Introduction
Congenital pulmonary malformations (CPMs) are heterogeneous disorders that occur during lung development and affect pulmonary airways, parenchyma, or pulmonary vasculature. The most common CPMs are congenital pulmonary airway malformation (CPAM), pulmonary sequestration, congenital lobar emphysema, and bronchogenic cysts1-3.
The estimated incidence of CPMs is 30-42 cases/100,000 population/year, with approximately 10% of cases diagnosed at birth and 14% diagnosed during childhood and adolescence1,4-6.
The clinical presentation varies from severe conditions, such as recurrent bronchopulmonary infections in children, to completely asymptomatic clinical situations in adolescents and adults. The latter are diagnosed incidentally when chest imaging is performed as part of other studies1,5,7.
Diagnostic support techniques during the prenatal period include maternal-fetal ultrasonography. Prenatal magnetic resonance imaging (MRI) is required if the lesions are extensive enough to cause pulmonary hypoplasia. In the postnatal period, regardless of the clinical presentation, a delayed diagnosis requires chest radiography, computed tomography (CT), or MRI, which are useful to confirm and characterize the different CPMs to follow a correct surgical approach7-12.
A few studies on CPMs have been conducted in Latin America5,13,14, but in Peru, no experience in diagnosing and managing this pathology in children has been reported. In the Instituto Nacional de Salud del Niño-Breña (INSN-Breña), the reference center for pediatric pathologies in Peru, diseases of the respiratory system ranked third among the 20 leading causes of hospitalization during the period 2010-2020. In general, congenital malformations were reported in 9.2% of patients, although the frequency of CPMs was not reported15.
Since information on this pathology in children is still limited, this study aimed to describe the clinical, imaging characteristics, and management of patients with CPMs in a pediatric hospital in Peru between 2010 and 2020.
Methods
Design and population
We conducted a descriptive and retrospective study. Data were collected from the medical records of patients diagnosed with CPM at the INSN-Breña in Lima, Peru, between January 2010 and December 2020. The INSN-Breña is an institution of the Peruvian Ministry of Health (MINSA, for its Spanish acronym) that carries out health care and research activities16 and is a national reference center for childhood diseases.
The study population included 70 patients. The diagnosis of CPM was a combination of clinical and imaging findings and anatomopathological confirmation. Patients with CPM diagnosis and who underwent surgery with confirmatory anatomopathological analysis were included in the study. We excluded ten deceased patients with suspected CPM but no anatomopathological confirmation.
Study variables
Clinical variables such as age at diagnosis (months), sex, origin, clinical manifestations, and saturation on admission were described. The imaging variables were chest radiography (focal hyperlucency, focal opacity, and multicystic mass) and tomographic features (parenchymal, mediastinal, and mixed involvement). The type of CPAM was reported according to the classification proposed by Stocker17. The type of CPMs, surgical procedure, post-operative complications, and hospital stay were also described.
A data collection form was used to obtain information from medical records, the hospital imaging database (PACS digitized system), and the anatomic pathology report.
Statistical analysis
For descriptive analysis, numerical variables were summarized as median and range Categorical variables were expressed as absolute and relative frequencies.
The difference between males and females was evaluated for bivariate analysis. The non-parametric MannWhitney U-test was used for continuous variables, and Fisher's exact test for categorical variables, with p < 0.05 considered statistically significant. All analyses were performed with the Statistical Package for the Social Sciences® for Windows version 24 (IBM, Chicago, IL).
Results
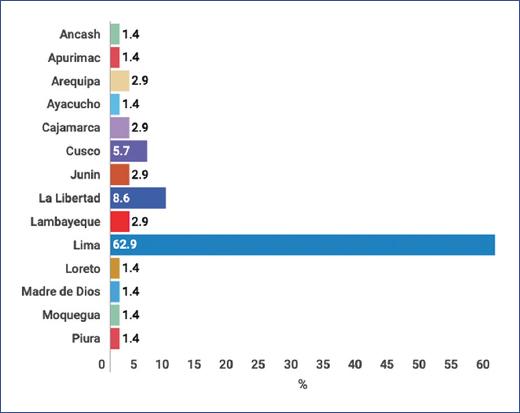
During the study period, 70 cases of CPMs were reported. The median age was 29 months (range 15 days to 14 years), and the male sex was more common with 41 (58.6%) cases. Forty-four (62.9%) patients were from Lima, and the rest were from other departments of Peru (Figure 1).
The most common clinical manifestations were recurrent infections in 28 (40%) cases and respiratory distress in the neonatal period in 19 (27.1%) cases. Twenty-two patients (31.4%) were asymptomatic at diagnosis. On chest radiography, focal hyperlucency was the most common feature (32 [45.7%] cases), and on tomography, parenchymal involvement (50 [71.4%] cases) was observed.
The most common type of CPM was CPAM, with 39 (55.7%) cases, followed by pulmonary sequestration, with 16 (22.9%) cases. Three (4.3%) cases were mixed CPM (case 1: extralobar pulmonary sequestration and type 2 CPAM in the right lower lobe; case 2: intralobar pulmonary sequestration and type 2 CPAM in the left lower lobe; and case 3: intralobar pulmonary sequestration and type 2 CPAM in the left upper lobe) (Table 1). The most common site of CPM was the left lower lobe, with 21 (30%) cases, followed by the right lower lobe, with 20 (28.6%) cases.
Table 1 Clinical and radiological characteristics and location of congenital pulmonary malformations by sex
| Characteristics | Total n = 70 (%) | Males n = 41 (%) | Females n = 29 (%) | p-value |
|---|---|---|---|---|
| Age (months)+ | 29 (0.5-168) | 20 (0.5-168) | 29 (0.8-168) | *0.99 |
| Clinical manifestations | **0.213 | |||
| Asymptomatic | 22 (31.4) | 13 (31.7) | 9 (31.0) | |
| Neonatal respiratory distress | 19 (27.1) | 14 (34.1) | 5 (17.2) | |
| Recurrent infections | 28 (40.0) | 13 (31.7) | 15 (51.7) | |
| Hemoptysis | 1 (1.4) | 1 (2.4) | 0 (0.0) | |
| SatO2 to FiO2 0.21 | 97 (92-99) | 97 (92-99) | 97 (94-99) | *0.912 |
| Chest X-ray | **0.340 | |||
| Focal hyperlucency | 32 (45.7) | 18 (43.9) | 14 (48.3) | |
| Focal opacity | 28 (40.0) | 19 (46.3) | 9 (31.0) | |
| Multicystic mass | 10 (14.3) | 4 (9.8) | 6 (20.6) | |
| Chest CT | **0.018 | |||
| Parenchymal involvement | 50 (71.4) | 26 (63.4) | 24 (82.8) | |
| Mediastinal involvement | 2 (2.9) | 0 (0.0) | 2 (6.9) | |
| Mixed involvement (parenchymal + vascular) | 18 (25.7) | 15 (36.5) | 3 (10.3) | |
| Type of CPM | **0.306 | |||
| CPAM1 | 23 (32.9) | 12 (29.3) | 11 (37.9) | |
| CPAM2 | 12 (17.1) | 7 (17.1) | 5 (17.2) | |
| CPAM3 | 2 (2.9) | 2 (4.9) | 0 (0.0) | |
| CPAM4 | 2 (2.9) | 0 (0.0) | 2 (6.9) | |
| Bronchogenic cyst | 10 (14.3) | 4 (9.8) | 6 (20.7) | |
| CLE | 2 (2.9) | 1 (2.4) | 1 (3.4) | |
| Extralobar PS | 7 (10.0) | 6 (14.6) | 1 (3.4) | |
| Intralobar PS | 9 (12.9) | 7 (17.1) | 2 (6.9) | |
| Mixed CPM | 3 (4.3) | 2 (4.9) | 1 (3.4) | |
| Localization | **0.182 | |||
| RUL | 15 (21.4) | 11 (26.8) | 4 (13.8) | |
| ML | 4 (5.7) | 2 (4.9) | 2 (6.9) | |
| RLL | 20 (28.6) | 9 (22.0) | 11 (37.9) | |
| LUL | 5 (7.1) | 3 (7.3) | 2 (6.9) | |
| LLL | 21 (30.0) | 15 (36.6) | 6 (20.7) | |
| Md | 5 (7.1) | 1 (2.4) | 4 (13.8) |
*MannWhitney U-test.
**Fisher's exact test.
+median (range). CLE: congenital lobar emphysema; CPAM - congenital pulmonary airway malformation; CPM: congenital pulmonary malformation; CT: computed tomography; FiO2: inspired fraction of oxygen; LLL - left lower lobe; LUL, left upper lobe; Md: mediastinum; ML, middle lobe; PS: pulmonary sequestration; RLL, right lower lobe; RUL, right upper lobe; SatO2: oxygen saturation.
Lobectomy was the most common surgical procedure, with 67 (87.1%) cases; pneumonia was the most common post-operative complication, with 9 (12.9%) cases. The median hospital stay was 26 days (range 2-135 days) (Table 2).
Table 2 Surgical management, post-surgical complications, and hospital stay of patients with congenital pulmonary malformations
| Characteristics | Total n = 70 (%) | Males n = 41 (%) | Females n = 29 (%) | p-value |
|---|---|---|---|---|
| Surgical procedure | **0.733 | |||
| Lobectomy | 61 (87.1) | 37 (90.2) | 24 (82.8) | |
| Segmentectomy | 2 (2.9) | 1 (2.4) | 1 (3.4) | |
| Cystectomy | 5 (7.1) | 2 (4.9) | 3 (10.3) | |
| Embolization | 2 (2.9) | 1 (2.4) | 1 (3.4) | |
| Complications | **0.961 | |||
| Pneumonia | 9 (12.9) | 5 (12.2) | 4 (13.8) | |
| Pulmonary abscess | 1 (1.4) | 0 (0) | 1 (3.4) | |
| Pulmonary air leak | 1 (1.4) | 1 (2.4) | 0 (0) | |
| Atelectasis | 4 (5.7) | 3 (7.3) | 1 (3.4) | |
| Pneumothorax | 5 (7.1) | 3 (7.3) | 2 (6.9) | |
| Residual abscess | 2 (2.9) | 1 (2.4) | 1 (3.4) | |
| None | 48 (68.6) | 28 (68.3) | 20 (69.0) | |
| Hospital stay (days)+ | 26 (2-135) | 24 (4-135) | 28 (2-72) | *0.747 |
*MannWhitney U-test.
**Fisher's exact test.
+median (range).
No differences were observed between males and females concerning the variables evaluated (p > 0.05), except for chest CT findings (p = 0.018) (Tables 1 and 2). According to Stoker's classification, type 1 CPAMs were the most common, followed by type 2 CPAMs (Table 3).
Table 3 Frequency of congenital pulmonary malformations studied according to Stocker classification17
| CPAM type | Histological features | n = 39 (%) |
|---|---|---|
| 0 | Involvement of all lung lobes, stillborn | 0 (0.0) |
| 1 | Single or multiple cysts > 2 cm, pseudostratified columnar epithelium | 23 (59.0) |
| 2 | Single or multiple cysts < 2 cm, columnar or cuboidal epithelium | 12 (30.8) |
| 3 | Predominant solid lesions, < 0.5 cm, cuboidal epithelium | 2 (5.1) |
| 4 | Large air-filled cysts, flattened epithelial cells | 2 (5.1) |
CPAM: congenital pulmonary airway malformation.
No patient died during hospitalization, and all were discharged clinically stable.
Discussion
Several theories have attempted to explain the origin of CPMs: defective sprouting of the tracheobronchial tree at 24-36 weeks of gestation, obstruction of the developing bronchus, pulmonary vascular anomalies, and genetic alteration of signaling pathways for lung formation1,7,18.
The most common CPMs are CPAM, bronchopulmonary sequestration, congenital lobar emphysema, and bronchogenic cysts1,3,19,20. After reviewing a series of cases of 11-year-old patients who underwent surgery in our institution, 70 CPMs were identified: 39 (55.7%) cases corresponded to CPAM, 16 (22.9%) to pulmonary sequestration, 10 (14.3%) to bronchogenic cyst, 3 (4.3%) to mixed congenital malformations, and 2 (2.9%) to congenital lobar emphysema.
CPAMs account for about 30-40% of all CPMs. Stocker classified them into five types, with the following proportions: type 0 CPAM < 2%, type 1 CPAM: 60-70%, type 2 CPAM: 15-20%, type 3 CPAM: 5-10%, and type 4 CPAM < 10%17. The proportions found in our study were similar to those reported by Stocker (Table 3).
The clinical manifestations of CPMs are varied; some cause perinatal respiratory failure, which can be very severe, others cause recurrent bronchopulmonary infections in the child, and others may be asymptomatic until adolescence and diagnosed incidentally in the course of other studies1,4,5. In this report, the most common clinical manifestations were recurrent bronchopulmonary infections and neonatal respiratory distress; however, approximately one-third of the patients were asymptomatic.
CPMs are diagnosed based on clinical and imaging findings, and confirmed with pathologic evidence. Frontal and lateral chest radiographs show focal hyperlucency, focal opacities, focal cystic masses, vascular abnormalities, airway abnormalities, or thoracic asymmetry7,8,18. We observed these features in our cases, with focal hyperlucency being the most frequent finding.
High-resolution tomography with multiple 2D and 3D reconstructions provides good-quality images of the airways, lung parenchyma, and vasculature, and the use of contrasting material provides a better approximation of CPM. Because children are radiosensitive, one option is to use MRI, although its ability to evaluate lung parenchymal abnormalities is limited7,10,11,20,21. In this study, the 70 cases underwent chest CT and parenchymal involvement was found in 50 (71.4%) and mixed involvement (parenchymal and vascular) in 18 (25.7%). Due to the lack of equipment for this study in our institution, MRI was not performed.
Other supportive diagnostic tests of CPMs during pregnancy include Doppler ultrasound and MRI; however, some CPMs cases are not detected in the prenatal period due to a lack of suspicion and imaging studies9,11,18,22. In this analysis, only one patient had a prenatal Doppler ultrasound study that suggested CPM as a diagnostic possibility. This patient underwent surgery at 6 months of age, and the diagnosis of extralobar pulmonary sequestration was confirmed; he had a good clinical and radiologic evolution.
The surgical management of CPMs asymptomatic cases is still poorly defined; some studies propose expectant management and surgical intervention when patients develop symptoms, expecting that late surgery may be safer and reduce complications19,20,22-24. In contrast, it is also argued that early intervention at 3 to 6 months could reduce the risk of respiratory infections, hemoptysis, pneumothorax, risk of malignancy and may allow compensatory lung growth5,20,23,24. In our study, half of the patients underwent surgery before one year of age, regardless of symptomatology, and showed adequate evolution during hospitalization.
Symptomatic CPM should be managed surgically; lobectomy is the best treatment to avoid the recurrence of pulmonary infection and risk of malignancy19,20,25,26. As CT is unreliable in delineating the lung lesion from the healthy zone, subtotal lobectomy or segmentectomy could leave remnants of the lesion if only imaging is relied upon. This consideration is important due to the association between CPAM and the development of malignancies such as pleuropulmonary blastoma or bronchioalveolar carcinoma20,26,27. Surgical management of pulmonary sequestration is also recommended to obtain an anatomopathological diagnosis and avoid malignancy risk; however, endovascular management has been reported as a conservative treatment28,29. In these 70 cases, the most frequent surgical procedure was lobectomy, and two patients underwent embolization for pulmonary sequestration.
At present, video-assisted thoracoscopic surgery (VATS) is used by some centers with a complication rate of 12.5% and a conversion rate of 12.5%. This technique reduces the length of hospital stay by up to half and reduces post-operative pain compared to traditional thoracotomy. Therefore, this is the procedure of choice for CPM resection in these centers22,27,30,31. In our study, all cases underwent conventional thoracotomy with a median hospital stay of 26 days; no VATS was performed.
There are few studies on post-operative morbidity and mortality of CPMs; factors to be considered are age at the time of surgery, other associated pulmonary pathologies, the extent of disease, hospital resolution capacity, and surgeon learning curve22,25,31,32,. In our report, the main complications were pneumonia and pneumothorax. Patients with these complications received medical management with favorable clinical evolution.
Our study has certain limitations: the results cannot be extrapolated to the general population because they are based on data from a single institution, and because it is a national reference hospital, an overestimation of cases could be found. In addition, the description of clinical manifestations may be subject to recall bias by family members (mainly in asymptomatic participants) who provided the information described in the medical records. Despite these limitations, this study contributes to the knowledge and description of a rare pathology in children, such as CPMs, with a considerable number of cases compared to other Latin American studies5,13,14.
In INSN-Breña, CPMs were more frequent in males, and recurrent bronchopulmonary infections were their main clinical manifestation. The most common types of CPMs were CPAM and pulmonary sequestration. Lobectomy was the most common surgical procedure, and pneumonia was the main complication during hospitalization.











 nueva página del texto (beta)
nueva página del texto (beta)