Introduction
Ocular trauma is one of the leading causes of permanent visual impairment and monocular blindness in children, significantly impacting the patient's development and quality of life1,2. The annual incidence of severe eye trauma in children is 8.85 to 15.2 cases per 100,000 inhabitants, although the frequency varies by location3. Most children with eye trauma had a normal vision before the accident4.
Today, eye trauma is a global public health problem. The risk of eye injury in children is higher in countries with lower levels of education, such as Mexico and other Latin American countries, where there is little health promotion in accident prevention5.
As this is a potentially preventable event, it is imperative to identify its characteristics and aim for prevention. The purpose of this study was to describe the clinical characteristics and functional outcome of severe eye trauma in patients ≤15 years of age who were admitted during one year to the Pediatric Emergency Department of the Hospital Civil de Guadalajara Fray Antonio Alcalde, located in western Mexico.
Methods
We conducted a retrospective, single-center, observational study, authorized by the Ethics and Research Committee of the Hospital Civil de Guadalajara, following the regulations corresponding to the Declaration of Helsinki (1964).
The study included patients ≤ 15 years of age diagnosed with severe eye trauma admitted to the Pediatric Emergency Department of the Hospital Civil de Guadalajara Fray Antonio Alcalde (HCFAA) from January 1 to December 31, 2017. This tertiary-level institution is a university hospital and a national reference center recognized for providing medical care to patients with a low socioeconomic level, in addition to patients who do not have other health care options.
Each clinical record was carefully reviewed to obtain detailed information. A database was used to extract relevant information for the study. Multiple variables were analyzed, such as sociodemographic characteristics, type of trauma, causes and circumstances surrounding the event, and the indicated treatment. Follow-up data were also collected to evaluate complications and measure final visual acuity.
Inclusion criteria
For this study, following clinical practice guidelines for ocular trauma in Mexico and other countries, severe ocular trauma included the following injuries: open ocular trauma, penetrating or perforating eye injuries, ocular rupture, chemical burns, and contusions involving the eye and adjacent tissues6. Severe ocular trauma can also be defined as a closed eye injury decreasing visual acuity to < 20/807.
Exclusion criteria
Cases that did not require hospitalization (non-severe ocular trauma), cases that met the criteria but did not consent to hospital admission, and patients with incomplete clinical records were excluded.
Trauma characteristics
The traumatic event was divided according to the circumstance in which it occurred (playing, leisure, sport, transportation, work, assault, and domestic violence); who was supervising at the time of trauma (father, mother, grandfather, none, or other), and the causative object or material (firearm, sharp object, fireworks, hand/fist, stone, animal, glass, and wood).
Classification of eye trauma
The categorization of patients and the terminology used were based on the Standardized Classification of Eye Trauma (Birmingham Eye Trauma Terminology, BETT), which classifies ocular trauma into closed and open. Open eye trauma includes ruptures and lacerations (penetrating injuries, perforating injuries, and the presence of an intraocular foreign body). Closed eye trauma includes contusions and lamellar lacerations8.
Visual acuity
For the classification of visual acuity in this study, the tenth revision of the International Classification of Diseases (ICD-10) proposed by the World Health Organization (WHO) was used. Therefore, the definition of blindness and visual impairment was classified as follows: no visual impairment (≥ 20/60), mild visual impairment (< 20/60 to ≥ 20/200), moderate visual impairment (< 20/200 to ≥ 20/400), severe visual impairment (< 20/400 to light perception) and blindness (no light perception)9.
Statistical analysis
Data analysis was performed with SPSS version 20.0 statistical software (SPSS, Chicago, IL). Data are presented as mean, standard deviation, range, and frequency. The Poisson probability distribution model was used to calculate each month's mean probability of occurrence. A c2 test was used to compare the proportions of occurrence by month. p-values < 0.05 were considered statistically significant.
Results
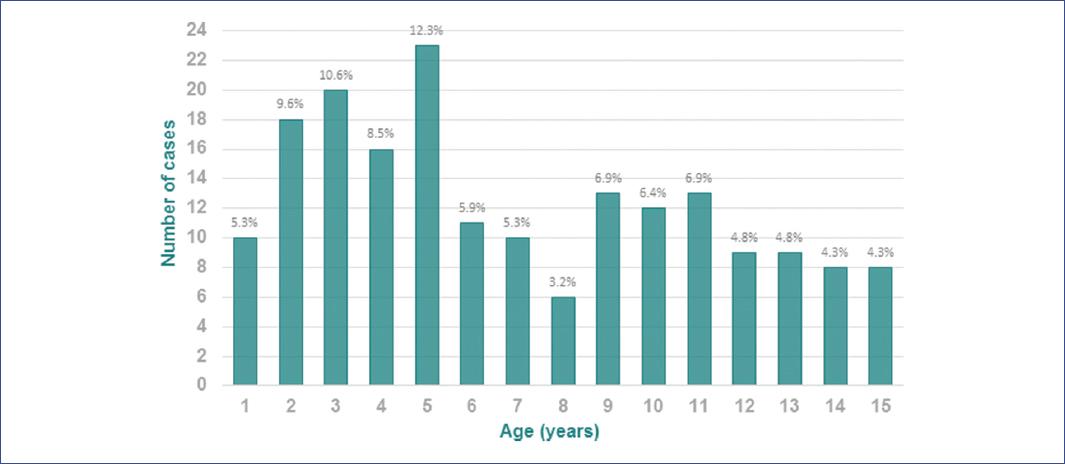
During the study period, 191 admissions with the diagnosis of severe ocular trauma were identified, of which four were excluded due to incomplete or insufficient clinical records. A total of 187 patients were included, with a mean ± standard deviation (SD) age of 6.99 ± 4.1 years. Children aged 2 to 5 years were identified as the most affected (41.1% of the cases) (Figure 1). Most of the patients were male (72.7%) with a male-female ratio of 2.6:1. Most patients (47%) resided in Guadalajara, 35% in other localities of Jalisco, and 12% in other states of the republic.
Regarding the circumstances at the time of the eye trauma, most occurred at home (78.1%), followed by accidents outdoors and on public roads (14%), at school (5.2%), and in workplace environments (2.7%). Almost half of the patients (48.1%) were unsupervised by an adult at the time of the trauma, 37.4% were supervised by the father, 8% by the mother, and 6.4% were cared for by another person.
A large proportion of patients experienced the trauma during leisure time (44.4%), 30.5% during play, 12.3% were associated with an assault, 7.4% of the cases occurred during sports, 2.7% at work, 1.6% in transportation, and 1.1% as a result of domestic violence (Table 1).
Table 1 Causal agent and circumstance of the event (n = 187)
| Injury-causing object | Patients (n) | Frequency (%) |
|---|---|---|
| Sharp object | 35 | 18.7 |
| Plant | 21 | 11.2 |
| Glass bottle | 20 | 10.6 |
| Fist | 18 | 9.6 |
| Wood | 15 | 8.0 |
| Animal | 12 | 6.4 |
| Work tools | 11 | 5.8 |
| Stone | 11 | 5.8 |
| Knife/scissors | 10 | 5.3 |
| Metallic bar | 8 | 4.2 |
| Fireworks | 7 | 3.7 |
| Toys | 6 | 3.2 |
| Pen/pencil | 6 | 3.2 |
| Falling on the ground | 3 | 1.6 |
| Shotgun | 3 | 1.6 |
| Chemical injuries | 1 | 0.5 |
| Circumstances when injury occured | ||
| Recreational activities | 157 | 83.9 |
| Work-related | 5 | 2.7 |
| Aggressions | 25 | 13.4 |
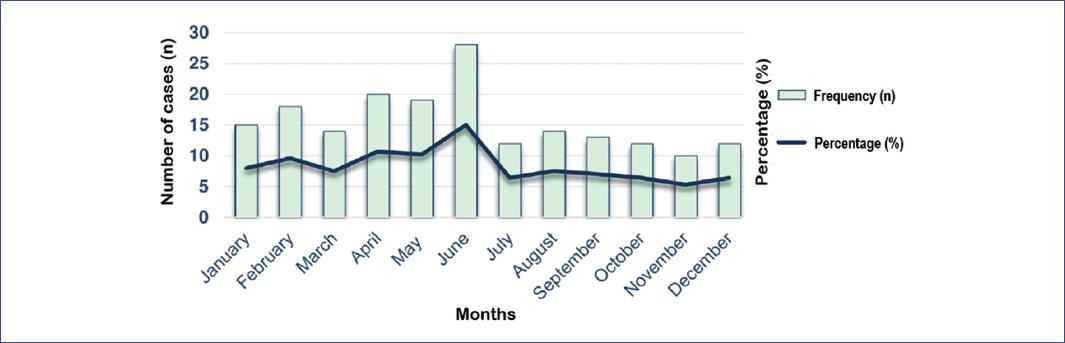
The average incidence was 15.6 cases per month during the study period, but significantly higher than expected occurrence during June, where 28 cases occurred (p = 0.002) (Figure 2). April, May, and June were identified as the months with significantly higher occurrence (35.9%) than October, November, and December (18.1%; p = 0.042).
Regarding the period between the incident and when medical attention was received in the emergency department, the average time was 36.13 ± 8.27 h (range between 1-720 h). Of the cases, 77.5% were attended within the first 24 hours after the trauma, 19.3% within 7 days, and 3.2% after one week. The mean hospital stay was 3.34 ± 3.6 days (range 0-30 days). The subsequent consultations ranged from 0-12, with a mean of 2.1 ± 2.25 consultations.
Concerning the characteristics of the ocular trauma, the right eye was affected in 95 cases (50.8%); only one patient presented bilateral ocular damage. Open eye trauma occurred in 136 cases (72.3%) and closed eye trauma in 51 cases (27.3%). For the cases of open eye trauma, penetrating injuries were the most common type of trauma (96 cases, 51.3%), followed by perforating wound (23 cases, 12.3%), ruptured eyeball (10 cases, 5.3%), and the presence of a foreign body (7 cases, 3.7%).
The most frequent diagnoses were traumatic cataract/crystalline lens dislocation (29.9%), vitreous hemorrhage (19%), lacrimal duct injury (10.2%), hyphema (5.9%), retinal detachment (5.3%), ruptured eyeball (5.3%), intraorbital foreign body (3.7%), intraretinal hemorrhage (3.2%), and retinal rupture (1.6%).
As for treatment, 11 patients received conservative management (5.8%), and 176 required surgical treatment (94.1%), even up to three surgical procedures in some patients. All procedures were performed under general anesthesia in the same hospital. Corneal wound repair was the most commonly used surgical procedure in 94 patients (50.3%), followed by corneoscleral wound repair in 42 cases (22.5%), dacryointubation in 18 cases (9.6%), vitrectomy in 7 cases (3.7%), foreign body extraction in 7 cases (3.7%), evisceration in 5 cases (2.7%) and lensectomy in 3 cases (1.6%). Thirty-four patients underwent a second surgical intervention: a lensectomy in 27, a vitrectomy in three, foreign body extraction in two, and dacryointubation in two. Twelve patients required a third procedure: 10 of them required intraocular lens placement, and two patients required foreign body extraction. The total number of surgical events was 222. Surgical complications occurred in 10% of the patients, of which 4.5% developed endophthalmitis. A total of five patients (2.7%) lost the eyeball, and three eyes progressed to phthisis bulbi (1.6%).
It was not possible to measure baseline visual acuity in 55 patients because of their young age and lack of cooperation. The baseline and final visual acuity of 132 eyes evaluated is described in Table 2.
Table 2 Visual acuity assessment before and after treatment (n = 132)
| Characteristic | Eyes (n) | Frequency (%) | Eyes (n) | Frequency (%) | ||
|---|---|---|---|---|---|---|
| Initial visual acuity | No light perception | 11 | 8.3 | Final visual acuity | 8 | 6.1 |
| < 20/400 to light perception | 32 | 24.2 | 10 | 7.5 | ||
| < 20/200 to ≥ 20/400 | 20 | 15.1 | 6 | 4.5 | ||
| < 20/60 to ≥ 20/200 | 43 | 32.5 | 80 | 60.6 | ||
| ≥ 20/60 | 26 | 19.6 | 28 | 21.2 | ||
Discussion
This study analyzed aspects related to severe pediatric ocular trauma cases in the Hospital Civil de Guadalajara. Different series have revealed that only 5-20% of eye injuries require hospitalization, so ocular trauma's high frequency and impact should not be underestimated10,11.
Consistent with other studies, our study showed that most affected children were between 2 and 11 years old and mainly were male2,4,12,13. These findings could be related to the type of activities and games performed, characterized by a certain level of aggressiveness and more physical contact, which puts this group at risk and makes them more susceptible to ocular trauma. Half of the affected patients were under 6 years of age, which considerably compromises the child's visual development and quality of life. Similar to other series that have reported that the highest number of cases occurs within 5-6-year-old,14 our series showed that the highest number of cases occurred at younger ages, from 2 years of age, with a peak at 5 years of age.
Most accidents occurred at home with everyday objects and with no adult supervision. Many of the patients were supervised by the father, with a ratio of 4.5:1 with respect to the mother's supervision, which could be related to the nature of the activities performed in the company of the father. Similar findings are reported in other series, indicating that supervision reduces the occurrence of childhood ocular trauma5.
When reporting employment-related ocular trauma or ocular trauma that occurred at a workplace, we should consider that some children were employed and others were accompanying their parents to help perform work-related activities, so the work environment is identified as a risk factor for childhood ocular trauma15. A study conducted in Africa showed that 39.3% of eye trauma was associated with child labor compared to 2.7% in our study16. Therefore, this percentage is relatively low compared to other countries with a higher proportion of child labor.
As for the objects identified as the cause of eye trauma, sharp objects (scissors, pencils, cables, screwdrivers, among others) were the most common. Other objects identified as causing the injury were wooden sticks, tree branches, and glass bottles, which increase the child's probability of eye trauma and any other type of life-threatening bodily injury.
The time between the ocular trauma and the emergency room examination was within the first 24 hours in most cases, enabling adequate treatment to be provided and reducing the probability of complications and long-term repercussions. Although not demonstrated in this case series, different studies suggest that patients receiving care > 72 hours after trauma have a worse visual prognosis and a higher risk of complications17,18.
Similar to the cases reported in a series from the Instituto Nacional de Pediatría, Mexico City, the patients came from rural areas and low-income urban regions, with half of the cases in marginalized areas and estates far from the hospital12. The same findings are observed in other series carried out in developing countries. The latter could explain that the delay in medical care is due to the time and resources needed to transport the patient14.
The higher occurrence of cases in April, May, and June suggest a variation probably related to higher temperatures and days with longer hours of sunlight during spring and summer (or school vacation periods). This variation associate the spring and summer months with a higher incidence of cases, similar to the findings of other series19.
Most studies on ocular trauma in children report a higher incidence of closed than open ocular trauma2,4,20,21. However, only patients with severe ocular trauma requiring hospitalization were included in this study, which explains the higher frequency of open ocular trauma. The high frequency of corneal lesions and its impact on visual impairment is striking, contributing to 20-30% of the indications for corneal transplant in other series22,23.
Of the total number of patients, it was only possible to determine visual acuity in 70.5%. Final visual acuity was ≥ 20/200 in 18.8% of patients, consistent with other studies24-26. However, these comparisons should be carefully reviewed since the proportion of open ocular trauma is different in each series: 47.4%, 51.7%, and 40.6%, respectively24-26. In our study, 13.6% of the affected eyes had a poor visual outcome, with a final visual acuity ≤ 20/400. Unfortunately, salvage of the eye was not possible in 4.6% of the patients.
The epidemiological profiles of ocular trauma vary according to country and age group. In adults, eye trauma occurs mainly in work areas, closed ocular trauma and the intraocular foreign object being the main types of injuries. In children, eye trauma occurs mainly at home or in play areas, especially during leisure time, open ocular trauma being the most frequent type of injury. In both cases, trauma could be preventable by supervising activities and using protective eye equipment27.
A limitation of this case series would be that patients with eye injuries admitted under different diagnoses (medical records coded as multiple trauma or head injury, among other diagnoses) were omitted, which causes the occurrence of ocular trauma to be underreported.
In this study, the highest proportion of cases occurred in males ≤ 5 years old, unsupervised, and at home. As in other studies, a large percentage of ocular trauma cases can be avoided by promoting preventive measures and raising awareness of the current situation of ocular trauma, focusing on the risks and repercussions that irreversibly affect the child's quality of life. Increased caregiver supervision and limiting young children's access to potentially dangerous objects can dramatically decrease the incidence of severe eye trauma in pediatric patients2,4,27. In alliance with pediatric organizations, it is imperative to implement educational, social programs that highlight the seriousness of the problem and promote safe environments. Prevention campaigns aimed at caregivers are crucial to avoid future accidents in pediatric patients.











 nueva página del texto (beta)
nueva página del texto (beta)