Introduction
The World Health Organization (WHO) defines child abuse as the maltreatment and neglect of children under 18 years of age that includes all types of abuse—physical or psychological, sexual, and commercial or other types of exploitation—and causes or has the potential to cause harm to health, developmental problems or endangers their survival or dignity of children in the context of a relationship of responsibility, trust or power1. However, each country may have its definition of child abuse. Even in the United States, each state has its way of classifying child abuse2.
Since a child or adolescent can be abused in different ways, the diagnosis of this condition is complex and challenging. Children may present with injuries that are the reason for the medical visit, or during the physical examination, the physician may detect damage that indicates suspicion of child abuse3. Being legal matters, physicians are responsible for studying the case and performing a complete diagnosis of abuse for notification to the prosecutor4, which is sometimes a difficult criterion to meet due to the uncertainty and difficulty of diagnosis, coupled with lack of training to perform the diagnosis and treatment, no time to complete the necessary studies, and the desire of medical staff not to be involved in a case of child maltreatment or medicolegal case5. However, health care professionals should be alert to physical injuries that are unexplained or inconsistent with the parents’ or other caregivers’ explanation or the child’s developmental status6.
Child maltreatment is a leading cause of morbidity and mortality worldwide that knows no cultural, social, ideological, or geographical boundaries. No country or community is immune, as this situation occurs in both developed and developing countries.
Each year, Child Protective Service agencies investigate more than 2 million reports of suspected child abuse in the United States2,7. The Pan American Health Organization (2017) ranks Mexico ninth in Latin America and the Caribbean in physical abuse. According to UNICEF 2010, Mexico ranks first in physical violence, sexual abuse, and homicides of children under 14 inflicted by their parents8,9. SAVE THE CHILDREN reports that seven out of every 10 children are victims of some type of violence in Mexico, and it is estimated that three children die every day due to violence10.
In 2015, at least six in 10 children aged 1-14 years experienced some violent method of discipline, and one in two children < 18 years experienced psychological aggression11.
Worldwide, an estimated 40,150 homicide deaths of children < 18 years of age occur each year, some of which are likely due to child maltreatment. However, this figure almost certainly underestimates the true magnitude of the problem, as a significant proportion of deaths due to child maltreatment are incorrectly attributed to falls, burns, drowning, and other causes12.
Based on the United Nations Convention on the Rights of the Child and other human rights standards, the following general principles need to be observed when caring for children and adolescents who may have been exposed to maltreatment, including emotional, physical, and sexual abuse and neglect13.
− Attention to the best interests of children and adolescents by promoting and protecting the safety, providing sensitive care, and protecting and promoting privacy and confidentiality.
− Address the evolving capacities of children and adolescents by providing age-appropriate information, seeking informed consent and assent, as appropriate, respecting their autonomy and wishes, and offering choices in the course of their medical care.
− Promote and protect nondiscrimination in care provision, regardless of sex, race, ethnicity, religion, sexual orientation, gender identity, ability, disability, and socioeconomic status.
− Ensure the participation of children and adolescents in decisions that have implications for their lives by soliciting and considering their opinions and involving them in the design and delivery of care.
− Demonstrate respect for caregivers to support their engagement in caregiving—when safe and appropriate—including interventions that promote nurturing and responsive caregiving.
Physical abuse consists of hitting, shaking, poisoning, burning, scalding, choking, suffocating, or other physical harm to the child. Physical damage can be caused when a parent or caregiver deliberately fabricates symptoms by inducing illness in the child14.
Healthcare professionals should consider exposure to child maltreatment when assessing children with conditions that may be caused or complicated by maltreatment to improve diagnosis/identification and subsequent care without putting the child at greater risk. Healthcare professionals should consider the following13:
− Be alert to an implausible, inadequate, or inconsistent explanation of any warning characteristics. All of these can be a sign of child maltreatment; however, none of them is sufficient evidence of child maltreatment.
− Consider child maltreatment when maltreatment is one of the possible explanations for the warning feature or is included in the differential diagnosis.
− Child maltreatment should be suspected when there is a severe level of concern about the possibility of child maltreatment.
− Exclude maltreatment when an adequate explanation for the warning features is found.
Abused children can present various injuries, from minor to life-threatening, whether parents, caregivers, or others report witnessing the act or, more importantly, the physician identifying a suspicious injury15.
In its latest review (2015), the American Academy of Pediatrics mentioned that the patient should be stabilized before further evaluation, as in any case of a child with trauma. In some cases, the patient requires a trauma response team and pediatric specialists in surgery, emergency medicine, and intensive care, depending on the severity of the trauma. After a severe life-threatening injury has been ruled out and the patient has been treated at the primary evaluation, a thorough physical examination should be performed to look for specific personal injuries and certain injury patterns that may be suggestive of abuse. However, few personal injuries are known to be pathognomonic16.
The guidelines for the evaluation of suspected child physical abuse propose several steps to complete the review of these cases, including laboratory and image tests, some of them mandatory, such as complete blood count (CBC) and nutritional status assessment, and others specific to the patient’s injury, such as head or abdominal computed tomography17.
Studies have reported that most cases of child abuse remain undiagnosed. Only 10% of them are diagnosed in emergency departments, and 64% are not diagnosed at the first consultation. If the abuse remains undetected, the risk of recurrence increases by 50% and the possibility of death by 30%18-24. The different types of abuse should be prevented, and late intervention a posteriori should be avoided so as not to allow physical and psychological distress. Another reason for abuse prevention is the immense morbidity and significant mortality. Furthermore, prevention could reduce multiple long-term cognitive, physical, behavioral, social, and emotional consequences, such as brain damage, learning problems, aggressiveness, juvenile delinquency, criminal behavior in adulthood, depression, and difficulties in work, social, and personal life25. Hence the importance of early detection; to this end, we must constantly look for sentinel lesions and have standardized and validated guidelines for detecting and following abuse5,21.
The purpose of this study was to identify whether the approach to the diagnosis of child abuse is entirely performed in a tertiary-level children’s hospital in Mexico City.
Methods
We conducted a retrospective review of the clinical records of patients with a final diagnosis of child abuse (diagnosis determined by the public prosecutor’s office) according to the ICD-10 classification. We considered those clinical archives of patients admitted to the emergency department of the children’s hospital in Mexico City between 2000 and 2016. In some of these patients, there was a suspicion of possible child abuse upon arrival; however, some were admitted to the emergency department for other reasons (e.g., pneumonia or traumatic brain injury). The following demographic variables were analyzed: sex, age, history of previous illness, disability, the reason for emergency department admission, type of abuse (sexual, physical, emotional, neglect), type of family (nuclear or single-parent), presence of dysfunctional family (referred to by the social services team in the clinical history as a family whose interrelationships serve to detract from, rather than promote, the emotional and physical health and well-being of its members), socioeconomic status (high, low, middle, referred to by the social services team in the clinical history), malnutrition, types of injuries (skin, skeletal, abdominal trauma, chest trauma, traumatic brain injury), the identity of the aggressor, history of parental child abuse, presence of domestic violence, parental substance abuse, the person suspecting abuse, follow-up, and death. It was also recorded whether the specialists performed different studies and assessments for diagnosis, including CBC, coagulation tests, nutritional status evaluation, fundus examination, consultation to ophthalmology or other departments (if necessary), liver function tests, cranial computed tomography (CT), or fontanel ultrasonography (USG), amylase and lipase, general urinalysis, FAST (focused assessment with sonography in trauma) ultrasound, abdominal CT, surgical consultation, and complete bone series.
The IBM SPSS (20.0) statistical package was used. Variables measured on a nominal scale are presented in absolute and relative frequencies. For variables measured on a numerical scale, the mean and median were used as measures of central tendency.
Informed consent was requested from the Hospital directors to review the medical records, guaranteeing the privacy of the information. The internal committees of the institution approved the study.
Results
Data from medical and social work notes obtained from the files of patients suspected of child abuse after admission are described. The initial emergency department assessment and notification were provided to the prosecutor’s office, who confirmed the diagnosis of child abuse. Seventy-three patients were found between 2000 and 2016. Maltreatment occurred in a higher percentage of females (65.8%). The most affected category by age was infants (67%), followed by school-age children (19.2%) (Table 1). The most frequent type of maltreatment was physical (80%); however, other types of abuse were also found (38.3%).
Table 1 Demographic characteristics and reason for consultation
| Variable | n = 73 n (%) |
|---|---|
| Sex | |
| Male | 25 (34.2) |
| Female | 48 (65.8) |
| Age group | |
| Neonate | 2 (2.7) |
| Infant | 49 (67.1) |
| Scholar | 14 (19.2) |
| Adolescent | 8 (11) |
| Factors that can condition abuse | |
| Disability | 10 (13.7) |
| Chronic disease | 25 (34.2) |
| Family characteristics | |
| Non-integrated family | 42 (57.5) |
| Dysfunctional family role | 52 (73.2) |
| Classification of socioeconomic level | |
| I-II | 72 (98.6) |
| III | 1 (1.4) |
| Parental drug abuse | |
| None | 18 (25) |
| Alcoholism | 22 (30.6) |
| Smoking (Tobacco) | 14 (19.4) |
| Both | 17 (23.6) |
| Other drugs | 1 (1.4) |
| Family history of violence | 26 (35.6) |
| History of parental child abuse | 18 (24.7) |
The factors frequently predisposed to child abuse in the population studied were chronic disease (34.2%) and disability (13.7%). Of the 73 patients, 46.6% were first-born children.
The frequency of other variables was as follows: dysfunctional family (73.2%), history of family violence (35.6%), low socioeconomic level (86.3%), parental alcoholism (30.6%), and history of child abuse during childhood (24.7%) (Table 1).
In most cases (49), the mother brought the child for consultation. Unfortunately, the medical records did not report in 41 patients (56%) who the aggressor was, while in 13% of the cases, the father was the perpetrator, as documented in the records.
In most patients, physicians were responsible for identifying or suspecting child maltreatment, followed by mothers in 16% of cases (Table 2).
Table 2 Distribution of responsibilities
| Variable | n = 73 n (%) |
|---|---|
| Person who brought the child for consultation | |
| Mother | 49 (67.1) |
| Uncles | 7 (9.6) |
| Grandparents | 5 (6.8) |
| Orphanages | 5 (6.8) |
| Both parents | 3 (4.1) |
| Paramedics | 2 (2.7) |
| Father | 2 (2.7) |
| Person who suspected the abuse | |
| Medics | 49 (67,1) |
| Mother | 12 (16.4) |
| Other relatives | 4 (5.5) |
| Psychology | 4 (5.5) |
| Father | 3 (4.2) |
| Teacher | 1 (1.4) |
| Person responsible for the aggression | |
| Unidentified | 39 (53.4) |
| Mother | 12 (16.4) |
| Father | 10 (13.7) |
| A third person | 7 (9.6) |
| Other members of the family | 3 (4.1) |
| Stepfather | 2 (2.7) |
Regarding the person who brought the child to the consultation for examination after the maltreatment, in 67% of the cases was the mother, followed by uncles and aunts (9.6%), grandparents (6.8%), both parents (4.1%), and, less frequently, the father (2.7%). Other persons who identified or suspected child abuse included the house staff (6.8%) and paramedics (2.7%).
As for a reason for consultation on admission to the emergency department, suspected child abuse was found in 21.9% of medical records, followed by traumatic brain injury (16.4%), sexual abuse (11%), bone fractures (11%), malnutrition (11%), altered mental status (9.6%), polytrauma (4.1%), suspected poisoning (2.7%), community-acquired pneumonia (1.4%), cardiorespiratory arrest (1.4%) and other causes (16.4%) including sepsis, soft tissue infection, tracheal injury, urinary tract infection, foreign body ingestion, or myopathy under study.
Regarding mandatory studies in cases of child abuse, we found in medical records that 100% of the patients underwent CBC and nutritional status study, 43% underwent coagulation tests [thromboplastin time (aPTT), prothrombin time (PT)], and 8% underwent ophthalmological consultation; however, no patient underwent complete bone series (Figure 1).

Figure 1 The mandatory exams have been incomplete regarding patient evaluation due to the lack of coagulation tests, ophthalmological consultations, and X-rays. When abdominal and cranial CT scans were required, they were performed in 100% of the cases. On the contrary, this was not the case for thoracic lesions since only one-third of CT scans were performed. CT, computed tomography.
According to the written medical records, the hospital followed up in 67% of the 73 cases after diagnosis. Unfortunately, in 4% of the cases, the injuries were so severe that they resulted in death.
Discussion
Our findings show that more than half of the patients were female. According to previous literature, boys experience slightly higher rates of physical abuse than girls, and, overall, adolescents are more likely to be physically abused than other children2. Moreover, in this study, infants were the most affected age group. International studies reveal that approximately 3 out of 4 children aged 2 to 4 years regularly suffer physical punishment or psychological violence from their parents and caregivers. Furthermore, 1 in 5 women and 1 in 13 men report being sexually abused as children12.
Previous studies have reported that physicians miss the opportunity to perform abuse identification and intervention up to 60% of the time2. The medical records included in this study show that 83% of the patients had a history of prior consultation for a violent injury, which may reflect the lack of suspicion and protocol initiation in these patients in previous visits to a medical service, resulting in delayed management and treatment.
In the reform of the Ley General de los Derechos de Niñas, Niños y Adolescentes (General Law on the Rights of Children and Adolescents)—published in the Diario Oficial de la Federación (Official Gazette of the Federation) in January 2021—Article 12 stipulates that “It is the obligation of any person who knows cases of children and adolescents who suffer or have suffered, in any way, a violation of their rights, to immediately inform the competent authorities, so that the corresponding investigation can be followed and, if necessary, the appropriate precautionary, protection and comprehensive restitution measures can be implemented in terms of the applicable provisions”26.
This study shows that the most frequent type of child abuse was physical (80.8%), followed by sexual abuse. It is imperative to consider these data, as previous studies show that physical and sexual abuse are the two types of abuse with the most severe long-term adverse effects. For example, Mass et al. (2008) reported that physical abuse in childhood is the type of violence most strongly associated with aggressive and violent behaviors in adulthood27. This type of phenomenon will result in a generational transmission of violence that can be prevented.
The literature reports the presence of sentinel injuries (hematomas, oral cavity injuries, or fractures) in 25% of patients and one-third of patients with head injuries due to maltreatment28. In this study, half of the patients had injuries not explained by the kinematics of the trauma or condition at the time of consultation. Consistent with other studies, dermal lesions were the most frequent in our population. Hematomas, bites, burns, and injuries with specific pattern objects were the most frequent injuries. Craniocerebral trauma was present in 23% of the patients, the first cause of death after physical abuse29. Fractures were present in 19% of the cases at consultation.
Rib fractures are strongly associated with physical abuse. A positive predictive value for abuse of 85% has been reported from the combination of any three of the following: rib fractures, subdural hematoma, brain parenchymal injury, or retinal hemorrhages29. Thoracic contusions are common, although they were recorded in only six patients in this study. Although abdominal injuries are a severe form of physical abuse and usually represent the second leading cause of death30, injuries to internal organs were infrequent in this study.
Given the wide variety of presentations of physical abuse, a systematic approach to the arrival of a patient with sentinel lesions or suspected child abuse in the emergency department is essential. Unfortunately, there are no precise algorithms in the emergency department defining the steps to follow in managing patients with suspected physical abuse, or at least there are none formally.
For example, suppose a patient arrives with polytrauma or is unstable. In that case, this patient should be treated according to the critical condition as any other patient with polytrauma, without neglecting the specific studies for suspected child abuse.
Any first contact area or emergency department should have an algorithm that includes the studies to be performed on all patients suspected of abuse: CBC, coagulation tests, complete bone series, fundus examination, nutritional status, and the mandatory initial ophthalmology and psychology evaluations. Also, the case should be reported to the maltreatment clinic if the institution has one, to the social work department, and the Public Prosecutor’s Office (MP, for its Spanish acronym). It should be considered that the MP in Mexico determines the diagnosis of child abuse and, therefore, is in charge of deciding whether or not the child is returned to the custody of the family.
No written evidence was found in this study that all the studies mentioned above were performed. Only the CBC and nutritional status assessment were documented in writing in 100% of the cases.
In cases with head trauma due to maltreatment, cranial CT (mandatory study) or USG of the fontanel was reported in 19 patients, although the diagnosis of head trauma at admission was only reported in 12 patients. Unfortunately, there is only a written record of the performance of fundus examination in six patients who received ophthalmologic consultation.
There are clear indications for bone series30, including obvious or suspicious injuries in children under two years of age, such as bruises or contusions, oral injuries, injuries not consistent with the history provided or the mechanism of injury, infants with a sudden unexplained death, infants with intracranial injuries, and in siblings under two years of age and twins of infants and toddlers who have been abused2. The projections included in the bone series are anteroposterior (AP) and lateral radiographs of the skull with optional Towne projection, AP and oblique of the thorax, AP of the abdomen, AP and lateral of the cervical, thoracic, and thoracolumbar spine, AP of the arms, forearms, femur, and lower extremities, posteroanterior (PA) of the hands and dorsoplantar (DP) of the feet, all of which should be repeated two weeks after the first bone series, as this will increase the identification of fractures by 25%. In the review of these records, reference was made to the performance of a chest X-ray in five patients; however, no written evidence was found of the complete bone series in the rest of the patients, much less of its repetition.
According to the American Academy of Pediatrics, the extent of diagnostic studies depends on several factors, including the severity of the injury, the type of injury, the age and developmental status of the patient. In general, a more comprehensive diagnostic approach is necessary for more severe injuries and at younger ages. There are different management algorithms or guidelines in the case of patients with suspected maltreatment, among which are the NICE guidelines, the Clinical Report of the American Academy of Pediatrics elaborated by the report of the Commission to Eliminate Child Abuse and Neglect Fatalities, or in Mexico, the CENETEC clinical practice guidelines. Unfortunately, these guidelines have not been updated since 2009, have 11 algorithms, and are not standardized. Therefore, given these findings and after reviewing the current literature, we propose an algorithm for managing and diagnosing patients with suspected child abuse in the emergency department (Figures 2 and 3) to reduce the high percentage of undiagnosed and untreated cases.

Figure 2 Initial steps for the evaluation of patients with suspected child physical abuse. These initial studies and steps are mandatory.
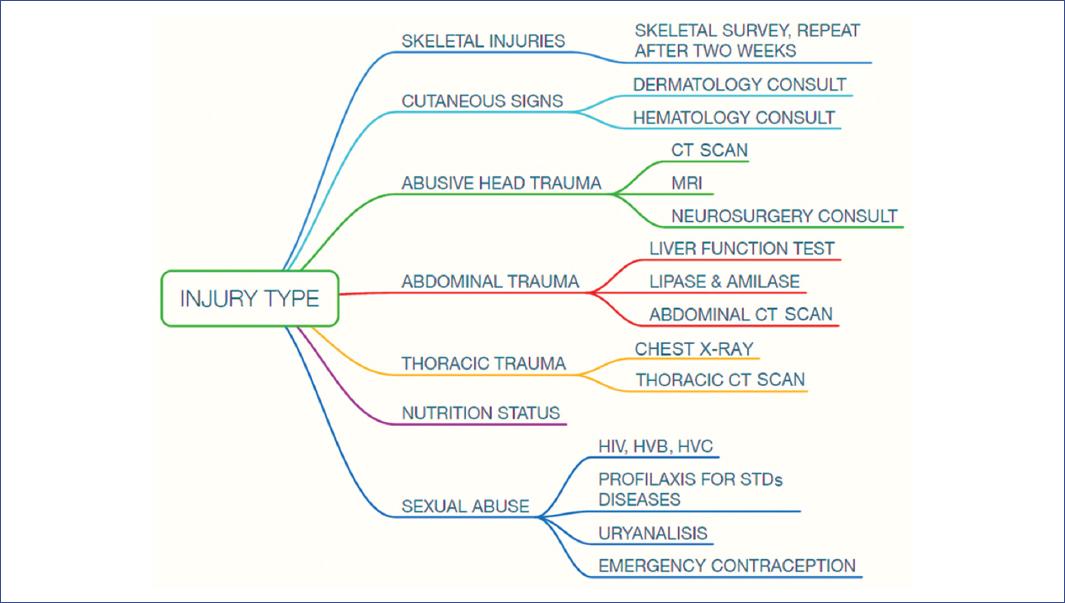
Figure 3 Assessment and studies to be expanded according to the clinical presentation data of the patient with suspected child physical abuse.CT, computed tomography; MRI, magnetic resonance imaging; HIV, human immunodeficiency virus; HVB, hepatitis B virus; HCV, hepatitis C virus; STD, sexually transmitted diseases.
In this study, the population of children diagnosed with child abuse seen in the emergency department over ten years was 73 patients. Despite being one of the most frequent pathologies in the country, the number of cases found and reviewed was small. One of the study’s limitations is a bias in the number of patients evaluated for child abuse—because our institution is a tertiary level health care center with strict selection criteria for admission, with a chronic population with high comorbidities. Therefore, we consider that child abuse is more frequent in other first and second-level hospitals.
As this was a retrospective study, specific information was impossible to obtain, leading to other biases, implying another study limitation. In addition, in years after those referred to in this study, paper medical records were changed to electronic. Finally, retrospective follow-up is difficult as there are not always notes or reports of the assessments or interpretations made, as in the case of radiographs. Ultimately, the law establishes that the protection of physical medical records is only five years, which prevents an accurate assessment of whether a complete approach to patients was made after they arrived at the emergency department.
Child maltreatment is a frequent and severe problem that leaves short- and long-term sequelae and affects the future health of the individual and the offspring. Healthcare professionals are privileged to identify patients with risk factors and detect signs of maltreatment.
Therefore, tools that offer speed and simplicity in addressing child abuse are needed in all settings where pediatric medical care and consultation are provided to significantly decrease the number of missed diagnostic opportunities in the future.
The correct and timely intervention of physicians is necessary in child abuse cases. As these are legal cases, it is essential to know the elements of the laws of each country to avoid obstacles in the management of each abused patient.











 nueva página del texto (beta)
nueva página del texto (beta)


