Introduction
Rhabdoid tumor, one of the most aggressive and lethal neoplasms in the pediatric population, mainly affects children under 3 years of age and is usually located in the kidney.
Although its localization outside the kidney is rare, a presentation called an atypical rhabdoid teratoid tumor is found in the central nervous system.
Other atypical locations have been described, such as the head, neck, thorax, mediastinum, liver, ileum, genitourinary tract, and retroperitoneum1. Most tumors contain biallelic somatic inactivation with mutations found in the SMARCB1 gene, located on chromosome 22q11.2. Under normal conditions, this gene controls cell growth, division, and death; one copy is inherited from the mother and one from the father. However, the cells of patients with rhabdoid tumor predisposition syndrome carry one functional copy of SMARCB1 and one altered copy. This change causes the gene to malfunction and thus results in the accelerated growth of malignant cells2.
The clinical picture depends on the location and size of the tumor. The mediastinal presentation may be asymptomatic or show signs and symptoms such as cough, stridor, respiratory distress, and evidence of vascular compression, such as superior vena cava syndrome3.
This type of tumor has a poor prognosis: in a series of 100 children diagnosed with extracranial rhabdoid tumor (2005 to 2014), overall survival at 3 years was only 38.4%4.
Malignant tumors are among the leading causes of mortality in pediatric patients, highlighting the importance of ruling them out as part of oncologic emergencies. This report aims to inform pediatricians how such a common symptom as laryngeal stridor can be secondary to severe pathologies, as in this case, a rhabdoid tumor of infrequent presentation. We also aim to raise awareness in the medical community about the timely detection of tumors and the identification of patients with a genetic predisposition. We report the clinical findings and the diagnostic-therapeutic methodology used unsuccessfully, in this case, to continue research on this subject and establish prognostic factors since there are no standardized therapy nor study protocols to develop an adequate chemotherapy/radiotherapy scheme that allows a higher survival rate.
Clinical case
We describe the case of an 8-month-old male patient admitted to the emergency department with 2-week evolution of symptoms consisting of rhinorrhea, sporadic cough, dysphonia, laryngeal stridor when crying, and polypnea. A posteroanterior and lateral chest X-ray reported mediastinal widening with airway compression; an emergency simple contrast-enhanced chest CT scan showed asymmetric hemithorax due to less volume expansion on the right side, with trachea decreased in caliber displaced to the left and surrounded by a hypoattenuating image with soft tissue density. Distally, the trachea partially recovered its caliber at the level of the carina; the main bronchi were well pneumatized. We observed a large mass with homogeneous soft tissue density and smooth, well-defined borders (6.7 x 4.6 x 5.5 cm in its principal axes), showing poor predominantly peripheral enhancement and small central vessels when contrast was administered. The mass displaced and compressed the trachea and the cardiac silhouette, causing atelectasis with an air bronchogram in the pulmonary base on the same side. The contralateral lung parenchyma was normal. The cardiac profile was of standard shape and size, slightly displaced to the left (Figure 1).
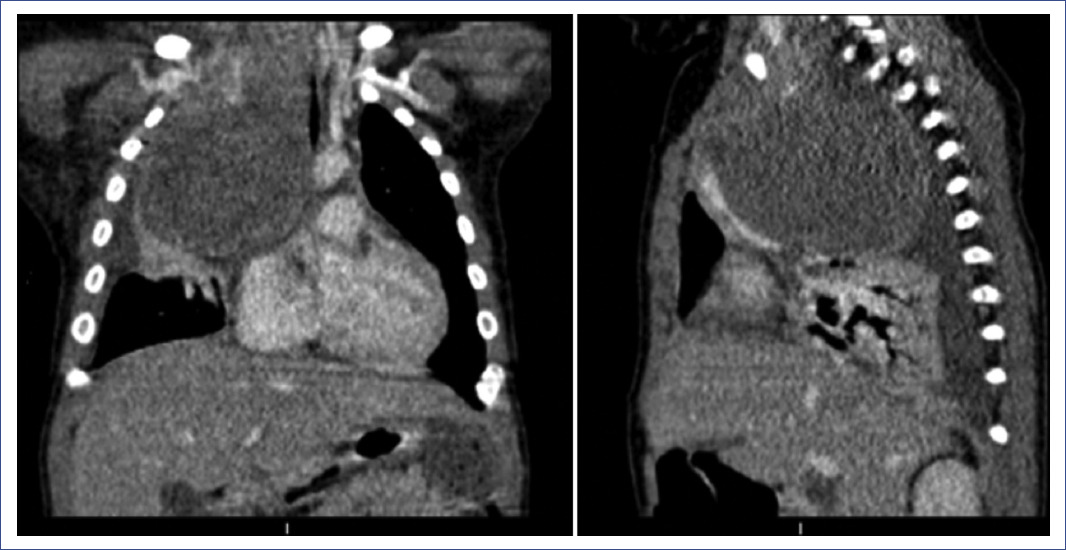
Figure 1 Initial computed axial tomography of the thorax in coronal and sagittal slices showed a solid mass of heterogeneous appearance, hypodense, displacing blood vessels and airway in the prevascular space, significantly reducing the tracheal caliber, right middle lobe atelectasis, and right pleural effusion.
Alpha-fetoprotein and human chorionic gonadotropin results were negative.
Empirical chemotherapy with vincristine (0.05 mg/kg/day) and doxorubicin (1 mg/kg/day) was initiated to reduce tumor volume, and the patient was admitted to the Intensive Care Unit.
Two days after initiating chemotherapy, we found anterior cervical lymphadenopathy and data suggestive of superior vena cava syndrome. A total right pleural effusion was found with a chest X-ray (Figure 2), so emergency incomplete tumor resection and drainage of the pleural effusion by median sternotomy were performed without perioperative complications (Figure 3). The patient was extubated two days after surgery and was maintained on high-flow nasal prong therapy, which decreased to low-flow after 24 hours.
Bone marrow biopsy, aspirate, immunophenotyping, and karyotyping showed no neoplastic infiltration; urine alpha-fetoprotein, human chorionic gonadotropin, and catecholamine quantification tests were negative, excluding the presence of the most frequent mediastinal tumors.
The patient was discharged from the Intensive Care Unit three days later and admitted to the Pediatrics Service. A transthoracic Doppler echocardiogram reported a pedunculated mass (5 x 6 cm) located at the arrival of the superior vena cava to the right atrium, thus concluding tumor infiltration to great vessels and right atrium.
After ten days of stay in the pediatrics department, the patient presented an intense crying crisis associated with stridor, severe respiratory distress, and significant desaturation, for which he was readmitted to the Intensive Care Unit, requiring high-flow ventilation. Subsequently, the patient presented bradycardia and severe desaturation with progression to mechanical ventilation. Sedation and advanced resuscitation maneuvers were required.
The control radiography showed right basal pneumonia, suspected right diaphragmatic paralysis, and a mediastinal mass with airway obstruction. Bronchoscopy showed dynamic occlusion of 40% of the airway at the tracheal level; tracheomalacia was diagnosed.
The pathology report showed a poorly differentiated malignant neoplasm with abundant tumor necrosis and recent hemorrhage, with infiltration of adjacent soft tissues. It was classified as an extrarenal rhabdoid tumor with SALL4+, CMYC+, CKAE1/AE33+, GLIPICAN 3+, INI1-, and a proliferation index of 70%.
An antineoplastic regimen was initiated based on carboplatin (19 mg/kg/day, single dose), ifosfamide (1800 mg/m2SC/day, days 1-3), and etoposide (3.3 mg/kg/day, days 1-3). Adequate tumor volume reduction was observed, and invasive mechanical ventilation was successfully withdrawn. He was discharged from the service and continued with chemotherapy according to the high-dose protocol of the European Rhabdoid Registry (EU-RHAB) for six cycles5.
A genetic study by microsatellite technique showed SMARCB1 gene loss, which confirmed the diagnosis of extrarenal rhabdoid tumor. Treatment was complemented with radiotherapy at a dose of 50.4 Gy in 28 fractions with concomitant weekly radiosensitizing vincristine with apparent good initial clinical evolution. However, during radiotherapy, the patient presented tumor progression data, so it was necessary to start a second-line VOIT (vincristine, irinotecan, temozolomide) scheme without a favorable response to treatment. The patient died 85 days after diagnosis and treatment.
Discussion
The present case report describes an 8-month-old male patient with an initial clinical picture of laryngeal stridor and respiratory distress. The clinical picture at admission initially suggested laryngotracheitis; however, differential diagnoses had to be considered, among which extrinsic compression of the airway and neoplasms were possible etiologies. Airway compression was initially diagnosed by chest X-ray and later delimited by computed tomography. This etiology explains the cause of the failure of the initial treatment with racemic epinephrine. Subsequently, the presence of the most frequent mediastinal tumors was ruled out through biochemical data. Finally, a more specific study protocol was initiated for less frequent pathologies, treating the patient initially with empirical chemotherapy. Once the tumor type was morphologically identified, treatment for this type of tumor was initiated based on the EU-RHAB. The diagnosis was corroborated by pathology and immunohistochemistry studies, determining the loss of the SMARCB1 gene. Despite adhering to the management guidelines established by EU-RHAB, the prognosis was as unfavorable as the international statistics at 3 months of follow-up under oncologic and surgical treatment.
Rhabdoid tumors are highly aggressive and lethal in the pediatric population. These tumors mainly affect children under 3 years of age, with a higher frequency in males3. The present case was an 8-month-old infant, an age group in which biallelic somatic inactivation secondary to the SMARCB1 gene mutation occurs and less frequently the SMARCA4 gene mutation. A predisposition due to a germline mutation may exist6-9.
Few cases of rhabdoid tumors located in the mediastinum have been described. One case was reported in Mexico of a female patient with chronic upper respiratory tract infection diagnosed by immunohistochemistry and treated with radiotherapy and chemotherapy based on cyclophosphamide, carboplatin, and etoposide9,10. In the case described here, a SMARCB1 gene mutation was identified by a microsatellite genetic study, which supported SMARCB1 or INI-1 gene deficiency. The SMARCA4 gene mutation has a higher ratio in hereditary transmission from one of the healthy parents unaffected by the mutation, whereas the SMARCB1 gene exceptionally presents in this form.
Rhabdoid tumors are mainly located in the kidney; the most frequent extrarenal location is in the central nervous system (up to 50% in the cerebellum), although it can infrequently occur in the head and neck, paravertebral muscles, liver, bladder, mediastinum, retroperitoneum, and heart.
The clinical presentation will depend on the location. The mediastinal presentation usually includes chest pain, dyspnea, cough, variable respiratory distress, and constitutional symptoms such as weight loss and generalized weakness3. Some cases even include superior vena cava syndrome or compression of the airway or great vessels due to mass effect or direct invasion of the tumor1,11,12. As we observed in this case, the patient showed an atypical extrarenal location in the mediastinum that started with respiratory symptoms due to the mass effect of the tumor.
In the case of neurological localization, this tumor has been described with initial presentation of subarachnoid and intraventricular hemorrhage13, and even acute hydrocephalus14 and de novo spinal cord presentations. There are also reports of cases in which it is difficult to distinguish between this type of tumor and other more frequent tumors or other pathologies. Differential diagnoses have been reported with yolk sac type tumors, neurofibromatosis type 2, and hydrops fetalis with a metastatic presentation of the tumor to the placenta during pregnancy15-17.
On computed tomography, the mediastinal tumor appears as a large heterogeneous mass that commonly presents displacement of the heart and mediastinal structures3; it also tends to infiltrate blood vessels, the airway, and adjacent structures. In this case, we described a tumor that caused a significant displacement of vessels and the airway, and infiltration of the superior vena cava and right atrium, which made it unresectable due to its invasive characteristics. The definitive diagnosis was made with histopathological and immunohistochemical studies, identifying the representative morphological characteristics in addition to the SMARCB1- or SMARCA4- gene mutations1,3,6,9.
Histologically, this type of tumor is classified into the following main groups: conventional-type tumors, the most common with the typical description; atypical teratoid/rhabdoid-type tumors, with myxoid matrix pattern, basophilic or with mucopolysaccharides, and small cell-type tumors, without rhabdoid cells, with small, round cells and scarce cytoplasm18. This case corresponds to the conventional type.
The mediastinal rhabdoid tumors usually present in advanced stages when it has become unresectable, as in this case. Approximately 20% of patients will have disseminated disease at the time of diagnosis. Survival curves have shown a survival rate of 31-38% at 3 years and 15-36% at 5 years1,7,13.
The suggested treatment described by the European Rhabdoid Registry is based on high-dose chemotherapy. It is also necessary to evaluate which patients will benefit from the adjuvant use of radiotherapy, depending on the presentation, manifestations, time of diagnosis, and prevention of complications inherent to oncologic treatment. There is no registry of prognostic factors for survival, so it is not yet possible to determine which patients will benefit from each scheme established by the European registry.
A strength of this case report is that all the information on the tumor was available; however, the diagnosis was difficult due to the low incidence of this neoplasm. Additionally, no diagnostic and treatment protocol for this type of non-neurological extrarenal tumor has been reported in the literature. Moreover, it is essential to remember that oncologic emergencies also cause respiratory distress. Therefore, it is vital to identify them promptly.
Mediastinal extrarenal rhabdoid tumor is a rare, very aggressive tumor with a poor prognosis. Although an early diagnosis and aggressive treatment are required, a 5-year survival > 40% has not been possible to exceed10. For this reason, it is necessary to study more cases to achieve specific treatment guidelines.
This paper describes the case of an 8-month-old patient with infiltration of large vessels and extrinsic compression of the airway, with an initial presentation of laryngeal stridor and severe respiratory distress. An exhaustive study was necessary to reach the clinical, imaging, surgical, histopathological, immunohistochemical, and genetic diagnoses. The multidisciplinary medical team administered thorough treatment. This is the first documented case in Mexico of a rhabdoid tumor with SMARCB1 gene loss detected by microsatellites, immunohistochemistry, and pathology.











 nueva página del texto (beta)
nueva página del texto (beta)




