2005 and 2006, Ramos Gutiérrez et al. reported a 15.7 % rate of tobacco use among 203 pregnant teenagers30. More recently, in 2016, Blanquet-García et al. reported an almost double prevalence rate for tobacco use in 608 teenage pregnancies, (53.6%)8, while Vazquez-Nava et al., in our same geographical region, reported a prevalence of 21.2% for tobacco use during pregnancy, in 785 cases, similar to our findings31. Factors associated with tobacco use during pregnancy in our study seem to be related to peer pressure and a non-intact family structure26,27,31.
A somewhat more complicated scenario was found concerning illicit drug use during pregnancy. Isolated marijuana use was reported by only four participants (1%), exactly half the frequency of exclusive tobacco use. This low frequency precludes any solid estimation of associated factors.
We should acknowledge that this study had some limitations. First, it was an observational, descriptive, and transversal study and relied mainly on the self-report of pregnant adolescents. Self-report approaches have been criticized, mainly because the epidemiological biases of information, selection, and confusion of participants complicate the documentation of prenatal exposure to illicit substances, tobacco, and alcohol. Moreover, the measurement of the substances or their metabolites in different types of specimens such as urine, meconium, maternal or neonatal hair, cord blood, breast milk, amniotic fluid, or umbilical cord tissue is rarely available and often unreliable due to the characteristics of the specimens or the inaccuracy of the detection techniques32,33. If we had chosen this study model, we would have needed to collect biological samples, thus complicating our work due to regulatory issues. Simultaneously, we emphasize that the survey instrument, equipped with a set of universal screening questions, has been adequately validated in our country. Furthermore, the researchers approach to these young women allowed for adherence to ethical consideration and observance of the principles of beneficence, non-maleficence, justice, and respect for autonomy, in the search for information, followed by a referral to brief intervention, if necessary34. This approach prevented any implicit criminalization of behavior and privileged the possibility of helping those involved. Another limitation was the inability of our study design to discern the burden that sociodemographic issues might have on the observed outcomes.
Based on our findings, self-reported use of alcohol, tobacco, and illicit drugs appears to be increasing in the study population compared with previous data. These findings support the need to establish a mandatory survey to address these exposures and to develop specific strategies aimed at reducing these behaviors. We agree that alcoholism during pregnancy is an underestimated problem in our country35. There is a clear need for more in-depth and analytical studies on this issue, and ideally, establishing a specific health registry strategy would facilitate further and more in-depth research on this issue.
In conclusion, our findings on the prevalence of alcohol, tobacco, and illicit drug use during adolescent pregnancy, assessed with a validated instrument, provide a worrying picture of yet another set of factors adding to the burden of teenage pregnancy. Addressing this issue by the perinatal team should be a clinical care priority.











 nueva página del texto (beta)
nueva página del texto (beta)


