Introduction
Entamoeba histolytica amebiasis, a common cause of gastrointestinal infections in developing countries with a high burden of morbidity and mortality1, affects approximately 40 million people annually, although these estimates are confused with the non-pathogenic agent Entamoeba dispar2. E. histolytica is transmitted through contaminated food or water, with food handlers and mechanical vectors which are potential sources of infection3.
Liver abscess is a severe manifestation of extraintestinal involvement caused by portal dissemination of the pathogen, commonly affecting males aged 18-50 years and rarely children1. Pulmonary involvement is rare and occurs by rupture of the abscess into the pleural cavity4 or by hepatobronchial fistula5, resulting in pleural empyema6,7. This study aimed to report a case of pleural empyema secondary to an amebic liver abscess in a pediatric patient.
Clinical case
We describe the case of a 13-year-old male from Huánuco (jungle region of Peru) who presented to the emergency room with a 4-week history of sharp abdominal pain in the right flank that worsened with physical exertion, decreased appetite, increased fatigue, and fever. In the past 7 days, he referred a productive cough with foul-smelling yellowish sputum, night sweats, fever, and shortness of breath. No diarrhea or changes in stool consistency were reported. He had no previous hospitalizations or surgeries; before hospitalization, he had only received outpatient symptomatic treatment and no antibiotics. He did not report any significant family history. He lives in a rustic two-room mud house with electricity and non-potable water. He breeds domestic animals such as pigs, sheep, and dogs.
On physical examination, he was alert with 28 breaths/min, heart rate 58 beats/min, weight 32.5 kg, temperature 36.7°C, and oxygen saturation 92% with an inspired oxygen fraction of 0.21, requiring supplemental oxygen through a nasal cannula at 2 L. There was no skin or scleral jaundice. The right hemithorax amplexation was decreased, and the vesicular murmur was absent; the right hemithorax also showed dullness to percussion in the lower 2/3 of the right hemithorax. The abdomen was distended with a palpable liver 6 cm below the costal margin with associated dullness; the lower limbs had moderate edema.
Blood tests showed hemoglobin (10.2 g/dL), leukocytosis (24.9 × 103/mm3), neutrophilia (22.1 × 103/mm3), band cells (1.2 × 103/mm3), lymphocytosis (2.4 × 103/mm3), eosinophils (0.0 × 103/mm3), thrombocytosis (457 × 103/mm3), C-reactive protein (250.79 mg/dL), hypoalbuminemia (2.3 g/dL), alkaline phosphatase (601 U/L), aspartate aminotransferase (30 U/L), alanine aminotransferase (44 U/L), lactate dehydrogenase (296 U/L), urea (17 mg/dL), and creatinine (0.38 mg/dL). Bilirubin, coagulation profile, and serum electrolytes were within normal limits. Serologies for hepatitis B, hepatitis C, and human immunodeficiency virus were negative.
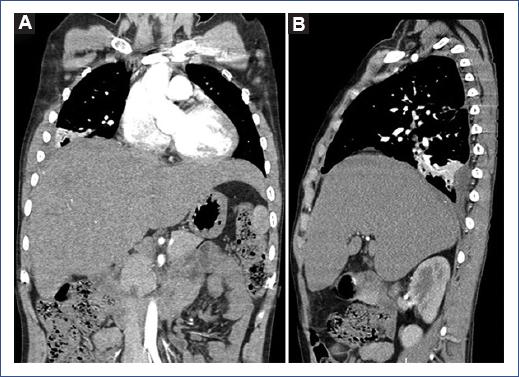
Chest radiography showed complete radiopacity of the right hemithorax with contralateral displacement of the mediastinum. Chest ultrasound showed a heterogeneous encysted accumulation extended over the entire right hemithorax and collapsing the ipsilateral lung. Abdominal ultrasound showed the liver with multiple heterogeneous cystic lesions involving the right lobe without free fluid in the cavity. Thoracic-abdominal tomography showed total right lung atelectasis and massive pleural effusion with a mediastinal shift to the left. In the abdomen, the liver had multiple subdiaphragmatic hepatic collections (the largest measuring 74.3 mm × 82.6 mm × 60.3 mm) with peripheral contrast enhancement in the right hepatic lobe with communication to the right pleural space (Figure 1).
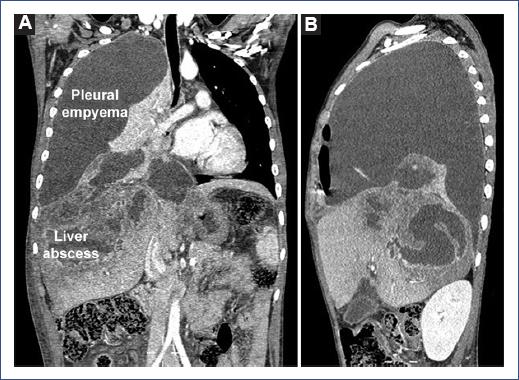
Figure 1 Chest and abdominal tomography. A: coronal plane and B: sagittal plane. Multiple hepatic collections (the largest measuring 74.3 mm × 82.6 mm × 60.3 mm) with diaphragmatic elevation and communication with the right pleural space, associated with hydropneumothorax and total lung collapse.
A chest tube was placed due to the massive right pleural effusion. In addition, 1500 cc of thick, chocolate-colored, and foul-smelling fluid were obtained. The pleural fluid examination showed leukocytes > 100 cells, polymorphonuclear 72%, mononuclear 28%, lactate dehydrogenase 109 U/L, total protein 2.1 g/dL, albumin 0.9 g/dL, and red blood cells 10-12 × C, Gram (−) bacteria. Cultures for aerobic bacteria, amoeba (culture and direct examination), and fungus were performed before antibiotic administration. The results were negative, as was the Western blot for hydatidosis. Anaerobic cultures were not performed. Due to the cystic images in the liver and the housing conditions (rustic house without environmental sanitation), it was decided to test for immunoglobulin G antibodies against E. histolytica by enzyme-linked immunosorbent assay (ELISA) according to the manufacturer's specifications (DRG brand, Germany). The result was positive, reporting 1.82 optical densities suggestive of infection (reference value > 0.30 OD).
The patient received ceftriaxone 100 mg/kg/day and clindamycin 60 mg/kg/day for suspected common organisms. When the serology results for E. histolytica were received 5 days later, intravenous metronidazole 50 mg/kg/day was added. Ceftriaxone, clindamycin, and metronidazole were administered for 28 days. The patient showed symptomatic improvement 7 days after starting antibiotic therapy and chest tube placement (which remained for 21 days); fever peaks persisted until day 10 of hospitalization, and he had a hospital stay of 42 days. Clinical evolution at 2 months follow-up was favorable, with the resolution of the hepatic abscesses and some sub-segmental atelectasis of the right lower lobe (Figure 2).
Discussion
Transudative pleural effusion is common in amoebic liver abscess; however, amoebic pleural empyema is a serious and rare complication in the pediatric population4. This condition occurs when a right lobe liver abscess contiguously invades the diaphragm and produces an empyema or bronchopleural fistula1,8, which may initially lead to a misdiagnosis of complicated pneumonia1.
Clinical manifestations include fever, vomiting, abdominal pain, and distention with respiratory distress due to pulmonary involvement5,9-12, and hemoptysis13-16 and dysenteric diarrhea in some cases6,7,17. The duration of of this condition ranges from weeks to months, especially in patients from an endemic area. In our patient, symptoms developed over 4 weeks; however, shorter periods5,10 of even days9,11 have been reported.
Diagnostic suspicion arises in residents or persons who recently traveled to regions with relevant epidemiology of parasitic diseases associated with clinical manifestations such as fever, abdominal pain5,9,10, or chest pain with dyspnea11,12 when pulmonary involvement is extensive, as in this patient (Figure 1). Imaging studies, such as ultrasound and tomography, demonstrate cystic intrahepatic cavities and pulmonary involvement, and confirmatory tests, such as serology or antigens, support the diagnosis1.
Detection of antibodies against amoebae in serum through ELISA is used to estimate seroprevalence in epidemiologic studies and to diagnose extraintestinal amoebiasis18. However, serologic testing may be limited in differentiating between recent and past infections in highly endemic areas. In addition, negative serology in a patient with a clinical presentation compatible with the disease requires repeating the test 7-10 days later3,18.
Antibodies against E. histolytica are detected in 85-95% of patients with amoebic liver abscess after one or more weeks of symptoms2 and in pleural parenchymal amebiasis at the time of presentation18. Serologic testing for recombinant E. histolytica antigens provides a diagnosis in 96% of cases of amoebic liver abscess before treatment and is negative in approximately 95% of patients 2 weeks after treatment initiation, making it important for diagnosis and monitoring of therapeutic response18.
As stool microscopy is usually negative for extraintestinal amebiasis, such as liver, pleuropulmonary, cardiac, or brain abscesses19, it is not recommended on its own when other diagnostic modalities are available18. Polymerase chain reaction (PCR) testing of E. histolytica DNA in stool, tissue, or abscess aspirates is considered the gold standard for diagnosis of amebiasis; however, high cost and lack of technical experience are important limitations in resource-limited countries3,18.
Our patient came from Huánuco (a jungle region of Peru), where a high frequency of E. histolytica isolation has been reported (26.2%)20. Based on the high prevalence, clinical presentation, and associated imaging data, we suspected pulmonary involvement secondary to a liver abscess of probable amebic etiology, which was confirmed by positive serology for E. histolytica. Neither antigen-based serologic tests nor PCR for E. histolytica were available in our setting.
Treatment of extraintestinal amebiasis consists of a compound such as metronidazole, tinidazole, or nitazoxanide, and an intraluminal agent such as paromomycin or iodoquinol to eradicate intestinal colonization1.
Unfortunately, cases of extraintestinal amebiasis are not diagnosed in the early stages. In these cases, a history of dysenteric diarrhea is not common. As the diagnosis requires a high index of suspicion, treatment in cases of pleural empyema as the initial manifestation is based on broad-spectrum antibiotics directed against common pathogens, as in this patient and other cases9-11. In uncomplicated patients, percutaneous aspiration of the liver abscess is not routinely performed but is justified when associated with clinical deterioration, risk of rupture, or to exclude other diagnoses21. However, in patients with hepatic and pulmonary involvement, thoracic drainage can reduce respiratory distress and improve pulmonary distensibility5,9-12 coupled with drainage of the liver abscess if extensive9,11.
The duration of antibiotic treatment with metronidazole is 7-10 days, with recommended doses of 35-50 mg/kg/day divided every 8 h (maximum dose 750/dose)18. Lack of response to metronidazole after 4-5 days of treatment leads to diagnostic uncertainty and increases the suspicion of an aggregated pyogenic abscess1,3. In our case, as the fever persisted until day 10 after metronidazole, we continued the broad-spectrum antibiotic treatment.
Clinical improvement has been reported between 3 and 6 weeks of follow-up5,10,11. However, there are also reports of fatal cases due to multisystemic involvement and liver failure9,12. In our case, clinical improvement and absence of liver abscesses were observed after 2 months of follow-up.
Pulmonary empyema is a rare complication of amoebic liver abscess with variable outcomes, from fatal to favorable depending on the degree of pulmonary and hepatic involvement.











 nueva página del texto (beta)
nueva página del texto (beta)