Introduction
Since the description of nitric oxide (NO) as an endothelial relaxation molecule and the demonstration of NO in exhaled air, the measurement of this compound has been used to determine the degree of airway eosinophilic inflammation1-3. According to different guidelines for asthma management, NO measurement is considered a tool for diagnosing and treating patients with this disease4-6. In 2005, the American Thoracic Society and the European Respiratory Society (ATS/ERS) made recommendations for the "online" (real-time display of NO measure) and "offline" (collection of exhaled air into a bag for delayed analysis) measurements of exhaled NO. The most standardized technique is the online method, in which the individual exhales with a flow of 50 mL/s while the device measures in real-time. However, the offline method is described as an alternative to the online method because NO is collected in a bag for later analysis using one of the following procedures: with a single exhalation maintaining a flow of 350 mL/s; breathing during constant flow against a pressure of 5 cmH2O, or breathing at tidal volume without the control of flow7.
Unfortunately, asthma in children < 5 years old is difficult to diagnose because symptoms are similar to those of other lung diseases6. Additionally, pulmonary function tests are difficult to perform correctly in this group of patients, considering that they have difficulties following the instructions to maintain the necessary constant flow for the correct measurement. Therefore, the best way to measure fractional exhaled nitric oxide (FENO) is to collect the exhaled air by breathing at tidal volume6,8. The standard way to measure FENO with the offline method at tidal volume is chemiluminescence technology. However, equipment with this technology is expensive and difficult to access. Although other devices with electrochemical technology are portable and easy to access, they are designed for online measurements9.
We hypothesize that the results of NO measurements collected at tidal volume can be similar, whether analyzed in chemiluminescence (cl) or electrochemical (eq) devices. Therefore, this study aimed to report the concordance and correlation of the results obtained by chemiluminescence vs. an electrochemical device using the offline technique collected at tidal volume in healthy children and children with lung disease.
Methods
A cross-sectional, observational, and prospective study was conducted in the Department of Respiratory Physiology of the National Institute of Respiratory Diseases (Instituto Nacional de Enfermedades Respiratorias, INER), Mexico City. It was approved by the Research and Bioethical Committee (agreement number C14-19). Children between 1-11 years of age were invited to participate and recruited by a direct invitation from the institution's outpatient clinic or by relatives of hospitalized patients. Healthy individuals or children with any pulmonary disease were included. However, children who could not wear the mask due to facial malformations, those with chest, abdominal, oral, or facial pain, those with altered consciousness, and oxygen-dependent individuals were excluded from the study. Finally, those who fulfilled the inclusion criteria but could not tolerate breathing through the mask at tidal volume were also excluded.
We administered a respiratory health questionnaire and took anthropometric measurements, including weight (kg) with a portable digital scale (Seca, model 813 and 232, Hamburg, Germany) and height (cm) with a mechanical stadiometer (Seca, model 206 and 232, Hamburg, Germany). Subsequently, the exhaled air sample for the evaluation of offline eNO at tidal volume was taken according to the recommendations of the ATS/ERS 2005 guidelines7. The purpose and procedure of the test were explained to patients and family members. If the parents agreed to allow the child to participate, we proceeded with their signature in the consent letter.
Calibration of the equipment
We used the Sievers® 280i nitric oxide analyzer (General Electrics, Boulder, Colorado, USA), a high-sensitivity detector that measures exhaled nitric oxide based on gas-phase chemiluminescence (eNOcl) reaction between nitric oxide and ozone. The equipment has a vacuum pump, which provides a vacuum of ~ 200 mL/min, that continuously extracts gas from the analyzer at a constant pressure. The limit for the measurement of nitric oxide in the gas phase is ~ 0.5 parts per billion (ppb), the sensitivity is < 1 ppb, with a range < 1-500,000 ppb, a response time of 67 ms, and repeatability of 5%.
The other equipment was the electrochemical (eNOeq) NO-Breath® (Bedfont, Harrietsham, England), which is based on an electrochemical sensor technology that reacts to the presence of nitric oxide. Its advantages are that it is portable, the detection range is 5-300 ppb, the repeatability is ± 5 of a measured value ≤ 50 ppb and ± 10 of measured value ≥ 50 ppb, and the response is given in < 10 s.
It is relevant to mention that the chemiluminescence equipment was calibrated daily by two methods. The first was zero gas calibration (NO < 1 ppb), achieved by placing a zero gas filter (which works by obtaining NO from the environmental air through a KMnO4-activated carbon filter to generate oxidation to NO2, which is absorbed by activated carbon) into the sampling line connection that goes to the equipment and opening the distal end to allow the flow. The filter is left connected for approximately 5 min to wash the sampling line of environmental air. Once the filter is placed, the device automatically calibrates to zero by measuring ppm at 0 and making a ppb adjustment with the calibration of the previous day. Calibration was also performed with a known gas concentration. For this procedure, a tank containing a gas between 10-100 ppb (usually 45 ppb of NO in balance with N2) is connected to the sampling line where the analyzer provides a flow of > 200 mL/min (generally at 300 mL/min given by the regulator). After these steps, the flow is left for approximately 5 min.
Two or three calibrations should be performed to ensure repeatability. The response factor measured in ppm should be within a range of 0.09768 to 0.1465, and the response factor in ppb should be within a range of 0.1953-0.293.
Conversely, electrochemical equipment is usually already calibrated according to the manufacturer's specifications. Therefore, it is only necessary to verify that the environmental module containing the equipment reads less than 5 ppb. Finally, the environmental reading in both instruments < 5 ppb was verified before each measurement.
Sample collection
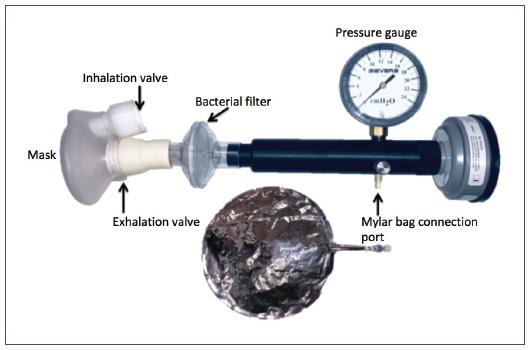
A mask with a unidirectional inhalation and exhalation valve, connected to a filter and pressure measurement system (Figure 1), was placed in patients seated with the back upright and the head slightly raised. At a tidal volume, patients were asked to breathe through the mask. Although the flow during the maneuver was not controlled, the pressure during breathing was monitored to stay above 5 cmH2O. In uncooperative children, we collected the sample at least with 2 cmH2O of pressure. After three respiratory cycles were taken to wash the dead space of the system, the valve was changed to obtain the sample in the 1.5-liter Mylar® collection bag (Sievers Instruments, Boulder, Colorado, USA). We decided to stop the process once the patient had performed five breaths at a tidal volume or when the bag was filled at least half of its capacity. In the end, samples were analyzed in less than 48 hours following the ATS/ERS 2005 guidelines7.
Sample analysis
The analysis of the samples was carried out on both devices randomly. Regarding the chemiluminescence equipment, the sample was taken according to the manufacturer's recommendations: the Mylar® bag was connected to the sampling line (which has a vacuum pressure that makes a plateau with NO value during 5 to 10 s). Subsequently, the measured values of NO were obtained. In the case of the electrochemical equipment, the Mylar® bag was connected to the device through a filter (Figure 2). Then, with the device in ambient mode, the suction pump was automatically activated, and after approximately 20 s, the sample analysis was performed. Importantly, two measurements were taken in each device, ensuring a variability of less than 10%, and the final result was formulated by the average of both measurements reported in ppb. All the samples were analyzed in less than 120 min.
Statistical analysis
Descriptive statistics were expressed as the mean ± standard deviation (SD) or median and interquartile range depending on the variables' distribution. Comparisons between both eNO devices were made using the paired Student's t-test. The correlation analysis was performed using the Spearman correlation coefficient (rsp), and the concordance correlation coefficient (CCC) was used to assess the degree of agreement between eNOcl and eNOeq. Considering two measurements for each subject, an intraclass correlation coefficient of 0.8, contrasted with an expected one of 0.5, resulted in an alpha error of 0.05, a power of 0.8, and a 20% loss. Therefore, the required sample size was calculated to be 35 tests. A p-value < 0.05 was defined to be significant, and a commercial statistical package was used to analyze the data (Stata V.13).
Results
A total of 36 children were studied, of which 24 (67%) were male. The mean (± SD) age of the study population was 6 ± 2.6 years old, with a minimum of 1 year and a maximum of 11 years; 9 (25%) of the subjects were healthy, and the rest had a history of lung disease. The most frequent lung diseases were bronchopulmonary dysplasia (12; 33.3%), asthma (11; 30.6%), suspected primary ciliary dyskinesia (3; 8.3%), and bronchiectasis not associated with cystic fibrosis (1; 2.8%). Table 1 shows the general characteristics of the population.
Table 1 General characteristics of the participants
| Female (n = 12) | Male (n = 24) | Total (n = 36) | |
|---|---|---|---|
| Age (years) | 6 (4-8) | 6 (5-8) | 6 (5-8) |
| Weight (kg) | 18.5 (14.5-24) | 20 (15-25.5) | 20 (15-25) |
| Height (cm) | 109 (100.5-120.5) | 115 (104-127.5) | 115 (102-126) |
| eNOcl (ppb) | 19.85 (15.2-22.5) | 18.55 (11.4-26.9) | 19.15 (12.2-26.2) |
| eNOeq (ppb) | 19 (15.8-22.3) | 18 (9.8-25) | 19 (11.3-24) |
Data are presented as median (percentile 25-75).
eNOcl, exhaled nitric oxide measured by the chemiluminescence device; eNOeq, exhaled nitric oxide measured by the electrochemical device.
The CCC between the two measuring devices was 0.98, with an average difference of 1.46 ± 3.5 ppb and 95% limits of agreement from -5.3 ppb to 8.3 ppb. The Bland-Altman graphs are shown in Figure 3: the agreement between the two measuring devices (Figure 3A) and the Spearman's correlation coefficient (r = 0.98; p < 0.001) (Figure 3B) The linear regression model equation for eNO estimation was eNOcl = (eNOeq·1.0718) - 0.1343 (r2 = 0.97). We decided to categorize the subjects into groups to see the concordance between the categories with eosinophilic inflammation. The CCC between devices was 0.92 in the < 20 ppb group, 0.89 in the 20-35 ppb group, and 0.94 in the group with > 35 ppb (Table 2).

Figure 3 A: Bland-Altman graph showing the agreement between both devices, the Sievers® (eNOcl) and the Bedfont® (eNOeq). CCC = 0.98. B: Spearman correlation between both devices (rsp = 0.98).eNOcl, exhaled nitric oxide measured by the chemiluminescence device; eNOeq, exhaled nitric oxide measured by the electrochemical device.
Table 2 Concordance by category according to FENO values in children
| FENO ≤ 20* (n = 19) | FENO ≥ 20* (n = 12) | FENO > 35* (n = 5) | |
|---|---|---|---|
| CCC | 0.92 | 0.89 | 0.94 |
| Mean difference± SD | -0.38 ± 1.5 | -1.5 ± 1.6 | -6.1 ± 7.6 |
| r | 0.93 | 0.96 | 0.96 |
| Limits of agreement | -3.3 to 2.5 | -4.7 to 1.7 | -2.1 to 8.7 |
*p < 0.001.
CCC, concordance correlation coefficient; FENO, fractional exhaled nitric oxide; SD, standard deviation.
Discussion
This study demonstrates that the eNO results obtained by chemiluminescence and electrochemical equipment, using the offline method and the tidal volume technique, are interchangeable. We also described the technique to analyze the samples using electrochemical equipment, which is more accessible and inexpensive.
Asthma is the most frequent chronic disease in children, and its prevalence is higher in children under the age of 5 years10. In these cases, asthma manifestations depend on the interaction between genetic and environmental factors, and it differs from person to person according to their phenotype, genotype, and endotype4,6. Asthma continues to cause high morbidity and mortality worldwide, mainly due to the absence of suspicion and difficulty making the diagnosis. This difficulty is evident in preschoolers because of their lack of cooperation to undergo a respiratory function test. Consequently, the diagnosis is based mainly on predictive indices in which pulmonary function and the degree of inflammation in the respiratory tract are not considered3.
In 2001, the ATS/ERS published the clinical guidelines for interpreting eNO measurements in adults and children, establishing cutoff points to define when inhaled steroid treatment should be administered and when it should be increased or decreased5. However, these guidelines and other studies considered only patients > 4 years of age, and the method used was the online method, where the individual must maintain a flow of 50 mL/s11-16. In 2005, the ATS/ERS made some recommendations for the standardization of measurements of eNO with the online and offline methods, and the offline measurement of eNO at tidal volume is mentioned as an alternative to the other methods described7.
By the end of the 1990s, some studies were published concerning toddlers and preschoolers with wheezing in whom eNO was measured with the offline method at tidal volume using chemiluminescence equipment. It was shown that preschoolers presented higher values of eNO during wheezing episodes (14.1 ± 1.8 ppb), which improved after steroid treatment, reducing eNO levels up to 52%17. Additionally, it was shown that exhaled air could be easily collected from these children, allowing to differentiate among asthmatic patients, those with chronic non-asthmatic cough, and healthy children8,18. As a result, these authors concluded that the offline method is easy to perform and can be executed on an outpatient basis17,18. Similar to these results, we demonstrated that the sample was easy to obtain without causing any discomfort to the children.
Moreover, several studies have reported reference values with the offline method at different respiratory flows, even in children < 2 years of age9,12,13,16,19-22. However, the main limitation to reproduce this technique is the availability of chemiluminescence equipment, which is expensive and difficult to access for most centers23. The present study demonstrates that the measurements of eNO obtained by the offline technique through breathing at tidal volume can be analyzed by electrochemical devices, and the results are interchangeable with those analyzed using the gold standard chemiluminescence equipment. This interchangeability is established based on the high concordance and correlation coefficients (CCC = 0.98, rsp = 0.97, p < 0.001), and it is important for the pediatric population because the offline method can be used in uncooperative patients. Also, we categorized to find the CCC between groups (probable eosinophilic inflammation) and obtained a value of 0.92 in < 20 ppb, 0.89 in 20-35 ppb, and 0.94 > 35 ppb; thus, both methods could identify low and high values of eNO. Equally important, using portable equipment that exists in the market could expand the spectrum of use in the clinical setting and as a good alternative for conducting epidemiological studies on a larger scale. Like other authors9,17,20,22, we used the bags recommended by the chemiluminescence equipment manufacturer (Mylar® bag) in this study, which are the typical bags made of a stretched polyester film (biaxial-oriented polyethylene terephthalate) that come with a connector and a unidirectional valve that facilitate obtaining the sample. In addition, these bags' material is the same as that used for balloons, and we consider that if it is used with another type of adapter, the cost for every measure could decrease considerably7.
Although our main objective in this study was to evaluate the agreement in exhaled nitric oxide measured offline at a tidal volume between the two devices, these results should be corroborated in patients with different clinical spectrum (e.g., patients with diseases or conditions that decrease nitric oxide and patients with very high values of it) to be used in clinical practice. A limitation of this study was that we did not control the flow, although our method can be used in noncooperative children, and additionally, the main objective was to validate interchangeability between devices.
In conclusion, the measurement of eNO by the offline method can be analyzed in an electrochemical device, and the results are interchangeable with those obtained in chemiluminescence equipment.











 nueva página del texto (beta)
nueva página del texto (beta)