Introduction
Currently, most experts studying the pancreas in the pediatric age group are relatively conservative in searching for a cause when dealing with a single episode of acute pancreatitis (AP)1; however, a detailed investigation is advised in cases of acute recurrent pancreatitis (ARP) or chronic pancreatitis (CP)2. Because PAR and CP are relatively rare in the pediatric population, few studies provide data regarding these conditions3.
Patients with ARP are considered to be at risk of developing CP over time. Although the diagnostic criteria are different, it is recognized that they share common etiologies4. The pathophysiology of recurrent episodes probably resembles that present in patients who experience a single episode; however, these patients may have additional genetic factors that increase the likelihood of developing ARP5-7. The following criteria must be met to establish the diagnosis of ARP2:
At least two different episodes of AP:
- Presenting complete resolution of pain between both events, with a minimum of 1-month duration between events or
- Complete normalization of serum pancreatic enzyme levels before the next AP event and complete resolution of pain symptoms, regardless of the time interval between the two episodes.
Furthermore, CP consists of an inflammatory process characterized by irreversible morphological changes, with fibrotic replacement of the pancreatic parenchyma resulting from repetitive or long-lasting inflammatory processes. Current theory suggests that CP begins with an AP condition that progresses to fibrosis, resulting from a continuous destructive process in susceptible individuals influenced by environmental and modifiers factors2,8. Many of these patients have a history of ARP prior to irreversible changes in pancreatic anatomy and function; however, some may present with diagnostic features of CP without having had a prior diagnosis of ARP. Since making a histopathologic diagnosis of CP at the pediatric age is uncommon, clinical criteria are considered more pragmatic in defining this condition. CP requires for diagnosis at least one of the following criteria2:
- Abdominal pain that suggests pancreatic origin associated with imaging findings suggestive of chronic pancreatic damage (irreversible structural changes such as focal or diffuse parenchymal destruction, sclerosis, and ductal abnormalities).
- Evidence of exocrine pancreatic insufficiency plus findings suggestive of chronic pancreatic damage.
- Evidence of endocrine pancreatic insufficiency plus findings suggestive of chronic damage.
As reported by the INSPPIRE consortium, children with ARP have more findings compatible with AP, i.e., inflammatory changes, edema, necrosis, and peri-pancreatic inflammation. In contrast, patients with CP present with persistent pancreatic lesions such as atrophy, irregular contour, heterogeneous texture, calcifications, irregularities, and defects of intraductal filling, calculi, strictures, or dilatations9.
Although the disorders associated with these forms of pancreatitis are divided into several categories for study, the prevalence of these causes varies significantly among different studies. This appears to result from the inherent limitations of retrospective studies, the bias or experience of physicians caring for children with pancreatitis, incomplete investigations about causes, the greater number of patients recognized as having pancreatitis, and the recognition of new etiologies in childhood6. In a cross-sectional study conducted by the INSPPIRE group that included 155 patients diagnosed with ARP and 146 with CP, associated risk factors were sought. The risk factors were divided into four categories: genetic, obstructive, toxic/metabolic, and autoimmune. At least one risk factor was identified in 72% of patients with ARP and 86% of patients with CP. The authors reported that the most common risk factors for the development of ARP or CP were genetic and obstructive9.
As in patients who experience a single episode of pancreatitis, many with ARP have no identifiable cause for their disease. Because of this, they are recognized as having an idiopathic cause6. In addition, children with ARP or CP are often considered to have multiple risk factors. For example, in a study conducted by the INSPPIRE group, multiple risk factors of different categories were identified in 30% of patients with ARP and 27% of patients with PC, demonstrating the multifactorial nature of these conditions9.
Pediatric patients with recurrent pancreatitis should be evaluated at least annually to identify early the development of pancreatic insufficiency. In the case of patients with CP, the recommendation is that they should be evaluated annually for both exocrine and endocrine pancreatic insufficiency4. The time course for transition to exocrine or endocrine failure is not clearly established. The timing of exocrine failure on the CP timeline spectrum is not fully known. The exocrine function may decline even before imaging findings are evident and thus may be a marker of disease changes10.
Examining and analyzing a population of Mexican pediatric patients with rare conditions such as ARP or CP allows us to generate greater knowledge and provide relevant information. For this reason, this study aimed to describe the clinical and paraclinical profiles, and related etiologies of patients with ARP and CP treated at a tertiary care institution in Mexico.
Methods
We conducted an analytical and retrospective cross-sectional study of the records of pediatric patients seen at the Hospital Infantil de México Federico Gómez with a diagnosis of ARP and CP from 2010 to 2020. Following the cross-sectional observational study protocol, the STROBE checklist was used. Patients without a complete clinical record, imaging studies, or a history of pancreatic-biliary surgery prior to diagnosis were excluded from the study.
A targeted search was performed in the clinical archive of the institute under the search code "K86.1", corresponding to the diagnoses "recurrent pancreatitis", "repetitive pancreatitis," and "chronic pancreatitis". In addition, an electronic tool (PRC-2021) was created for data collection that covered the most relevant aspects of each individual: demographic, clinical, and radiological. All imaging studies used in the diagnosis and follow-up of patients were intentionally sought, mainly for findings suggestive of chronic pancreatitis. Furthermore, a search was made of the associated etiologies and diagnostic tests used in each case, which were classified as genetic, anatomical, metabolic, or autoimmune. Once the database was obtained, patients were grouped by diagnosis (ARP vs. CP) and by the age of onset (early vs. late), with a cut-off point at six years. Finally, complications such as exocrine or endocrine pancreatic insufficiency were analyzed in each patient.
Statistical analysis
A descriptive analysis of participant characteristics was performed using frequencies for dichotomous variables and medians, minimums, and maximums for quantitative variables. Tests of medians for quantitative variables and Fisher's exact test for nominal variables were performed to identify differences according to the type of diagnosis (ARP vs. CP) and age of presentation (early vs. late). A statistical significance level of p < 0.05 was considered. The SPSS V27 program was used for the analysis.
Ethical considerations
The present study was considered a risk-free research as it was a retrospective documentary research in which no intervention or intentional modification of the variables of the study's participants would be performed. Therefore, no letter of informed consent was requested. The confidentiality of the data and the anonymity of the participants were maintained.
Results
A population of 25 patients, who met the INSPPIRE diagnostic criteria were studied. The age range was between 5 and 24 years, according to the date of the last hospital visit. The distribution was similar between genders. The number of patients with ARP was 17 (68%) compared to CP, with eight patients reported (32%) (Table 1). All patients presented abdominal pain; in more than half of the cases, vomiting was reported as an associated symptom, followed by nausea, anorexia, and abdominal distension. In 64% of the patients, placement of a pancreatic prosthesis was required as a temporary measure to manage the inflammatory process and to evaluate the evolution of the clinical picture. This measure was carried out to observe if the patient presented a complete resolution of symptoms or if surgical treatment needed to be considered after 24 months of follow-up.
Table 1 General characteristics of the participants (n = 25)
| Median | (min-max) | |
|---|---|---|
| Age (years) | 14 | (5-24) |
| Time of evolution (years) | 6 | |
| n | (%) | |
| Sex | ||
| Male | 12 | (48) |
| Female | 13 | (52) |
| Diagnosis | ||
| Acute recurrent pancreatitis | 17 | (68) |
| Chronic pancreatitis | 8 | (32) |
| Early onset (< 6 years) | 9 | (36) |
| Symptoms reported in acute events | ||
| Abdominal pain | 25 | (100) |
| Nausea | 7 | (28) |
| Vomiting | 16 | (64) |
| Anorexia | 2 | (8) |
| Abdominal distention | 4 | (4) |
| Other | 6 | (24) |
| Etiology | ||
| Genetic | 1 | (4) |
| Pancreatic duct alterations | 8 | (32) |
| Biliary tract anatomical alterations | 3 | (12) |
| Metabolic/Toxic | 3 | (12) |
| Cause not identified | 12 | (48) |
| Treatment | ||
| Pancreatic prosthesis | 7 | (28) |
| Surgical | 9 | (36) |
| Complications | ||
| Exocrine pancreatic insufficiency | 2 | (8) |
| Secondary diabetes mellitus | 1 | (4) |
Twelve percent of the study universe developed exocrine or endocrine pancreatic insufficiency. The main etiology identified corresponded to anatomical alterations of the pancreatic duct (32%); however, in 48%, the etiology could not be identified. Pancreas divisum was the most prevalent condition (Figure 1). Concerning genetic causes, only two patients were screened for associated mutations. Only one case of ARP was identified with the CFRT gene mutation. In three patients, serum IgG4 levels were requested to indicate autoimmune disease, reporting levels within normal ranges. In one adolescent patient, a fine needle pancreatic biopsy guided by endoscopic ultrasound was performed, reporting the histopathological study as an inconclusive sample; no case of autoimmune pancreatitis could be documented. Metabolic/toxic causes were reported in 3/25 patients, two of them with the presence of hyperlipidemia, and one case associated with L-asparaginase.

Figure 1 Endoscopic retrograde cholangiopancreatography (ERCP). The image shows a pancreas divisum, the course of the duct of Santorini continues with the dorsal duct. In the ventral portion of the pancreas a small duct of Wirsung is observed.
The most frequent finding in the imaging studies of the group with CP was the presence of calcifications and pancreatic ductal dilatation (Figures 2 and 3). In patients with ARP, ductal dilatation and pancreas with a heterogeneous pattern were frequently reported.
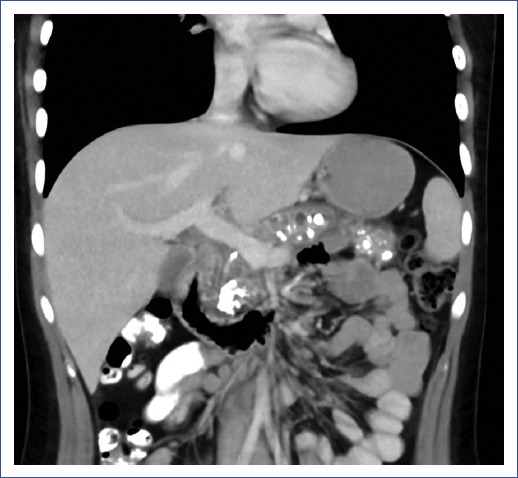
Figure 2 Chronic pancreatitis with calcifications. The CT image shows an enlarged pancreas, heterogeneous parenchyma, with multiple calcifications, poorly demarcated borders, and loss of peri-pancreatic fat.

Figure 3 Ductal dilatation in chronic pancreatitis. In the image obtained by magnetic resonance cholangiopancreatography a dilated pancreatic duct of up to 10 mm is observed (asterisk), in addition there are areas of absence of signal in relation to a calculus (arrow).
No differences were identified in the clinical picture, treatment received, or complications (Table 2). In contrast, when comparing groups by the age of onset, there was a higher frequency of pancreatic prosthesis placement in the late-onset pancreatitis group compared to the early form. No other differences were identified between the groups (Table 3).
Table 2 Differences between the participants according to diagnosis
| Acute recurrent (n = 17) | Chronic (n = 8) | p* | |
|---|---|---|---|
| Age (years)a | 13 | 16 | 0.031 |
| Time of evolution (years)a | 5 | 8.5 | 0.194 |
| Episodes of pancreatitisa | 4 | 4 | 0.549 |
| Male sexb | 9 | 3 | 0.673 |
| Early onset (< 6 years)b | 8 | 1 | 0.182 |
| Image findingsb | |||
| Pancreatic atrophy | 0 | 2 | 0.093 |
| Calcifications | 0 | 6 | < 0.001 |
| Heterogeneous pattern | 3 | 5 | 0.061 |
| Ductal obstruction or stenosis | 0 | 1 | 0.320 |
| Pancreatic ductal dilation | 5 | 8 | 0.002 |
| Etiologyb | |||
| Genetics | 1 | 0 | |
| Pancreatic duct alterations | 3 | 5 | 0.061 |
| Biliary tract anatomical | |||
| alterations | 3 | 0 | 0.527 |
| Metabolic/Toxic | 2 | 1 | 1.000 |
| Cause not identified | 8 | 3 | 0.673 |
| Treatmentb | |||
| Pancreatic prosthesis | 5 | 2 | 1.000 |
| Surgical | 4 | 5 | 0.087 |
| Complicationsb | |||
| Exocrine pancreatic | 0 | 2 | 0.093 |
| insufficiency | |||
| Secondary diabetes mellitus | 0 | 1 | 0.320 |
aDifference of medians.
bFisher's exact test.
Table 3 Differences of participants according to age of onset
| Late-onset (n = 16) | Early-onset (n = 9) | p* | |
|---|---|---|---|
| Age (years)a | 15 | 9 | 0.500 |
| Time of evolution (years)a | 6 | 5 | 0.250 |
| Episodes of pancreatitisa | 4.5 | 4 | 0.250 |
| Male sexb | 7 | 5 | 0.688 |
| Diagnosisb | |||
| Acute recurrent | |||
| pancreatitis | 9 | 8 | 0.18 |
| Chronic pancreatitis | 7 | 1 | 2 |
| Etiologyb | |||
| Genetic | 1 | 0 | 0.661 |
| Pancreatic duct alteration | 6 | 2 | 0.530 |
| Biliary tract alteration | 1 | 2 | 1.000 |
| Metabolic/Toxic | 2 | 1 | 1.000 |
| Cause not identified | 7 | 4 | |
| Treatmentb | |||
| Pancreatic prosthesis | 7 | 0 | 0.027 |
| Surgical | 5 | 4 | 0.671 |
| Complicationsb | |||
| Exocrine pancreatic insufficiency | 1 | 1 | 1.000 |
| Secondary diabetes mellitus | 1 | 0 | 1.000 |
aDifference of medians.
bFisher's exact test.
Discussion
ARP and CP are relatively rare in children; however, these conditions have been recognized more frequently in recent years. Reporting our institution's experience with this nosologic condition is useful to evaluate the current disease landscape in our country. Our results show similarities to those reported by the INSPPIRE group. An earlier presentation of the disease was observed in the ARP group compared to children with CP, similar to that reported by Kumar et al.9, suggesting the relationship and continuity of the disease between both conditions.
The INSPPIRE group consensus published by Gariepy et al3. noted that a large proportion of patients with these disorders had one or more underlying causes, suggesting the multifactorial nature of these diseases. This could not be observed in our study due to the limitations of the etiological approach, identifying only three cases with more than one associated causal factor.
In our series, a complete etiological approach was not performed in all patients; for example, it is noticeable the lack of identification of genetic alterations. However, we performed a complete anatomical study on all participants, including highly specialized studies such as magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography. In our study, anatomical alterations of the pancreatic duct were the etiological group most frequently found, with the pancreas divisum standing out among them. These data are similar to those reported in the large cohorts of the INSPPIRE group, such as those reported by Kumar et al.9 and Wejnarska et al.11, with up to 30% of their population presenting these anatomical alterations.
At present, the impact of genetic mutations as a risk factor for the development of ARP and CP is quite underestimated, as reported by Randall et al.12 In our population, a genetic study was performed in only two patients, identifying the CFRT gene mutation in only one. This condition is of great relevance and corresponds to an area of opportunity for improvement in the management of these patients since a severe course of pancreatitis has been found to be mostly related to patients with these mutations13. Even an earlier progression to the chronicity of these conditions has been associated with genetic mutations, as Abu-El-Haija et al. reported in their cohort of patients with chronic pancreatitis10,14. With imaging studies, we identified a higher frequency of calcifications and ductal obstruction in patients with CP than in those with ARP. Other authors have reported these changes with reports of persistent pancreatic lesion changes in CP (atrophy, calcifications, and ductal irregularities)9.
Autoimmune pancreatitis is currently recognized as a rare cause of recurrent pancreatitis in the pediatric age group. Large cohorts of patients have reported its presence in 3.9-15% of the population studied13,15. In our study, autoimmune pancreatitis was not reported, although we cannot rule it out reliably, given the complex workup required for establishing this etiology16,17.
The main limitation we face when we want to have a complete study of these patients in whom autoimmunity is suspected is the absence of pancreatic tissue to perform immunohistochemistry. Therefore, obtaining a histological sample with a fine needle guided by endoscopic ultrasound would be the most appropriate method as it is considered the least invasive procedure.
Despite the limitations in the diagnostic approach in our population, we did not identify differences in etiology between the early-onset and late-onset groups. This also agrees with that reported by other authors, who found no significant differences in the distribution of etiological factors according to the age of onset of the disease12.
In conclusion, the main etiology of ARP and CP identified in our study corresponds to anatomical alterations of the pancreatic duct; however, in almost half of the cases, there was no established cause. Patients with CP have more findings in imaging studies related to calcifications and pancreatic ductal dilatation; however, the risk factors associated with progression to ARP or CP, early or late presentations of the disease are not clear.
Although comparing our results with those offered by the large cohorts of the INSPPIRE group is complicated, we found relevant similarities. The data in this descriptive study provide the precedent and the basis for future research in the field of pediatric pancreatology in the Mexican population. This study allows to propose a comprehensive assessment of these patients by geneticists, pediatric surgeons, nutritionists, endocrinologists, and gastroenterologists to direct efforts on a better etiological diagnosis, follow-up, and timely medical or surgical treatment to avoid sequelae in the endocrine or exocrine pancreatic function.











 nueva página del texto (beta)
nueva página del texto (beta)


