Introduction
Healthcare-associated infections (HCAIs) are a severe problem worldwide. In the U.S., at least one HCAI is diagnosed every day in approximately one out of 31 hospitalized patients1. The mean prevalence of HCAIs is between 10 and 20%, according to different studies worldwide. Furthermore, the prevalence in intensive care units (ICUs) increases to 35-50%2. In Mexico, HCAIs prevalence is approximately 5%, although no specific ICU studies exist3. Among studies that included pediatric patients, the most frequent HCAIs were bloodstream infections, upper respiratory tract infections, and nosocomial pneumonia. The most frequent microorganisms responsible for these HCAIs were coagulase-negative staphylococci, enterococci species, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter species2.
Several studies have shown that HCAIs are preventable4. HCAI prevention strategies include hospital hygiene, hand hygiene, personal protective equipment, safe use and disposal of sharps, asepsis, assessment of the need for catheterization, catheter type selection, catheter insertion, catheter maintenance, and education of patients, family members, and healthcare personnel5-7. In addition, a poor patient-nurse ratio (PNR) has been associated with higher proportions of HCAIs8-11.
More adequate human resources could be a strategy to prevent HCAIs. However, the need for more nursing personnel is global. The U.S. Bureau of Labor Statistics predicts that there will be a shortage of 11 million nurses12. The State of the World's Nursing reported a "shortfall of 5.9 million nurses" in 202013; it is expected that "10.6 million nurses will be needed by 2030"14. According to the Organization for Economic Cooperation and Development (OECD), Mexico has 2.85 nurses per 10,000 inhabitants, a figure well below the global average of 9 nurses per 10,000 inhabitants15. High nurse shortage rates make it challenging to achieve the recommended PNR goals. For ICUs and emergency rooms, a ratio of one nurse for every 1-2 patients is recommended16,17. However, different reports show that this is not always achieved18.
Few studies have demonstrated the correlation between PNR and HCAIs in the pediatric population. Some studies have addressed the relationship between nursing staff and specific HCAIs19,20. However, these studies were conducted in neonatal intensive care units (NICUs) or considered only one type of infection. More information is needed on poor PNR and its association with different HCAIs, specifically in the pediatric population.
Regarding the scarce evidence in the general pediatric population, we conducted a prospective analysis to address the association between PNR and HCAIs in a tertiary-level pediatric hospital.
Methods
We conducted a descriptive and prospective study in a tertiary-level pediatric hospital in Mexico. The emergency and surgery departments, surgical ICU (SICU), pediatric ICU (PICU), and NICU were included. Data were obtained from the nursing department attendance records and the epidemiology department surveillance records for 18 months.
The unit of study was the 24-hour day (considering morning, evening, and night shifts) in each hospital service (emergency, surgery, SICU, PICU, NICU). The primary outcome variable was the presence of one or more HCAIs per day and hospital unit.
We used the CDC/National Healthcare Safety Network (NHSN) definitions of HCAIs21,22. The HCAIs studied were catheter-associated urinary tract infections (CAUTI), urinary tract infections (UTI), hospital-acquired pneumonia (HAP), central line-associated bloodstream infections (CLABSI), varicella, occult bacteremia (OB), primary bloodstream infections (PBSI), and procedure-related pneumonia (PRP). OB was defined as the "presence of bacteria in the bloodstream of febrile children who have no apparent foci of infection"23. PBSI was defined as the "presence of viable bacterial or fungal microorganisms in the bloodstream (subsequently demonstrated by the positivity of one or more blood cultures) that elicit or have elicited an inflammatory response"24. PRP was considered in cases where pneumonia was documented 48 hours after specific procedures such as bronchial aspiration, foreign body extraction, intubation for surgical procedures, antisepsis practices at the time of intubation, and tooth brushing.
Previously, De la Rosa-Zamboni et al. described epidemiologic surveillance7. Trained nurses visited all wards three to four times weekly to detect suspected cases. Infectious disease physicians and specialized nurses from the Department of Health Epidemiology validated each suspected case of HCAI. The presence of infection was attributed to the three shifts from the three previous calendar days before the condition to determine the PNR for HCAI risk. For example, if the HCAI event was on day 25, the PNRs of the three shifts on day 22 were considered an exposure. Therefore, the unit of study was the workday that included all three shifts in each unit. The definition of HCAI and the day of the event were taken from the NHSH/CDC surveillance definitions at the time of the study21.
The primary exposure variable was the PNR. The PNR was obtained by dividing the number of patients in a unit during a shift by the number of nurses in that same area and shift. The nurses who were not in charge of patients, i.e., those in charge of administrative tasks, were excluded from the analysis. The sources of information were the nursing department attendance records and the patient census. Nurse attendance was defined as the percentage of nurses arriving at work compared to those scheduled. In addition, if support nurses were sent to the units studied, these nurses were also considered in the calculation.
Other exposure variables considered for the study were absenteeism, number of patients on mechanical ventilation, number of nurses reassigned from their usual workplace to the units studied (nursing support staff), pre-scheduled nurse absences, seasonality, and the period when resident physicians begin their specialty. We considered seasonality a confounding variable due to the influence of weather on the rate of respiratory infections. November to January was considered the period of cold weather. In addition, during this period, there are more absences due to Christmas and New Year's holidays. June to August was considered the rainy season. We included nursing support staff since they are taken from units that may have different protocols and other types of patients, such as neonatal and surgical patients. From March to May, the period when residents begin their specialty was taken as an approximation of the adaptation time and learning curve of residents.
Statistical analyses were performed using Stata 15. We compared categorical variables with the χ2 test and conducted univariate and bivariate analyses. We calculated odds ratios (OR) and 95% confidence intervals (CI) for the different HCAIs. We used logistic regression to estimate the OR and adjust for confounders. For specific analyses, the PNR was considered a quantitative variable, while for others, as a categorical variable categorized as follows: 1:1; 2:1; 3:1; 4:1, and ≥ 5:1. The variable HCAI was dichotomized into presence or absence. We performed a χ2 test for the multivariate model to determine the association between variables and the outcome variable. If the association was significant, the variable was retained for model construction. These variables were added one by one to the model; if the risk (OR) changed substantially, i.e., more than 10%, the variable was retained. A likelihood ratio test was performed with each variable to determine if the models differed (p < 0.05).
Results
From July 1, 2017, to December 31, 2018 (549 days), 63,114 attendance entries were analyzed. The number of patient days during the study was 43,349, with a median of 17 hospitalized patients per day. Two hundred HCAIs were identified, 4.6 per 1000 patient days. The median of PNR was 2:1 (Table 1). This same table contains the data for each unit studied.
Table 1 Baseline characteristics
| Total | Emergency | PICU | SICU | Surgery | NICU | p-value | |
|---|---|---|---|---|---|---|---|
| Patient-days | 43,349 | 9,678 | 4,704 | 4,074 | 12,476 | 12,417 | |
| Hospitalized patients per day* | 17 (9-23) | 18 (14-22) | 9 (8-10) | 8 (6-9) | 23 (21-25) | 23 (20-25) | < 0.001 |
| HCAIs, n | 200 | 10 | 26 | 30 | 47 | 87 | |
| Rate per 1000 patient-days | 4.61 | 1.03 | 5.53 | 7.36 | 3.77 | 7.01 | < 0.001 |
| Assistance, n (%) | |||||||
| Total | 53,512 (84.8) | 13,823 (85.5) | 9,090 (82.4) | 9,047 (81.3) | 7,570 (84.7) | 13,982 (88.3) | < 0.001 |
| Morning | 21,640 (90.2) | 5,812 (90.9) | 3,489 (87.0) | 3,541 (88.7) | 3,475 (90.7) | 5,323 (92.3) | < 0.001 |
| Evening | 16,100 (90.3) | 4,299 (91.0) | 2,872 (89.6) | 2,659 (84.4) | 2,115 (93.7) | 4,155 (92.4) | < 0.001 |
| Night | 15,772 (74.0) | 3,712 (73.4) | 2,729 (71) | 2,847 (71.3) | 1,980 (69.3) | 4,504 (80.8) | < 0.001 |
| Patients per nurse* | |||||||
| Total | 2.1(1.5-3.1) | 2.3 (1.8-2.8) | 1.4 (1.3-1.7) | 1.4 (1.2-1.7) | 4.2 (3.8-4.8) | 2.6 (2.3-2.9) | < 0.001 |
| Morning shift | 1.9 (1.3-2.7) | 1.9 (1.4-2.2) | 1.3 (1.2-1.5) | 1.3 (1.2-1.5) | 4 (3.6-4.3) | 2.4 (2.2-2.6) | < 0.001 |
| Evening shift | 2.3 (1.7-3.2) | 2.5 (2-3) | 1.6 (1.4-1.8) | 1.6 (1.3-1.8) | 4.4 (4.0-5.0) | 2.7 (2.5-3.0) | < 0.001 |
| Night shift | 2.3 (1.5-3.3) | 2.5 (2-3) | 1.4 (1.3-1.7) | 1.5 (1.3-1.8) | 4.5 (4.0-5.0) | 2.6 (2.3-3.0) | < 0.001 |
*Median (IQR).
**χ2, KruskalWallis. HCAI, healthcare-acquired infections; IQR, interquartile range; NICU, neonatal intensive care unit; PICU, pediatric intensive care unit; SICU, surgery intensive care unit.
Differences were observed between the HCAIs rates of the units studied. The units with the highest rate of HCAIs were SICU and NICU. In contrast, the emergency unit showed the lowest rate of infections.
Absenteeism, a factor affecting the PNR, was 15.2% during the study period. This rate varied according to department and shift. The lowest absenteeism rate was recorded in the surgery unit during the evening shift, with only 6.3%, while the night shift from the same unit showed the highest rate of 30.7%. In all units studied, the night shift had more absences. For all shifts and units, the most frequent PNR was 2:1 (n = 3,388, 41.1%, p < 0.001). However, in more than half of the recorded nursing attendances (56.3%), more than three patients per nurse were registered, sometimes reaching seven patients per nurse (0.5%).
All studied units and shifts required at least one support nurse. The evening shift required the most nursing support staff: 48.6% (n = 1341, p = 0.024) of the required nurses covered by nursing support staff. The surgery department needed 69.1% (1,144) of nursing support staff. The SICU had the lowest staffing requirements; the nurses in this unit covered 71% (1,177) of the staff requirement.
According to logistic regression, in the univariate analysis, PNR was positively associated with the occurrence of HCAIs (OR, 1.85; 95%CI, 1.59-2.15; p < 0.001).
In the multivariate analysis, the confounding variables fitting the model (p < 0.05) were the following: shift, patients with mechanical ventilation, nursing support staff, weather, previously planned absences, and the period in which the residents start their medical specialties. Adjusting for confounding variables in the model, the PNR was positively associated with the occurrence of HCAIs (OR 1.54; 95%CI 1.421.67; p < 0.001). Mechanical support increased the risk of HCAIs (OR 1.14; 95%CI 1.111.18; p < 0.001). Nursing support staff showed a borderline value (p = 0.06) for being a risk factor for HCAIs (OR 1.09, 95%CI 11.19) (Table 2).
Table 2 Multivariate analysis of risk for HCAIs with PNR and with all the variables included in the model
| Variable | OR | p-value | 95%CI | |
|---|---|---|---|---|
| PNR | 1.54 | < 0.001 | 1.42-1.67 | |
| Shift | Morning | 1 | ||
| Evening | 0.66 | < 0.001 | 0.53-0.81 | |
| Night | 0.63 | < 0.001 | 0.51-0.78 | |
| Special conditions | Mechanical ventilation | 1.14 | < 0.001 | 1.11-1.18 |
| Nursing support staff | 1.09 | 0.06 | 1.00-1.19 | |
| Previously planned absences | 0.91 | 0.41 | 0.72-1.14 | |
| Period | Cold weather season | 1 | ||
| Resident starting period | 1.08 | 0.57 | 0.83-1.40 | |
| Raining season | 0.76 | 0.03 | 0.60-0.98 |
CI, confidence interval; HCAI, healthcare-associated infection; OR, odds ratio; PNR, patient-nurse ratio. Logistic regression was performed with the variables that fit into the model.
The correlation between PNR and HCAIs showed a positive trend: the higher the number of patients per nurse, the higher the risk of HCAIs (Figure 1).
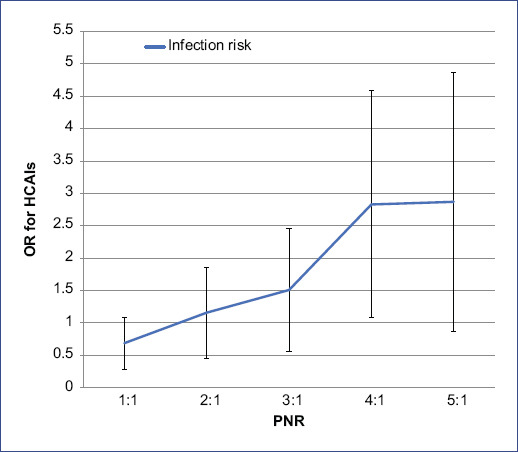
Figure 1 Risk of infection by PNR. Black lines indicate 95% confidence intervals (95%CI). HCAIs: healthcare-associated infections; OR: odds ratio; PNR: patient-nurse ratio.
Univariate and bivariate analyses were conducted. These analyses showed that PNR is a risk factor for different HCAIs. A high number of patients per nurse increased the risk of CAUTI by 33% (95%CI 1.04-1.71; p = 0.022), of UTI by 82% (95%CI 1.34-2.46; p < 0.001), of HAP by 39% (95%CI 1.22-1.58; p < 0.001), of PRP by 108% (95%CI 1.41-3.07; p < 0.001), of varicella by 133% (95%CI 1.08-5.03; p = 0.031), and of CLABSI by 21% (95%CI 1.05-1.41; p = 0.009) (Table 3).
Table 3 Univariate and bivariate analysis of PNR with each type of HCAI, including nursing support staff
| Crude | Adjusted for supporting staff | |||||
|---|---|---|---|---|---|---|
| Risk according to the PNR | Risk according to PNR including the nursing support staff | |||||
| OR | CI | p-value | OR | CI | p-value | |
| CAUTI | 1.28 | 1.00-1.63 | 0.045 | 1.33 | 1.04-1.71 | 0.022 |
| UTI | 1.93 | 1.44-2.57 | < 0.001 | 1.82 | 1.34-2.46 | < 0.001 |
| HAP | 1.41 | 1.24-1.60 | < 0.001 | 1.39 | 1.22-1.58 | < 0.001 |
| OB | 1.05 | 0.92-1.20 | 0.446 | 1.05 | 0.91-1.20 | 0.48 |
| PRP | 2.09 | 1.43-3.05 | < 0.001 | 2.08 | 1.41-3.07 | < 0.001 |
| Varicella | 2.33 | 1.09-4.97 | 0.029 | 2.33 | 1.08-5.03 | 0.031 |
| CLABSI | 1.24 | 1.07-1.43 | < 0.003 | 1.21 | 1.05-1.41 | 0.009 |
| PBSI | 1.50 | 1.31-1.72 | 0 | 1.44 | 1.25-1.66 | 0 |
CAUTI, catheter-associated urinary tract infection; CI, confidence interval; CLABSI, central line bloodstream infection; HAP, hospital-acquired pneumonia; OB, occult bacteremia; OR, odds ratio; PBSI, primary bloodstream infection; PNR, patient-nurse ratio; PRP, pneumonia related to procedure; UTI, urinary tract infection. These variables were explored using logistic regression.
Discussion
This study brought to light some interesting facts that had yet to be examined in the pediatric population in developing countries. We found that a higher number of patients per nurse on any given shift was associated with developing HCAIs. We also found that the risk of PRP and varicella infection doubled if the number of patients per nurse was high.
We found a positive association between a high number of patients per nurse and the risk of HCAIs; specifically, the risk increases when the PNR is ≥ 3:1. This aspect has hardly been described in the pediatric population. Tubbs-Cooley et al. (2019) found a mean PNR of 2:1 in a U.S. academic medical center and reported a negative correlation between this parameter and an acuity score (p < 0.001)25. However, this measurement was obtained only in the NICU, and they did not consider HCAIs as an outcome. In 2017, Tawfik et al. reported an association between HCAIs and California NICU nurses' perception of excessive workload. These authors stated that overwork might make nurses "less likely to notice errors or omissions in healthcare delivery," although they did not measure PNR26. Blot et al. found a relationship between PNR and ventilator-acquired pneumonia (VAP), but this study was conducted in an adult ICU. They reported fewer VAPs with a 1:1 PNR than when the PNR was >1:1 (p = 0.002)27. However, they did not address other types of HCAIs. Although we found that PNR increases the risk of PRP by 108% (p < 0.001), no association was found with different types of pneumonia. In 2011, Schwab et al. published a mean PNR in a study conducted in German ICUs similar to our research. They found that adequate PNR was associated with fewer cases of HCAIs; however, the association was lost in the multivariate analysis28.
In this study, the increased risk of HCAI was maintained even in multivariate analysis, probably due to the presence of nursing support staff. We found that sending nursing support staff to areas with nursing staff shortages solved the problem. However, a marginally significant association between nursing support staff and HCAI risk was identified in the multivariate analysis (OR 1.09, p = 0.06). Few studies have considered nursing support staff within their confounding variables. Bae et al. and Xue et al. did consider nursing support staff in their studies. However, they found no association between nursing support staff and HCAIs29,30. We propose that more extensive studies are needed to evaluate the role of support nurses and other factors, such as the preparation and expertise of supporting nurses to address this issue.
A higher risk of HCAIs was observed during the morning shift, independently of the other factors, and a lower rate of HCAIs in the emergency department. This finding could be associated with several factors not measured in the study because they are outside its scope. Such factors could be workload, sampling, medical rounds, and preparation of solutions and medications, among other procedures that may be more frequent in the morning shift. As for the emergency unit, they take fewer cultures. However, a limitation of our study is that these factors should have been measured. Further studies are required to analyze the risk of these factors.
When the types of infection were analyzed, hospital-acquired varicella and PRP were the HCAIs most strongly associated with PNR. Poor PNR doubles the risk of developing these infections. One hypothesis is that a higher workload is related to a lower adherence to protective equipment when caring for children with varicella and a lower adherence to hand hygiene. In the case of PRP, it could be that all necessary preparations for procedures, such as adequate oral care before surgery, were not correctly performed. Finding the causes of these infections should be the subject of future research, as these associations have yet to be described.
If a PNR of 2:1 is maintained most of the time, it will likely reduce the rate of HCAIs. The mean PNR in our study was 2:1, consistent with international guidelines and recommendations for ICUs16,17. However, in some shifts, there was a PNR of up to 7:1, which can be counterproductive for patients.
One of the limitations of our study was that there are other factors that, according to some authors, should be considered and should have been included. These factors include technological advances in healthcare, epidemiological profiles of the region, academic and professional staff profiles, and social, political, cultural, and health services31-33. As this is a tertiary-level hospital, the professional profiles are homogeneous within the services studied, and the included patients' and nurses' social and political context. In addition, the needs and complexity of each patient still needed to be addressed. However, all the services studied are critical care services, and a patient on mechanical ventilation was considered to need specialized and vital care. Finally, this study responds to what is experienced in many hospitals on a day-to-day basis since, in most hospitals, staffing is calculated by considering only the number of beds and patients with the traditional and pragmatic method34. The causes of absenteeism were not identified in this study, although it could be helpful to address this aspect in the future.
In conclusion, our data indicate that a high number of patients per nurse increases the risk of several types of HCAIs. Nurse staffing is critical for optimal patient care. Therefore, we strongly support the need to consider PNR in designing and implementing any HCAIs policy or preventive package.











 text new page (beta)
text new page (beta)


