Introduction
Congenital Zika syndrome (CZS) is considered a specific pattern of newborn defects caused by Zika virus (ZIKV) infection, a microorganism that has been considered a teratogenic agent1-3. Although the pathophysiological pathways by which this infection causes organ dysfunction are still under investigation, nervous system, musculoskeletal and visual impairment have been described in infected newborns. The following clinical manifestations stand out: microcephaly with subcortical calcifications, retinal alterations, congenital contractures, early hypertonia, and extrapyramidal symptoms, which can occur together or separately in each patient4,5.
ZIKV infection has become very important in recent years because it is associated with significant health problems worldwide and has been classified as a public health emergency of international concern6. This has prompted various international organizations such as the World Health Organization (WHO), the United States Centers for Disease Control and Prevention (CDC), and the Pan American Health Organization (PAHO) to take preventive measures to avoid its further progression as a pathological entity6-8.
In October 2015, the Secretaría Estatal de Salud (State Health Secretariat) of Pernambuco, Brazil, reported 26 cases of microcephaly associated with ZIKV infection8,9. Subsequently, countries worldwide began to report cases of patients with microcephaly and infection with serum ZIKV viral load. ZIKV infection during pregnancy was found to cause CZS and complications during pregnancy, such as preterm labor or even spontaneous abortion5,10.
In Mexico, epidemiological surveillance has been conducted through the Secretaría de Prevención y Promoción a la Salud (Secretariat of Prevention and Health Promotion). According to the information bulletin "Confirmed cases of ZIKV disease" for the 52nd epidemiological week of 2021, 12,991 cases of ZIKV infection were reported from 2015 to December 31, 2021, with Veracruz, Yucatán, and Nuevo León being the states with the highest number of confirmed cases. In addition, it was reported that 7152 pregnant patients presented ZIKV infection, with Yucatán having the highest number of cases with 926, followed by Veracruz with 888 cases and Tamaulipas with 692 cases11. In addition, 44 cases confirmed by epidemiological association of CZS and 56 laboratory-confirmed cases of CZS were reported12,13.
At present, the diagnosis of ZIKV disease in first-contact health services is complicated due to the similarity of the clinical picture with diseases caused by other viruses of the same genus, such as Dengue and Chikungunya virus14-16 (Table 1). Symptoms are generally mild, lasting 2-7 days, and may consist of fever, rash, conjunctivitis, muscle and joint pain, malaise, and headache; however, most infected patients are asymptomatic8.
Table 1 Main clinical manifestations in Zika, dengue and Chikungunya virus infections
| Signs and symptoms | Zika | Dengue | Chikungunya |
|---|---|---|---|
| Reason for consultation | Exantema o prurito | Fever, myalgia | Joint pain, fever |
| Fever | Mild | Moderate | Intense |
| Very infrequent | Very frequent | Very frequent | |
| Duration: 1-3 days | Duration: 5-7 days | Duration: 5-7 days | |
| Exanthema and features | Typically from day 1 | Appears from 5th to 7th day | Appears on the 2nd or 3rd day |
| Maculopapular, cephalo-caudal | Not characteristic | Not characteristic | |
| Pruritus | Moderate to intense | Mild to severe | Mild to moderate |
| Conjuntivitis | Very frequent | Infrequent | Adults: Very rare/Children: Very common |
| Neurological manifestations | Possible and serious | Infrequent | Infrequent (can be frequent and severe in newborns) |
| Headache | Mild to moderate | Intense and frequent | Mild to moderate |
| Retro-orbital pain | Infrequent | Intense and frequent | Infrequent |
| Polyarthralgia | Frequent | Absent | Very frequent |
| Polyarthritis | Frequent | Absent | Frequent |
| Myalgia | Infrequent | Very frequent and intense | Frequent, moderate to severe |
| Diarrhea | Very infrequent | Frequent | Very infrequent |
| Skin bleeding | Very infrequent | Frequent | Very infrequent |
| Mucosal bleeding | Very infrequent | Alarm sign | Very infrequent (severe when present) |
ZIKV
The virus was named after the Zika forest in Entebbe, Uganda, Africa, where it was discovered in 1947 in rhesus monkeys, in which transmission was only enzootic, restricted to primate-mosquito circulation17,18.
Subsequently, the first case of human transmission was reported in 1954 in a 10-year-old Nigerian girl who had a serum viral load of ZIKV. However, it was difficult to relate her clinical presentation to ZIKV infection because parasites of the genus Plasmodium were also found in her blood samples19. In the same year, two more cases of ZIKV infection in humans were reported, confirmed by increased serum-neutralizing antibodies20. In 1966, ZIKV infection was massively detected in the Asian population, which increased research on human transmission. As a result, the ability of the virus to infect humans through a vector was reported, and its wide geographical distribution and the presence of different viral lineages, both from the African and Asian continents, were demonstrated21. Subsequent studies showed that ZIKV is an arbovirus of the genus Flavivirus, whose main vector is the Aedes aegypti mosquito1. Since then, cases of ZIKV infections in humans with diverse clinical manifestations have been reported; over time, cases with more severe alterations have appeared5,15,22.
Subsequently, a high incidence of cases was reported in 2007 on the islands of Yap in Micronesia23, and in 2008 the first cases of sexual transmission were reported24. In 2013 and 2014 in French Polynesia, the first cases of ZIKV infection were reported with post-infectious onset of Guillain-Barré syndrome, maternal-fetal transmission, and the presence of viral load in semen samples from asymptomatic donors25. In the Americas, it is estimated that ZIKV was introduced between May and December 2013; however, the first reported cases of CZS were in May 2015 in Brazil, attributed to globalization and migratory movements due to social and sporting events5,26,27.
The worldwide spread of the virus was rapidly progressive, and cases began to be documented in subtropical areas, Central and North America, and 87 countries of different geographic distribution. More than 500,000 cases were reported worldwide. This prompted the WHO to declare ZIKV infection as a Public Health Emergency of International Concern on February 1, 2016, and temporarily confirmed the association of ZIKV infection with microcephaly, Guillain-Barré syndrome, sexual, blood and vertical transmission, as well as the occurrence of severe birth defects in neonates with parents with a history of ZIKV infection5-7,20.
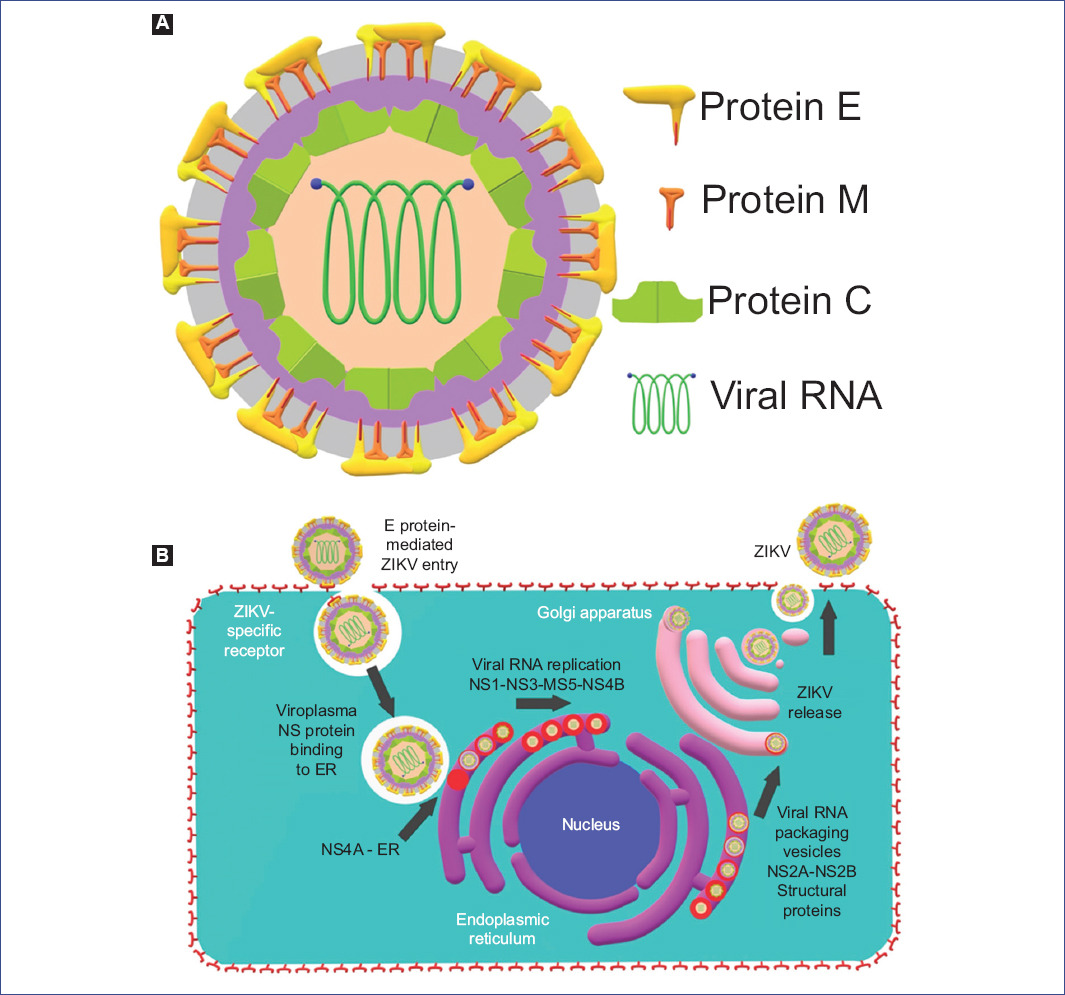
ZIKV belongs to the Flavivirus genus of the Flaviviridae family and measures approximately 40 nanometers (nm) in diameter. Its genetic material corresponds to a single-stranded ribonucleic acid chain (single-stranded RNA) of positive polarity, which encodes a polyprotein whose translation gives rise to three structural proteins: capsid protein (C), membrane precursor (prM) and envelope protein (E), and 7 non-structural proteins (NS): NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS528. The function of each of these is described in Table 2.
Table 2 Functions of Zika virus proteins
| Type | Protein | Function |
|---|---|---|
| Structural | Protein C | Forms the viral capsid |
| Protein E | Enables membrane binding and fusion with the host cell, penetration and hemagglutination during the viral replication cycle | |
| Protein prM | Generates M protein, which releases mature virion out of the cell forming complexes with E protein | |
| Non-structural | NS1 | Initiates the process of viral RNA genome synthesis |
| NS2A | Interacts with NS3 and NS5 for viral packaging and replication | |
| NS2B | Interacts with NS3 for viral packaging and replication | |
| NS3 | Harbors RNA protease and helicase activity, essential for viral replication and survival | |
| NS4A | Participates in the localization of the replication complex to the membrane | |
| NS4B | Assists NS3 protein | |
| NS5 | Participates in the inhibition of the host innate immune system and is a coadjuvant of the NS3 protein in the nuclear localization of the virus |
Adapted from Panwar28.
The viral particle consists of a symmetric icosahedral structure with a viral envelope containing the E and M proteins as molecules for attachment and host cell recognition (Fig. 1A)26,29. The entry of ZIKV into the host cell is mediated by the E protein, which allows attachment and fusion to the specific receptors TIM1, TYRO-3, and AXL, thus activating the endocytosis processes and the entry of the virion into the cell cytoplasm29,30.
Inside the cell, non-structural proteins bind to the endoplasmic reticulum (ER), forming a complex that allows replication and assembly of viral RNA called viroplasm31. This involves NS4A and the formation of ER invaginations in which NS1 subsequently acts to initiate the viral genome replication processes, and NS3 RNA helicase and NS5 polymerase act, assisted by NS4B. Viral packaging requires the action of NS2A and NS2B through viral RNA packaging vesicles. In these vesicles, the structural proteins are integrated, a process necessary for their transport into the cell, mainly through the interaction of the E protein and prM with the Golgi apparatus28,31,32. At the same time, ZIKV generates modifications in centrosomes to reorganize microtubules and facilitate their transport and intracellular propagation33,34. Subsequently, for viral release into the extracellular environment, it was described that ZIKV can induce a process of apoptosis mediated by autophagy, processes of degranulation of viral RNA packaging vesicles, or processes of exocytosis34. The NS5 viral protein antagonizes the type I interferon response to favor viral dissemination. This leads to proteasomal degradation of STAT2 (a transcription factor that generates chain responses of the immune system), allowing ZIKV to infiltrate the lymphatic and circulatory system, which leads to the dissemination of the virus throughout the body and the development of clinical manifestations (Fig. 1B)30,35.
ZIKV transmission can be vector-borne or non-vector-borne1. Vector-borne transmission occurs when the virus infects the host through mosquito bites36. This explains the sylvatic transmission cycle, where non-human primates and endemic mosquitoes (enzootic vectors) are involved, as well as human-mosquito-human transmission in urban and suburban regions1,37. On the other hand, the mechanisms of non-vectorial infection that has been described are sexual38, vertical39, perinatal40, blood transfusion, and organ transplantation41, as well as contact with body secretions such as tears, saliva, urine, or sweat42.
Vertical, maternal-fetal transmission of Flaviviruses is unusual. It has been proposed that these viruses follow different pathways that vary according to gestational age and the route of maternal infection (vectorial or non-vectorial) to invade and replicate viral proteins in fetal tissue43,44.
Pathophysiology
ZIKV has a strong tropism to ectodermal derivatives, which confers greater dissemination potential with a wide variety of clinical manifestations and specific alterations according to the infected tissue35,45. It has been reported that ZIKV presents neuronal tropism and towards other organs, such as the liver, kidney, heart, spleen, testicle, and ovary since viral RNA has been found in these tissues30,46,47.
ZIKV tropism is mediated by type I and III interferon-stimulated genes, which induce signaling for the production of membrane proteins AXL and Tyro-3, members of the receptor tyrosine kinase-like protein family, which are expressed mainly in neuronal progenitor cells and play an important role in embryonic developmental homeostasis. In addition, the TIM1 glycoprotein, which interacts with ZIKV, has been found in multiple target organs, such as Hofbauer cells or placental macrophages, endothelium, and cytotrophoblast30,47.
Moreover, detection of ZIKV RNA in fetal tissues has also been reported in the umbilical cord, placental cells such as macrophages, amniotic fluid, and brain, as well as in tissues from spontaneous abortions of first and second-trimester human fetuses, mainly in placenta and brain8,30,47. In vitro studies suggest that viral replication occurs mainly in Hofbauer cells, trophoblast cells, and fetal endothelium48-50.
Vertical transmission of ZIKV can develop through the interaction of the virus in maternal blood or uterine fibroblasts with embryonic cells35,51. For this, two hypotheses are considered: direct transfer or placental mediated response on placental precursor tissue such as trophoblast, chorioamniotic villi and membranes, Hofbauer cells, umbilical cord endothelial cells, and amniotic epithelial cells44,50-52. The direct transfer theory stipulates that viral contact occurs within the first 10 weeks of gestation through the presence of ZIKV in maternal blood or uterine fibroblasts, thus infecting embryonic precursor cells of neuronal tissue due to its neurotropism. On the other hand, the theory of placental response can be considered complementary to the pathophysiology since the inflammatory response caused by ZIKV infection produces a disruption of placental signals that mediate neuronal development and changes the profile of inflammatory markers in fetal organs, which eventually generates the clinical manifestations depending on the specific tissue affected49,52-54.
According to the CDC, approximately 5% of pregnant patients with maternal ZIKV infection either lose the pregnancy or develop birth defects50,51. Gestational age and host genetic variation are important determinants of placental infection and immune system function35. In addition, infection acquired during the first trimester increases the risk of developing CZS in the embryo51,55. Statistically, infection in the first two trimesters is associated with severe alterations in target organs such as the brain, eye, and male and female genital tract; however, infection in any trimester of pregnancy is associated with adverse fetal outcomes35,55-57.
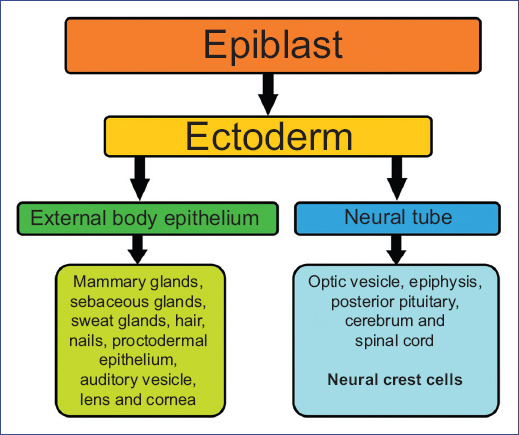
During the 3rd week of embryonic development, gastrulation and, thus, organogenesis begins. The external epithelium of the body and the neural tube are formed from the ectoderm. The external body epithelium gives rise to organs and structures that are in contact with the outside world (e.g., sensory epithelium of the ear, nose, and eye, epidermis, skin, nails, mammary, sweat, and sebaceous glands), anterior pituitary, and tooth enamel. At the same time, from the neural tube, the components of the nervous system are formed from the neural plate (notochord-induced thickening of the ectoderm) and neural crest cells (NCC) (Fig. 2)58,59.
NCCs undergo an epithelial-mesenchymal transition for their active movement and migration into the mesoderm50, directed by the expression of the bone morphogenetic protein, WNT signaling pathways, and by fibroblast stimulating factor 8 expressed by the mesoderm. In addition, they are regulated by the expression of cell adhesion molecules and extracellular matrix molecules (fibronectin, laminin, and type IV collagen), filopodia, guidance molecules (neuropilin/semaphorin), and by planar cell polarity. It should be noted that NCCs can be differentiated by prior programming and by interaction with nearby tissues59. NCCs are divided into three regions for their study: cranial, circumpharyngeal, and truncal, each with specific derivatives according to its region59. NCCs contribute to the formation of the peripheral nervous system, meninges, melanocytes, odontoblasts, medullary chromaffin cells, and a large part of the connective tissues that form the cervical and craniofacial territory, including bone, cartilage, and muscle tissue60. This is why an agent with ectodermal tropism can present diverse clinical manifestations61.
Clinical, embryonic, and fetal manifestations of CZS
The clinical features of CZS are a consequence of direct neurological involvement and intracranial volume loss, causing structural, and functional alterations4,62,63. Structural alterations include cranial morphology, cerebral and ocular anomalies, congenital contractures, and mainly microcephaly (Fig. 3A-C)64, while functional alterations are exclusively related to neurological impairment55,65,66.

Figure 3 Newborn with clinical features of microcephaly. Female patient at 39 weeks of gestation. A and B: frontal view. C: lateral view. Image obtained from Aviña-Padilla et al.64.
Chronic cerebral neuropathy in ZIKV-infected children consists of intracranial calcifications, typically subcortical (Fig. 4A and B), increased fluid spaces (ventricular and extra-axial) (Fig. 4C and D), cortical thinning with abnormalities in the convolutions (polymicrogyria, pachygyria, and agyria), hypoplasia or absence of the corpus callosum, decreased myelin, and hypoplasia of the cerebellum or cerebellar vermis67-69.

Figure 4 CT scan of newborn with severe microcephaly. A: profound craniofacial disproportion, corpus callosum (short white arrow), brainstem (long white arrow) and cerebellar hypoplasia (short black arrow), enlarged cisterna magna (long black arrow). B: calcifications in frontal lobe. C: severe ventriculomegaly. D: increased thickness of pachymeninges. Image obtained from de Fatima Vasco Aragao et al.68.
Calcifications have also been identified in the basal ganglia and brainstem. Ultrasound or magnetic resonance imaging (MRI) studies can detect these brain abnormalities during the prenatal period. In cases of microcephaly, damage of the central nervous system caused by ZIKV occurs by direct and indirect cellular injury through various pathways such as apoptosis, regulation of the immune response, ubiquitination, and viral replication, mostly in neuronal progenitor cells35,70. This apoptotic capacity may explain the alterations in the embryonic neurodevelopment of infected products. In addition, experiments have been reported in animal models, where infection in postnatal products causes dysfunction of cell death pathways, decreased proliferation of stem cells in the periventricular zone, and disruption of corticospinal pyramidal neurons71,72. These are not the only factors contributing to microcephaly caused by ZIKV; NCCs are also affected by this virus. Consequently, they produce pro-inflammatory cytokines that induce apoptosis via the paracrine pathway affecting neuronal progenitor cells35.
Neurological alterations caused by ZIKV infection include hypertonia, hypotonia, spasticity, hyperreflexia, severe irritability, and seizures. Some patients with confirmed or probable infection present fetal disruption sequence phenotype, characterized by severe microcephaly, marked craniofacial disproportion, occipital bone prominence, altered hair implantation, short neck, redundant nuchal and cranial folds, retrognathia, contractures, and multiple arthrogryposes73,74.
In the eyes, viral RNA has been detected in the cornea, optic nerve, and neurosensory retina. The most frequent ocular structural anomalies are, in particular, microphthalmia, coloboma, congenital cataracts, and intraocular calcifications. Likewise, cases of chorioretinal atrophy and retinitis pigmentosa have been reported, generally affecting the macular region and producing atrophy of the optic nerve75.
In the male reproductive tract, the infection damages spermatogonia and Sertoli cells, destroys testicular architecture, decreases sperm motility, and thus reduces fertility76. In parallel, in the female genital tract, viral RNA has been reported in the cervical mucosa up to 11 days after the onset of symptoms. In vitro studies showed that uterine fibroblasts have increased susceptibility to ZIKV, contributing to fetal developmental damage35,77.
On the other hand, congenital contractures of one or multiple joints (arthrogryposis multiplex congenita) have been described in fetuses and newborns with congenital ZIKV infection. The clinical picture of congenital contractures varies according to proximal or distal location, laterality, upper or lower limb, and severity, as reflected by neurological damage78,79.
Neurogenic factors affecting the corticospinal tract and motor neurons or their interactions may cause fetal motor abnormalities, resulting in decreased movements and contractures. However, the specific mechanism causing contractures in prenatal ZIKV infection is not yet fully understood80.
To date, the means of non-vectorial transmission and the pathophysiology at the molecular level of this condition are still under investigation.
Diagnosis
Due to the severe effects caused by ZIKV infection on embryonic and fetal development, it is necessary to identify risk factors and make a timely diagnosis. As has been described, CZS can present diverse clinical manifestations, both mild and severe; in addition, the clinical data presented are nonspecific since different infections can also cause them during pregnancy81. Therefore, it is important to detect pregnant patients with probable ZIKV infection through adequate prenatal screening, where all pregnant women should be evaluated to identify possible risk factors82.
Risk factors for ZIKV exposure include81-84:
Living in or having visited areas with active ZIKV transmission in the past 15 days or during pregnancy.
Having had unprotected sex in the 2 weeks before conception with a partner who has traveled or lived in areas with active virus transmission in the previous 6 months, regardless of whether or not symptomatology was present.
The clinical presentation of CZS is generally characterized by disruption in brain development, both embryonically and at the fetal level20,85, characterized by direct neurological disturbance followed by the collapse of the fetal cranial vault due to decreased intracranial hydrostatic pressure4,62,63.
For its study and diagnosis, PAHO has typified CZS under the following criteria86:
A case of congenital syndrome suspected to be associated with ZIKV infection is determined when the live newborn presents:
Microcephaly, whose occipitofrontal head circumference measurement is below the third percentile according to standard growth charts for age, sex, and gestational age at 24 h after birth.
Maternal history of residence or travel to an area with circulation or suspected circulation of ZIKV.
Unprotected sex with a partner with a history of residence or travel to an area with ZIKV circulation or suspected ZIKV circulation.
A case of congenital syndrome probably associated with ZIKV infection is determined when the live newborn meets the criteria for a case of congenital syndrome suspected to be associated with ZIKV infection and with any of the following features:
Intracranial morphological alterations diagnosed by any imaging method, excluding other known possible causes.
Maternal history of having presented with exanthema during pregnancy.
A case of congenital syndrome confirmed to be associated with ZIKV infection:
When the live newborn of any gestational age meets the criteria for a case of congenital syndrome suspected of being associated with ZIKV infection and in whom ZIKV infection has been laboratory confirmed, regardless of the detection of other agents.
Infection by vertical transmission can occur in any trimester of pregnancy, regardless of whether the mother has symptoms or not20,55,59,60. However, not all products exposed to ZIKV become affected. It is estimated that 70-80% of exposed products do not present alterations suggestive of ZIKV infection. Of the 20-30% who become infected, only 5-14% develop CZS. On the other hand, about 4-7% culminate in fetal loss; the rest are asymptomatic20.
The general malformations associated with CZS are81:
Severe microcephaly, where the skull has partially collapsed.
Decreased brain tissue with calcifications in the subcortical region.
Damage of the fundus, manifesting with macular scarring and focal retinal pigmentary staining.
Congenital contractures such as clubfoot (talipes) or arthrogryposis.
Congenital hypertonia limiting body movement shortly after birth.
It should be noted that microcephaly caused by ZIKV is diagnosed under the following parameters81:
Defined dongenital microcephaly:
For live births:
Occipitofrontal circumference at birth less than the 3rd percentile for gestational age and sex within the first 2 weeks of life.
For stillbirths and elective terminations
Occipitofrontal circumference at birth less than the 3rd percentile for gestational age and sex.
Possible congenital microcephaly
For live births
Occipitofrontal circumference less than the 3rd percentile for age and sex after 6 weeks of age.
For all pregnancy outcomes
Microcephaly diagnosed or suspected by prenatal ultrasound in the absence of available postnatal occipitofrontal circumference measurements.
The imaging methods for CZS diagnosis are ultrasonography (USG), computed tomography (CT), and MRI87. It is important to remember that during pregnancy, ultrasounds should be performed every trimester for fetal and maternal risk screening during prenatal control visits. Likewise, during the intrauterine stage, it is also advisable to use USG and MRI; while in the extrauterine stage, CT can be performed82,88.
Cranial alterations such as microcephaly and intracranial calcifications can be identified mainly at the end of the second and beginning of the third trimester89. On the other hand, images taken by CT or MRI can identify some of the findings that have been described in patients with CZS, such as intracranial calcifications, ventriculomegaly, increased extra-axial fluid, polymicrogyria (alterations of neuronal migrations resulting in excessive cortical folds and shallow sulci), reduction of brain parenchymal volume, cortical atrophy or malformation, hypoplasia of the cerebellum or cerebellar vermis, delayed myelination, and hypoplasia of the corpus callosum40,89-91.
In addition, laboratory diagnosis of CZS should be made on clinical suspicion and identification of risk factors by molecular testing to confirm or rule out the presence of ZIKV, such as real-time polymerase chain reaction or time-dependent neutralization of antibodies (NNT), with blood samples from both the newborn and the mother, or embryonic annexes such as the umbilical cord or placenta, to prevent possible cases of CZS92,93. Detection of immunoglobulin (Ig)M antibodies is possible by enzyme-linked immunoadsorbent assay and immunofluorescence in cerebrospinal fluid samples or by amniocentesis73,86,93. IgM antibodies can be detected in serum from the 5th or 6th day after symptoms onset, and a positive serology requires a positive NNT test to confirm infection. For this purpose, it is important to strictly follow-up prenatal and postnatal control, both for the mother and the newborn40,75.
Laboratory criteria for ZIKV infection in pregnant patients are as follows. For confirmed cases, virus isolation in a clinical specimen (blood/urine), nucleic acid detection in a clinical specimen (blood/urine), and detection of NNT in IgM-positive specimens. For probable cases, the presence of IgM antibodies, not confirmed by NNT in a serum sample, seroconversion of virus-specific IgG antibodies, or a four-fold increase in titer between samples taken in the acute and convalescent phase, the first serum is collected at the onset of the disease, and the second 10-14 days later. Furthermore, the detection of NNT in samples with negative IgM and positive IgG markers73. When congenital infection is suspected, it is advisable to perform laboratory tests to determine the presence of cytomegalovirus, herpes simplex, rubella, human immunodeficiency virus, toxoplasmosis, and syphilis infection to rule out other possible etiologies54,69.
Treatment
Given the severe alterations caused by CZS, there is no specific treatment, and therapeutic measures are symptomatic, aimed at maintaining an adequate hydric status for the patient, as well as the use of analgesics and antipyretics. At present, some specific antiviral treatments and the development of anti-Zika vaccines are under study20,35,73,94.
Patients with SCZ require constant monitoring, multidisciplinary care, referral to early intervention and stimulation centers, and family counseling20. Therefore, preventive measures are of major importance to avoid cases of CZS.
Preventive measures
According to PAHO and WHO, the best way to prevent the infection of communicable diseases is to control their vectors. Therefore, it is recommended to increase efforts to implement effective strategies to reduce vector density, mainly of the transmitting mosquito, which is widely distributed in the American continent, and the danger of exposure increases due to the emerging risk of population movement and migration95.
In countries without local cases of ZIKV infection, it is recommended that patients with suspected ZIKV infection be tested for the virus to identify the circulating viral strains, the appropriate characterization of the outbreak, and the implementation of an adequate response. In countries with local cases of ZIKV infection, it is recommended to monitor the geographic spread of the virus to delimit the affected area, assess the clinical severity and public health impact, identify risk factors associated with ZIKV infection, and identify circulating ZIKV lineages. Any changes detected through surveillance should be promptly reported to the national prevention and control authorities to ensure that appropriate action is taken on time73,95,96. It is also necessary to take personal preventive measures, including wearing appropriate clothing (cotton and neutral colors) that covers most of the body (long-sleeved shirts, pants, socks, or caps, especially during peak mosquito activity hours). It is recommended to use mosquito nets on windows, doors, and at night, on the child's bed or crib. Furthermore, use mosquito repellents containing diethyltoluamide, picaridin, or icaridin according to the product manufacturer's instructions. In the house, look for and destroy possible sources of mosquito breeding sites by avoiding accumulations of stagnant water. For couples who wish to conceive, and either partner has traveled to high-risk areas, it is recommended that pregnancy be postponed for at least 8 weeks after the onset of symptoms or last possible exposure to the virus for women (symptomatic or not) or at least 6 months after the onset of symptoms or last possible exposure to the virus for men (symptomatic or not). Sexual partners of pregnant women returning from areas with local ZIKV transmission should maintain barrier-protected sex throughout pregnancy95,96.
In conclusion, CZS is a pathological entity of wide distribution and easy transmission that can produce severe affectations. Its clinical presentation varies from asymptomatic to severe alterations that compromise the quality of life and even the course of life. The main neonatal clinical manifestations are microcephaly, ventriculomegaly, intracranial calcifications, ocular alterations, and congenital contractures. Its diagnosis is complex due to the variety of its clinical manifestations and its unspecificity; in addition, there is no specific treatment.
As health personnel, it is important to be constantly updated on this subject to identify risk factors, make a timely diagnosis and thus avoid both the effects during embryological development and the spread of this virus to more people in the population. Although there is no treatment or vaccine, personal prevention measures are straightforward and inexpensive, so it is essential to know them and promote them to avoid further complications. It is also important to continue with lines of research to better understand the pathogenic pathways through which it acts, optimize the diagnostic protocol, and produce specific therapeutic measures.











 nueva página del texto (beta)
nueva página del texto (beta)