Introduction
Child development, also called psychomotor development or neurodevelopment, is a complex process of biological, psychological, and emotional changes resulting from the interaction between genetic and environmental factors1,2. The sequence of child development is usually presented in the form of milestones1. Several screening instruments have been adapted for each country to facilitate the assessment of these milestones in children under five years of age, and are used systematically at key moments of child development3.
The American Academy of Pediatrics recommends universal child development screening through standardized tests (at 9, 18, and 30 months of corrected age), paying particular attention to four and five-year-old children before entering school4. Timely screening for developmental delay allows early interventions so that children can adequately develop their potential5; however, the regular use of screening instruments is often low and less frequent in vulnerable populations and areas with high poverty rates6,7.
In Peru, since 2011, a national health strategy of the Ministry of Health (MINSA) called Norma Técnica de Salud para el Control de Crecimiento y Desarrollo (CRED) de la Niña y el Niño Menor de Cinco Años (Technical Health Standard for the Control of Growth and Development of Children under Five Years of Age) has been implemented)8. However, in 2016, nine impoverished departments in Peru reported inadequate CRED care due to limitations in infrastructure, equipment, materials, management and organizational capacities at the local level, and human resources9.
A study conducted in 2012 at the National Institute of Rehabilitation (Lima, Peru) reported that the two most frequent diagnoses in children < 8 years of age were specific developmental motor function (17.5%; n = 400) and specific mixed developmental (15%; n = 400) disorders. However, milestones or areas of child development were not evaluated, but subjectively assessed the presence of deficits in any function10. Similarly, in 2017, Díaz et al. evaluated the influence of sociodemographic factors on motor and language development in children < 5 years of age in Peru, and reported that those who lived in rural areas or who were children of mothers with low schooling or belonged to households with unsatisfied basic needs showed lower values in the two evaluated areas of child development11.
Unfortunately, these studies did not use an instrument with validity in the Peruvian population and did not evaluate all areas of child development. In addition, few studies in our country have evaluated in depth the characteristics of children who receive care in rehabilitation services, which is essential to understand the needs of rehabilitation teams and to adopt improvement proposals. Therefore, we conducted the present study to evaluate the frequency and characteristics of developmental delay in children < 5 years of age seen at the Pediatric Rehabilitation Service of Edgardo Rebagliati Martins National Hospital (PRS-ERMNH) in Lima, Peru.
Methods
Study design and population
We conducted an analytical cross-sectional study based on information from the medical records of all children < 5 years of age seen at the PRS-ERMNH between April 1 and September 30, 2022. We included those children who did not receive previous care from a physiatrist and excluded those children whose medical records did not present all the variables of interest.
Context
Peru is a country with a shortage of specialized human resources in health (physiatrists, physical therapists, occupational therapists, speech therapists, and psychologists, among others)12 in which there are several health systems, with the largest being the Ministry of Health and the Social Health Insurance (Seguro Social de Salud, EsSalud).
The ERMNH is one of the most important EsSalud national referral centers due to its high specialization and resolution capacity13. It should be noted that all PRS-ERMNH patients were referred from a less complex EsSalud health care center (outside Lima or the Rebagliati Health Care Network) or by inter-consultation with another ERMNH service. At the PRS-ERMNH, during the medical consultation (face-to-face or virtual), all children < 5 years of age undergo a child development evaluation.
Procedures
After ethics committee approval, we requested from PRS-ERMNH the list of all children under five years of age who were evaluated for the first time through a medical consultation (face-to-face or virtual) between April and September 2022. Subsequently, we reviewed each electronic medical record to extract the data of interest to a database in Microsoft Excel.
Evaluation of child development
Child development was evaluated by PRS-ERMNH physiatrists using the Rebagliati Hospital Child Development Assessment Profile (REBA-PED) (Annex 1).
The REBA-PED is a child development screening test, developed and revised by experts in the PRS-ERMNH in 2020. This test is based on an analysis of the instruments used in various countries and has the Peruvian Child Development Assessment Test as its conceptual foundation14.
The REBA-PED was developed through an exhaustive review of seven tests currently used in various countries of the region. Regular meetings were held to select the developmental milestones for each age group, and three important characteristics were considered: ease of use, evaluation based on direct observation or on what parents reported, and objectivity to detect simple, global, or organic delays14.
A pilot study was conducted with two groups of physiatrists who evaluated 100 children to test the reliability of the REBA-PED. In both groups, one person administered the test, and the other observed and scored independently. Inter-rater agreement was found to be high in both groups, with a Kappa of 0.82 in the ERMNH group and 0.84 in the group from the other institution. In addition, the application of the instrument was quick, lasting 5-10 minutes14.
The REBA-PED assesses five areas of child development (gross motor, fine motor, hearing and language, intelligence and learning, and personal-social), showing the degree of delay for each area and the warning signs in child development14.
The gross motor area assesses movement involving the larger muscle groups. The development of movements occurs in a cephalo-caudal pathway, from proximal to distal, which requires the inhibition of primitive neurological reflexes, and the emergence of others. The fine motor area assesses the control of the hand, fingers, and thumb; its development is highly dependent on adequate vision15.
The area of hearing and language assesses the development of verbal (expressive language, comprehensive language, articulation, and prosody) and nonverbal communication. Communication development is highly dependent on adequate hearing. The area of intelligence and learning assesses thinking, reasoning, and problem-solving skills. This area involves other areas such as fine motor or hearing and language15.
The personal-social area assesses the development of independence in a practical sense, personality development, and awareness of separation from others. This area includes feeding, toileting, and dressing abilities, and also the acquisition of social skills that evolve into meaningful relationships15.
The REBA-PED was applied through an interview with the person responsible for the child during the medical consultation (face-to-face or virtual). Delay ≥ 25% (equivalent to 2 standard deviations in similar instruments) was considered a significant developmental delay in any area16. We consider global developmental delay16,17. Delay ≥ 25% in two or more areas was considered as a simple developmental delay was considered as a delay > 0% but < 25% in one or more areas.
Warning signs in child development represent a significant chronological delay in the onset of developmental milestones, and also findings of the persistence of patterns that should have disappeared by a particular age18.
Intervention for developmental delay was deeemed necessary when there was a significant delay, global delay, or any warning sign.
Other variables
Sociodemographic variables such as age (1 to 11 months, 12 to 35 months, 36 to 60 months), sex (male and female), and origin (Lima and other departments) were collected. Clinical variables were also collected, including cause of attendance at the PRS-ERMNH, diagnosis of low weight or short stature, diagnosis of anemia, behavioral problems, associated disease or condition, history, and classification of prematurity (non-premature [gestational age ≥ 37 weeks], extreme or very extreme [< 32 weeks], moderate [32 weeks to 33 weeks with 6 days], and late prematurity [34 weeks to 36 weeks with 6 days]), and prior child development assessments recorded in the electronic medical file (no or yes).
For this study, a behavioral problem was defined as a "behavior of the patient with negative repercussions for him/her (affective) and the environment in which he/she lives (family, school, work, neighbors) for breaking the rules of coexistence"19.
Statistical analysis
We imported the collected data into R software version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria), for conducting all analyses and graphs. Numerical variables presented a non-normal distribution; consequently, we used medians and interquartile ranges (IQR). Categorical variables were presented with absolute and relative frequencies. We evaluated the association between categorical variables using the χ2 test or Fisher’s exact test (according to the expected values) for bivariate analysis. We considered p values < 0.05 as statistically significant.
Results
Between April and September 2022, we identified 226 children < 5 years of age seen for the first time at the PRS-ERMNH: 120 by referral and 106 by inter-consultation. Of these children, seven had a suspected developmental delay as a reason for consultation, and the rest had genetic diseases (20.8%), neurological diseases (15.0%), musculoskeletal disorders (10.6%), autism spectrum disorder (5.3%) and other diseases (10.6%) (Table 1).
Table 1 Characteristics of patients seen for the first time in Pediatric Rehabilitation, (n = 226)
| Characteristic | n (%) |
|---|---|
| Age (months)a | 35.0 (16.3-47.0) |
| Groups of age | |
| 1 to 11 months | 47 (20.8) |
| 12 a 35 months | 68 (30.1) |
| 36 a 60 months | 111 (49.1) |
| Female sex | 129 (57.1) |
| Origin: Lima | 193 (85.4) |
| History of prematurity | |
| Non-premature (≥ 37 weeks) | 183 (81.0) |
| Extreme or very extreme (< 32 weeks) | 13 (5.8) |
| Moderate (32-33 weeks) | 12 (5.3) |
| Late (34-36 weeks) | 18 (8.0) |
| Underweightb | 42 (18.6) |
| Low heightb | 30 (13.3) |
| Anemiac | 26 (11.5) |
| Behavioral problems | 124 (54.9) |
| Associated disease or condition | |
| None | 85 (37.6) |
| Genetic diseases | 47 (20.8) |
| Neurological diseases | 34 (15.0) |
| Musculoskeletal disorders | 24 (10.6) |
| Autism spectrum disorder | 12 (5.3) |
| Other diseases | 24 (10.6) |
| Previous child developmental assessment | 0 (0.0) |
| Type of development delay | |
| No (0% delay in all areas) | 33 (14.6) |
| Simple (delay > 0% but < 25% in one or more areas) | 28 (12.4) |
| Significant (≥ 25% delay in one area) | 44 (19.5) |
| Global (≥ 25% delay in two or more areas) | 121 (53.5) |
| Warning signs of child development | 160 (70.8) |
| Need for intervention due to developmental delay (significant, global or presence of a warning sign). | 178 (78.8) |
| Reason for admission at the PRS-ERMNH | |
| Interconsultation (for prematurity, congenital hypertonia, congenital hypotonia, genetic or neurological disorder) | 106 (46.9) |
| Referral for suspected developmental delay | 7 (3.1) |
| Referral for other reasons (trisomy 21, musculoskeletal disorders, autism spectrum disorder, dyslalia, etc.) | 113 (50.0) |
aMedian (25th percentile - 75th percentile).
bAccording to the World Health Organization’s child growth standards35.
cAccording to the technical norm of the Peruvian Ministry of Health, considering age and sex36.
PRS-ERMNHs: Pediatric Rehabilitation Service of the Edgardo Rebagliati Martins National Hospital.
Of these patients, 49.1% were 3-5 years old, 57.1% were female, 85.4% were from Lima, and 81% were born at term. At the time of the first evaluation, 18.6% were underweight, 13.3% were short, and 11.5% were anemic. None had had a previous child development evaluation recorded in the electronic medical file (Table 1).
According to the child developmental assessment through the REBA-PED, we identified 12.4% of the children with simple developmental delays, 19.5% with significant developmental delays, and 53.5% with global developmental delays. Moreover, 70.8% of the children showed some warning signs. On this basis, we identified that 78.8% of the children needed intervention for developmental delay (Table 1).
We found that more than half of the children evaluated (54.4%) presented significant delay in the area of hearing and language, followed by gross motor (49.1%) and intelligence and learning (45.6%) (Table 2). The medians and distributions of the results in each area are shown in a raincloud diagram (Figure 1).
Table 2 Child development area according to the need for intervention due to developmental delay
| Child development area | Frequency of any delay (> 0%) n (%) | Frequency of significant delays (≥ 25%) n (%) | Percentage of delay median (IQR) |
|---|---|---|---|
| Hearing and language | 153 (67.7) | 123 (54.4) | 31.5 (0.0-63.0) |
| Gross motor | 142 (62.8) | 111 (49.1) | 20.5 (0.0-42.8) |
| Intelligence and learning | 136 (60.2) | 103 (45.6) | 20.0 (0.0-50.0) |
| Fine motor | 143 (63.2) | 100 (44.2) | 18.5 (0.0-49.5) |
| Personal-social | 125 (55.3) | 88 (38.9) | 14.0 (0.0-42.0) |
IQR: interquartile range.
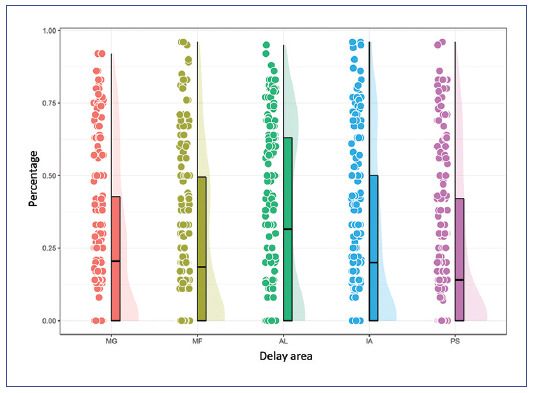
Figure 1 Raincloud plot showing the percentage of developmental delay by area. The bars show the 25th percentile and 75th percentile. The line within the bars shows the median score. The silhouette of each bar represents the number of individuals for each level of delay (percentage). AL: hearing and language; IA: intelligence and learning; MF: fine motor; MG: gross motor; PS: personal-social.
We found a significant correlation of child development among all areas. The strongest correlation (r = 0.82) was found between the fine motor and the intelligence and learning areas, and the weakest (r = 0.49) between the gross motor and the hearing and language areas (Figure 2).
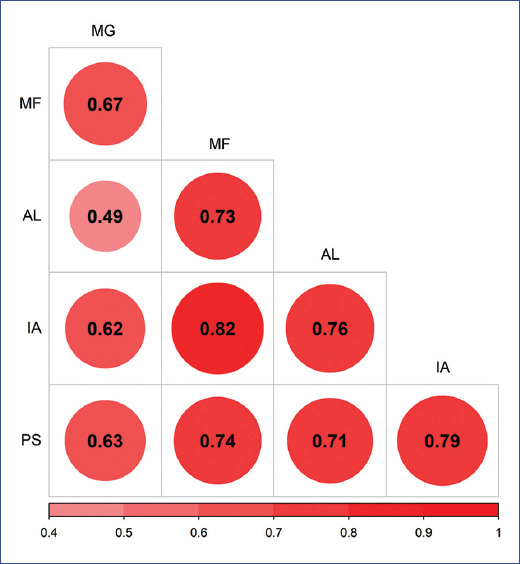
Figure 2 Correlation graph between the areas of child development assessed with the REBA-PED. Note: each point indicates the percentage of delay for each patient, while the central point indicates the median and the straight line the interquartile range. AL: hearing and language; IA: intelligence and learning; MF: fine motor; MG: gross motor; PS: personal-social.
Furthermore, we compared the frequencies of significant delay (≥ 25%) in certain subgroups of interest. We found that the frequency of significant delay in any area, except gross motor, was higher in children > 12 months (p < 0.002) and in those who presented behavioral problems (p < 0.001). The frequency of significant delay in gross motor was higher in females (p = 0.025). The frequency of significant delay in gross motor, hearing and language, and personal-social areas was higher in patients with no history of prematurity. Finally, the frequency of significant delay in any area was higher in patients with genetic diseases or underweight, but it was not associated with short stature in any area (Table 3).
Table 3 Significant delay in child development in each area according to the characteristics of patients seen for the first time in Pediatric Rehabilitation
| Characteristics | Significant delay (≥ 25%) in child development, n (%) | ||||
|---|---|---|---|---|---|
| Gross motor | Fine motor | Hearing and language | Intelligence and learning | Personal- social | |
| Age | |||||
| 1 a 11 months | 19 (40.4) | 7 (14.9) | 5 (10.6) | 11 (23.4) | 4 (8.5) |
| 12 a 35 months | 40 (58.8) | 32 (47.1) | 46 (67.7) | 39 (57.4) | 30 (44.1) |
| 36 a 60 months | 52 (46.9) | 61 (55.0) | 72 (64.9) | 53 (47.8) | 54 (48.7) |
| p value | 0.122 | < 0.001 | < 0.001 | 0.001 | < 0.001 |
| Sex | |||||
| Female | 56 (57.7) | 45 (46.4) | 52 (53.6) | 46 (47.4) | 40 (41.2) |
| Male | 55 (42.6) | 55 (42.6) | 71 (55.0) | 57 (44.2) | 48 (37.2) |
| p value | 0.025 | 0.574 | 0.831 | 0.629 | 0.539 |
| Behavioral problems | |||||
| No | 43 (42.2) | 30 (29.4) | 35 (34.3) | 30 (29.4) | 22 (21.6) |
| Yes | 68 (54.8) | 70 (56.5) | 88 (71.0) | 73 (58.9) | 66 (53.2) |
| p value | 0.058 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Origin | |||||
| Lima | 91 (47.2) | 84 (43.5) | 105 (54.4) | 86 (44.6) | 73 (37.8) |
| Outside Lima | 20 (60.6) | 16 (48.5) | 18 (54.6) | 17 (51.5) | 15 (45.5) |
| p value | 0.153 | 0.596 | 0.988 | 0.458 | 0.406 |
| History of prematurity | |||||
| Non-premature (≥ 37 weeks) | 98 (53.6) | 84 (45.9) | 111 (60.7) | 88 (48.1) | 80 (43.7) |
| Extreme or very extreme (< 32 weeks) | 5 (38.5) | 6 (46.2) | 4 (30.8) | 6 (46.2) | 2 (15.4) |
| Moderate (32-33 weeks) | 4 (33.3) | 5 (41.7) | 4 (33.3) | 3 (25.0) | 3 (25.0) |
| Late (34-36 weeks) | 4 (22.2) | 5 (27.8) | 4 (22.2) | 6 (33.3) | 3 (16.7) |
| p valuea | 0.036 | 0.534 | 0.001 | 0.319 | 0.023 |
| Underweight (current) | |||||
| No | 80 (43.5) | 74 (40.2) | 94 (51.1) | 74 (40.2) | 60 (32.6) |
| Yes | 31 (73.8) | 26 (61.9) | 29 (69.1) | 29 (69.1) | 28 (66.7) |
| p value | < 0.001 | 0.011 | 0.035 | 0.001 | < 0.001 |
| Low height (current) | |||||
| No | 92 (46.9) | 83 (42.4) | 104 (53.1) | 85 (43.4) | 72 (36.7) |
| Yes | 19 (63.3) | 17 (56.7) | 19 (63.3) | 18 (60.0) | 16 (53.3) |
| p value | 0.094 | 0.141 | 0.293 | 0.088 | 0.083 |
| Associated disease or condition | |||||
| None | 29 (34.1) | 31 (36.5) | 38 (44.7) | 29 (34.1) | 23 (27.1) |
| Musculoskeletal disorders | 6 (25.0) | 1 (4.2) | 0 (0.0) | 2 (8.3) | 0 (0.0) |
| Genetic diseases | 40 (85.1) | 39 (83.0) | 41 (87.2) | 36 (76.6) | 34 (72.3) |
| Autism spectrum disorder | 4 (33.3) | 5 (41.7) | 9 (75.0) | 8 (66.7) | 8 (66.7) |
| Neurological diseases | 25 (73.5) | 20 (58.8) | 26 (76.5) | 25 (73.5) | 20 (58.8) |
| Other diseases | 7 (29.2) | 4 (16.7) | 9 (37.5) | 3 (12.5) | 3 (12.5) |
| p valuea | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
a sχ2 test or Fisher’s exact test.
Discussion
We found a high frequency of children who required intervention for developmental delay (19.5% with significant delay, 53.5% with global delay, and 70.8% with some warning sign). Most of the patients studied were female, from Lima, born at term, without malnutrition or anemia, with behavioral problems, and mainly neurological and genetic comorbidities. The behavioral problems and comorbidities, and the fact that ERMNH is a national referral center, may explain this high need for intervention for developmental delay.
No patient had had previous child developmental assessment recorded in the electronic medical file. This deserves to be studied in depth since the universal use of screening tests, especially at the first level of care by health personnel such as pediatricians and physiatrists, is part of CRED care, and their adequate application and recording are essential to guarantee an objective and systematic evaluation in children < 5 years of age8,20,21.
As the present study was conducted during the COVID-19 pandemic, we cannot ignore its possible influence on our findings. Other researchers have shown the possible detrimental effects of social isolation, reduced interaction among children, and lack of access to recreational activities on children’s development and growth22-24. For example, a systematic review involving 21,419 infants (11,438 examined during the pandemic and 9,981 in the pre-pandemic period) reported a higher probability of communication deficits (odds ratio (OR): 1.70; 95% confidence interval (CI), 1.37-2.11) in the pandemic cohort compared to the pre-pandemic cohort.25 Similarly, a study in China reported that the COVID-19 pandemic might be associated with an increased risk of delayed fine motor (OR: 2.50; 95% CI, 1.25-4.99) and language development (absolute risk difference (RRa): 1.13; 95% CI, 1.02-1.25) in 1-year-old children26. In Peru, due to its precarious health system and controversial political decisions, an aggressive and prolonged quarantine was applied in contrast to other countries27,28, which may have had a relevant impact on child development in our population since most of them were > 3 years. This could explain, at least in part, the high frequency of delay in the area of hearing and language.
Furthermore, the fact that the area of hearing and language was the most affected suggests the of having many speech therapists in the PRS-ERMNH, and cohorts and experimental studies, to understand the outcomes of these patients and the efficacy of interventions.
A strong correlation was observed between the delay percentages in certain areas of child development (e.g., fine motor and intelligence and learning). This correlation was expected since impairment or progress in one area is related to the others. Hence, the importance of assessing not only one area or milestone at a time but the sequence of milestone acquisition in all areas of child development2,20.
The frequency of significant delay in the gross motor area was not higher in children > 12 months than those aged 0-12 months, in contrast to what was found in all other areas of child development. This observation could be related to previous studies reporting that the prevalence of delay in the gross motor area decreases with age29,30.
The frequency of significant delay in most areas of child development was higher in children with behavioral problems. This finding is consistent with previous studies in which children with developmental delay are three to four times more likely to have behavioral problems than children without developmental delay31,32. In addition, many behavioral problems are part of diseases or conditions associated with global developmental delay, such as autism spectrum disorder, attention deficit hyperactivity disorder, and anxiety disorder, among others33.
Finally, the frequency of significant delay in any area of child development was higher in patients with genetic diseases or underweight. This finding is consistent with previous studies in which 30-50% of cases of global developmental delay are of genetic etiology17,33 and significant developmental delay is associated with a higher prevalence of exposure to indicators of malnutrition (underweight, wasting, and stunting) in middle- and low-income countries similar to Peru34.
Limitations and strengths
This study has some limitations: 1) Child development was evaluated using the REBA-PED instrument proposed for the Peruvian and Latin American context14. However, like the instruments used in other countries in the region, it has yet to be validated in long-term cohorts or compared with a comprehensive reference test. Therefore, future studies are necessary to validate these instruments in different contexts.
2) As this study was conducted based on clinical record review, it was not possible to assess the adequacy of data recording. However, the care of each patient was performed by a physiatrist.
This is one of the first Peruvian studies that has evaluated in depth the characteristics of children receiving care in rehabilitation services. Moreover, to our knowledge, this is the first study to address this topic after the COVID-19 pandemic, which provides relevant information to understand the needs of rehabilitation teams and to make proposals for improvement.
In conclusion, a high frequency of developmental delay was found among the children evaluated, with a predominance in the area of hearing and language. Although all children were referred from the first or second level of care, none had a previous child development assessment recorded in the electronic medical file. Future studies should further evaluate and explore whether child development is being assessed objectively and systematically at different levels of health care.
Supplementary data
Supplementary data are available at Boletín Médico del Hospital Infantil de México online (10.24875/BMHIM.23000026). These data are provided by the corresponding author and published online for the benefit of the reader. The contents of supplementary data are the sole responsibility of the authors.











 nueva página del texto (beta)
nueva página del texto (beta)


