Introduction
The prevalence of allergic sensitization (AS) in children is significantly variable, as shown by the International Study of Asthma and Allergies in Childhood Phase Two (ISAAC II) worldwide1,2 and other previous reports3. In those studies, a limited proportion of asthma and rhinitis symptoms would be attributable to atopy, particularly in non-affluent countries. The ISAAC II study, conducted about two decades ago, included only two centers in Latin America: Pichincha (a province of Ecuador with high rurality) and Uruguaiana in Brazil, with an AS prevalence of 19.7% and 13.3%, respectively1. More recent data in Brazil showed an AS prevalence of 46.8% in urban children (Sao Paulo and Nova Iguaçu, 2008)4 and 52.7% (Porto Alegre, 2015) in a sample of 241 children5. However, there is little current information on the prevalence of AS in low-income urban children in this region. It is likely that, as has been shown for the prevalence of asthma and rhinitis6-8, the prevalence of AS may be highly variable in South America.
This population-based study aimed to determine the prevalence of AS by skin prick test (SPT) to common local allergens and to explore its relationship with asthma and rhinitis in a random sample of schoolchildren from a low-income urban area in Santiago de Chile.
Methods
We conducted a cross-sectional study in a random sample of schoolchildren (6-10 years old) in the southern area of Santiago, the capital of Chile, in the districts of San Bernardo and El Bosque, an area with a Mediterranean climate at 575 m of altitude, and an air quality index of 72 (moderate). Both districts are low-income, with a monthly household income below USD 800. In addition, 9.5% of people are below the income poverty line, and 24.4% live below the multidimensional poverty line9.
Subjects
A sample of children aged 6-10 years (grades 1 to 3) was randomly selected from humanistic schools close to El Pino Hospital in southern Santiago, Chile; their parents completed the ISAAC questionnaire on respiratory symptoms at home10. The current prevalence of asthma and rhinitis was estimated from symptoms occurring in the last 12 months, while cumulative prevalence was calculated from positive responses to the diagnostic label (ever had asthma or allergic rhinitis). Questions included items on potential risk/protective factors for AS such as gender, tobacco exposure, maternal education, exclusive breastfeeding for at least 4 months, one or more siblings, family history of asthma, rhinitis or eczema, pets, and respiratory admissions. AS (synonymous with atopy) was defined as a positive reaction to one or more allergens in the SPT. Children with atopic or non-atopic asthma or rhinitis were those with positive or negative SPT and the presence of symptoms at any time (cumulative) or in the past 12 months (ongoing). Since the prevalence of AS in the target population was unknown, a sample size (simple random) of 377 children was estimated considering a 95% confidence interval (95%CI), a precision level of 5%, and a relative error of 5.1%.
Skin test reactivity
SPT was performed on the forearm for nine common inhalant allergens, histamine (positive control), and diluent (negative control), according to a detailed protocol described by Weiland et al.11 using the following extracts: a mixture of Dermatophagoides (D. pteronyssinus, D. farinae), cat epithelium, dog epithelium, Alternaria alternata, olive tree pollen (Olea europaea), plane tree pollen (Platanus acerifolia), (ALK-Abelló, Madrid, Spain); cockroach mixture (Periplaneta americana, Blattella germanica), (Leti, Madrid, Spain); mixed grass pollen (Festuca pratensis, Lolium perenne, Cynodon dactylon), and mixed weed pollen (Chenopodium album, Plantago lanceolata, Rumex acetosella, Taraxacum officinale) (Nelco Labs., Deer Park, NY, USA). Histamine 10 mg/ml (ALK-Abelló, Madrid, Spain) was used as a positive control. A positive skin reaction was defined as wheal size ≥ 3 mm after subtracting the size of the negative control.
The Scientific Ethics Committee, Chilean Ministry of Health, Southern Metropolitan Area of Santiago, Chile, approved the study. Full-informed and signed consent was obtained from all parents.
Statistical analysis
The prevalence of respiratory symptoms and AS was obtained by the percentage of positive responses to each question on respiratory symptoms and the proportion of positive SPT. The χ2 for trend was used to assess the effect of age on the prevalence of positive SPT, and descriptive statistics (χ2) were used to compare proportions between atopic and non-atopic children. Association between AS and gender, tobacco exposure, maternal education, exclusive breastfeeding for at least 4 months, family history of asthma, rhinitis or eczema, and pets, among others, was estimated by multivariate-adjusted logistic analysis (stepwise) and reported as odds ratios (OR) and 95%CI; p < 0.05 was considered statistically significant. Analyses were performed with medical statistics software (MedCalc version 20.014, Ostend, Belgium).
Results
A total of 545 children with a mean age of 8.3 ± 0.9 years (50.1% males) underwent the SPT, and their parents completed the questionnaire.
The prevalence of sensitization to one or more allergens in the whole sample was 25.5% (95%CI 22.0-29.3), and the difference between males (28.6%, 95%CI 23.5-34.2) and females (22.1%, 95%CI 17.5-27.4) was not significant (p = 0.35). The prevalence of sensitization increased proportionally with age. However, the linear trend of positive SPT prevalence according to age was not significant (p = 0.082): 21.7% (95%CI 21.9-29.1) in the 6-7-year age group (males 24.0% vs females 18.9%, p = 0.67); 26.9% (95%CI 20.8-34.0) in the 8-year age group (males 35.1% vs females 20.6%, p = 0.287), and 29.5% (95%CI 22.6-37.6) in the 9-10-year age group (males 30.0% vs females 29.0%, p = 0.945).
The prevalence of positive SPT to the allergens in the sample is represented in Figure 1. Additionally, the proportion of SPT-positive children with current asthma, rhinitis, and rhinoconjunctivitis symptoms is shown in Figure 2. The most frequent sensitization was to grass pollen, followed by Dermatophagoides mites, cat epithelium, olive tree pollen, and Alternaria.
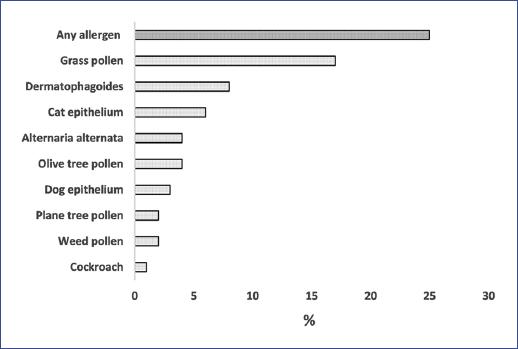
Figure 1 Proportion (%) of positive skin prick test by an allergen in low-income urban children (n = 545).
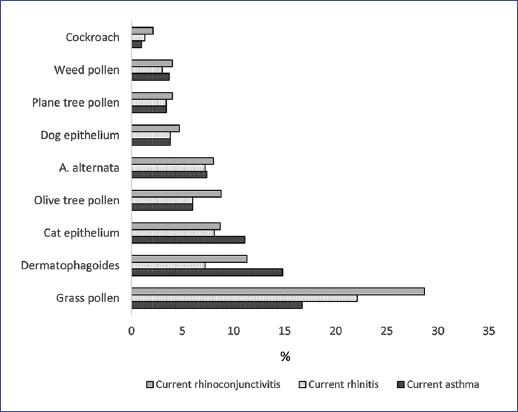
Figure 2 Prevalence (%) of positive skin prick test by current asthma, rhinitis, and rhino-conjunctivitis symptoms (n = 545).
The prevalence of asthma, rhinitis, and rhinoconjunctivitis in the whole sample and atopic and nonatopic children is shown in Table 1. In general, the prevalence of symptoms was higher than that of diagnostic labels (medical diagnosis) for the respective condition. For example, 35.5% (95%CI 26.9-44.6) of those with current wheezing reported the diagnosis of asthma, whereas 25.9% (95%CI 20.1-31.2) and 32.0% (24.5-39.1) of those with current rhinitis and rhinoconjunctivitis, respectively, reported allergic rhinitis. As shown in Table 1, the difference in current wheezing and asthma prevalence between atopic and non-atopic children was not statistically significant. Atopic children had a significantly higher prevalence of rhinitis and rhinoconjunctivitis symptoms (p = 0.017 and p = 0.019, respectively) than nonatopic children. Although the prevalence of allergic rhinitis was more elevated in atopic children, the difference was not significant. Overall, the prevalence of AS in children with asthma and rhinitis symptoms was less than 40%. In children who had never had asthma or rhinitis symptoms, the prevalence of positive SPT was 23.8% (95%CI 17.2-32.0). The proportion of children with asthma at some time who had current symptoms of rhinitis and rhinoconjunctivitis was 71.8% (95%CI 61.0-80.6) and 46.2% (95%CI 35.5-57.1), respectively. In children with current wheezing, the prevalence of symptoms of rhinitis and rhinoconjunctivitis was 66.4% (95%CI 57.0-74.6) and 42.1% (95%CI 33.1-51.5), respectively.
Table 1 Prevalence of asthma and rhinitis symptoms in atopic or non-atopic children
| Whole sample | Atopic SPT (+) | Non-atopic SPT (-) | p-value*a | ||||
|---|---|---|---|---|---|---|---|
| % | 95%CI | % | 95%CI | % | 95%CI | ||
| Wheezing (at any time) | 54.4 | (50.2-58.6) | 54.4 | (48.0-62.4) | 54.5 | (49.6-59.3) | 0.976 |
| Wheezing (ongoing) | 20.0 | (16.8-23.5) | 23.9 | (17.6-31.7) | 18.6 | (15.1-22.7) | 0.529 |
| Asthma (at any time) | 14.4 | (11.7-17.6) | 13.8 | (9.0-20.5) | 14.6 | (11.5-18.4) | 0.931 |
| Rhinitis (at any time) | 49.0 | (44.8-53.2) | 61.2 | (52.9-68.9) | 44.9 | (40.0-49.7) | 0.012 |
| Rhinitis (ongoing) | 43.4 | (39.3-47.7) | 55.8 | (47.5-63.8) | 39.2 | (34.6-44.1) | 0.017 |
| Rhinoconjunctivitis (ongoing) | 27.8 | (24.2-31.7) | 41.3 | (33.4-49.7) | 23.1 | (19.3-27.5) | 0.019 |
| Allergic rhinitis (at any time) | 12.6 | (10.1-15.7) | 15.9 | (10.7-22.8) | 11.4 | (8.7-15.0) | 0.623 |
aDifference between the proportion of atopic and non-atopic children;
*χ2-test.
CI: confidence interval; SPT: skin prick test.
AS was not associated with asthma symptoms (OR 1.37; 95%CI 0.86-2.19, p = 0.180); however, it was significantly associated with rhinitis (OR 1.96; 95%CI 1.32-2.89, p = 0.001) and rhinoconjunctivitis (OR 2.34; 95%CI 1.60-3.53, p = 0.000) symptoms.
Adjusted logistic regression (stepwise) showed no significant association between positive SPT and family history of asthma, rhinitis, eczema, pre and postnatal tobacco exposure, sex, and paternal or maternal education. Breastfeeding for ≥ 4 months was a significant protective factor (OR 0.48, 95%CI 0.26-0.78; p = 0.008) (Figure 3).
Discussion
This population-based study found that AS was present in 25% of low-income schoolchildren in the southern metropolitan area of Santiago de Chile. Of children with current asthma, rhinitis, or rhinoconjunctivitis symptoms, less than 40% had AS, which is consistent with previous findings from large international multicenter studies1-3. However, more recent studies in South America have shown a higher prevalence of AS. For example, in a random sample of 996 children, Pastorino et al. found that 46.8% had positive SPT, and 60.1% of asthmatic patients had AS4. In contrast, in the same country, Schuh et al. showed that 52.7% of the sample had AS and 61.9% and 69.2% in children with lifetime and current asthma, respectively5.
The present study found a lower prevalence of AS (25.5%) in the whole sample. However, other studies have reported lower AS rates in poor urban children. For example, a study in a metropolitan area of Indonesia found that children of low and high socioeconomic status had a prevalence of AS of 8% and 25%, respectively12.
AS figures differ significantly within and between rich countries, as has been found in Spain, showing substantial variation among centers: Almería (43%), Cartagena (23.8%), Madrid (34.5%), and Valencia (14.3%)6. An extensive nationwide study in the USA, NAHNES III (1988-1994), found a prevalence of positive SPT in children aged 6-9 and 10-19 years of 45.6% and 55.5 %, respectively13. Subsequently, in NAHNES 2005-2006, the prevalence of allergic sensitization based on serum IgE levels in children aged 6-9 years was 46.7%14. In a representative sample of 17,641 children and adolescents in Germany, the prevalence of AS was 40.2%15, while in Italy, the prevalence of positive SPT was 17.1%16.
Case-control studies in developing regions also show significant differences in AS between asthmatic and non-asthmatic children in urban areas. In Africa, 73% of Nigerian asthmatic children had positive SPT compared to 60% of the non-asthmatic subjects17, while in urban Cameroonian children, SPT was positive in 76.8% of asthmatics and 32.3% of controls18. In South America, the prevalence of AS in low-income urban children is also variable. A survey of low-income urban Chilean children found SPT positivity of 44.2% in asthmatics and 42.3% in non-asthmatic controls19. In contrast, in Caruaru (northeastern Brazil), the prevalence of AS in asthmatic and non-asthmatic children was 54.0% and 33.3%, respectively20.
Information on AS prevalence and its relationship to asthma and other allergic diseases in children in our region and other developing regions are minimal and difficult to interpret regardless of study design. However, it suggests that most asthmatic and allergic diseases in low-income children may not be attributable to atopy21 or helminthic intestinal parasitosis22. The latter supports the responsibility of other frequent environmental features prevalent in unprivileged settings, including indoor/outdoor air pollution and the burden of viral respiratory infections. These factors may be determinants of the prevalence of AS in low-income urban children and likely participate in the variability of asthma and rhinitis6.
In this group of schoolchildren, we did not find an increased risk of AS related to sex, which is consistent with other studies4,19. However, other authors have found a predominance in males22.
Regarding age, our study did not find an age-related increase in the prevalence of AS, possibly due to the narrow age range of our children (6-10 years). A birth cohort study conducted in Australia found an increase in the prevalence of sensitization from 19% at one year to 71% at 24 years of age23. Some cross-sectional studies have also shown an increase in sensitization in students from elementary (59.2%) to high school (68.2%)24.
The high prevalence of non-atopic wheezing, rhinitis, and rhinoconjunctivitis may be related to other environmental factors commonly associated with low socioeconomic conditions, such as the high burden of respiratory infections and air pollution (smog and second-hand tobacco), among others. However, the relationship between a higher rate of non-atopic asthma and rhinitis symptoms and lower socioeconomic status is unclear19,25. The high prevalence of non-atopic asthma and rhinitis in this low-income metropolitan area is consistent with other reports19. Despite this, the relationship between AS, asthma, and rhinitis has not been consistently associated with low socioeconomic status, as demonstrated in Spanish children, where 38% of wheezing cases were non-atopic, with different risk factors presenting between atopic and non-atopic children25.
In the ISAAC phase III study, performed in 2002 in the same urban area as the present study (southern Santiago), the prevalence of rhinoconjunctivitis and rhinitis in schoolchildren aged 6-7 years was found to be 13.7% and 25.3%26. Conversely, in the present study, the prevalence was 27.8% and 43.4%, respectively. Thus, although both studies are not comparable, the results suggest a significant increase in the prevalence of rhinitis and rhinoconjunctivitis symptoms in the same area of Santiago.
In this population-based study, no associations were found between AS (positive SPT) and factors related to genetic predisposition and environmental exposures, such as sex, parental and sibling history of asthma and rhinitis, pre-and postnatal maternal tobacco smoking, parental education, acetaminophen or antibiotics use during the first year of life, among others. However, breastfeeding for at least 4 months was protective for AS. In an affluent country, other authors found that parental predisposition for atopic diseases was unrelated to AS but suggested that some environmental factors play an important role in sensitizing children27.
Limitations and strengths
The limitations of the present study are mainly related to its cross-sectional design, which does not allow causality to be inferred but helps hypothesize at the population level. The sample size may be a limitation, but it is similar to previous studies on the prevalence of AS in children with asthma or rhinitis from low socioeconomic backgrounds. The prevalence of asthma symptoms is mainly based on parental reports and was not corroborated by objective measurements (lung function). However, the questionnaire has been extensively validated by ISAAC phases I and III10, and we have shown the poor diagnostic value of standard asthma tests28. Furthermore, using only nine aeroallergens may have underestimated the prevalence of sensitization. Still, this panel of allergens has been recommended for standardization11 and validated by a large international multicenter study (ISAAC II)1,11. Our results should not be extrapolated to other low-income urban areas in countries with different geography and developmental characteristics. However, the figures obtained on the prevalence of AS could be helpful for future studies in this region. In addition, this is an original study that contributes to increasing the scarce information on the prevalence of AS at the population level in low-income urban children and its relationship with current symptoms of asthma and rhinitis in Latin America.
Our study found a significant proportion of healthy children (23.8%) with positive SPT. Other regional studies have found higher figures (41%)4, while in the USA, 39% of healthy children showed AS, with African American children at higher risk of asymptomatic sensitization29. Although AS in otherwise healthy children is a recognized risk for the future development of asthma and rhinitis, no information exists in this regard in longitudinal studies in our region. Even acknowledging the importance of AS as a risk factor for the allergic disease is not synonymous with an allergic disease with no concordant clinical history30. The complexities and challenging interpretation of the findings on the relationship between AS, asthma, and allergic diseases in populations from different settings, particularly children, require further research using standardized multicenter international protocols.
In conclusion, the prevalence of AS in this group of low-income urban children was low, consistent with findings in other developing regions. The high prevalence of non-atopic asthma and rhinitis in this study could be explained by environmental exposures frequently related to low socioeconomic status. The high burden of air pollution and respiratory infections might be more important determinants than atopy for developing asthma and rhinitis in schoolchildren in underprivileged urban areas.











 nueva página del texto (beta)
nueva página del texto (beta)



