Introduction
Diabetes mellitus (DM) during pregnancy may be associated with poor maternal and perinatal outcomes1. Due to improvements in medical care, offspring of diabetic mothers have higher survival rates, although a greater risk of overweight/obesity (O/O) during their lifetime. However, the pathophysiological mechanisms of these alterations have not been fully understood2.
Since O/O are among the most important nutritional problems in the world, their causes require further research as prevention can help improve the quality of life in children and even in adult life. It is necessary to identify what risk factors favor the development of childhood obesity to decrease the high percentage of children with O/O3.
DM during pregnancy is associated with increased fetal growth, possibly due to the storage of more fetal fat mass and altered hormone levels, which result in hyperglycemia, hyperinsulinemia, and a high leptin synthesis4. Pregestational DM (PDM) and gestational DM (GDM) can also modify the fetal epigenome, influencing the expression of genes that drive to accumulation of body fat or related metabolism alterations5.
Mothers with PDM have a chronic metabolic disorder, and they may present hyperglycemia since the beginning of pregnancy. Conversely, mothers with GDM develop hyperglycemia in the second or third trimester of pregnancy, but the complications found have been described as not severe6. However, not all physicians agree with this statement. It has been shown that strict glycemic control during early gestation reduces the prevalence of some complications of the mother-child binomial7. As we cannot assume that PDM and GDM have the same effects on fetal development and the same long-term outcomes in offspring, it is essential to study the effects of both conditions on the offspring of these mothers.
This research hypothesized that fetal hyperglycemia reorganizes hypothalamic centers for hunger and results in super-expression of child search for food and later in O/O. This study aimed to analyze the effect of differential distribution of body mass index (BMI) as a parameter of nutritional status in the offspring of mothers with PDM or GDM at 2, 4, 6, and 8 years of age at pediatric follow-up. Maternal and neonatal variables were analyzed, looking for possible associations with O/O.
Methods
Subjects
We designed and conducted a prospective study. Measurements of BMI were carried out at 2, 4, 6, and 8 years of age. For observations, four groups were studied: offspring from mothers with type 1 DM, offspring from mothers with type 2 DM, and offspring from mothers with GDM. A control group (CG) with infants from healthy pregnancies was also included. Inclusion criteria for mothers with DM and their infants were children from mothers with DM born at our institution and who accepted to participate in the follow-up program. Children from mothers with DM were part of the multidisciplinary pediatric follow-up of infants at high risk. The CG was formed with low-risk mother-child binomials: mothers with no history of DM, hypertension, or infections; intake of anticonvulsants, anti-depression, anti-coagulant, or other drugs during pregnancy; neither multiple pregnancies nor other alterations. Inclusion criteria for control children were no genetic syndromes, congenital malformations, severe complications at delivery or during the neonatal period, sensory or neurological sequelae, or any other. In addition, they must also belong to our pediatric follow-up clinic.
The research committee of the institutions accepted this protocol. The parents were informed of the importance of children's participation and the purposes and benefits of the research. Informed consent was requested and signed according to the Helsinki declaration.
Studied variables
Our hospital is a specialized institution in human reproduction medicine and a reference center for high-risk pregnancies. For these reasons, pregnancies complicated with DM are one of the followed conditions. The following variables were studied in mothers: diagnosis and type of DM based on the recommendations of the American Diabetes Association criteria8, age during pregnancy, insulin dependence, use of prenatal steroids for fetal pulmonary maturation, delivery method, history of morbidities, such as preeclampsia and others.
The variables studied in infants were gestational age at birth (weeks), birth weight (grams), Apgar score at 1 and 5 minutes, sex, morbidities during the neonatal period, respiratory distress syndrome, application of pulmonary surfactant, history of broncho-pulmonar dysplasia according to Northway's criteria9, neonatal hypoglycemia (capillary glycemia < 45 mg/dl), hypocalcemia (total Ca serum < 8 mg/dl in term newborns and <7 mg/dl in preterm newborns), intraventricular hemorrhage (determined by transfontanelar ultrasonography after Volpe's classification10), neonatal hyperbilirubinemia (managed with phototherapy or exchange transfusion).
Anthropometric measures
- Weight was determined in children by a certified nutritionist at every appointment (at 2, 4, 6, and 8 years of age) with standardized techniques11: during the mornings, with the child wearing only underwear. We used a Seca weight scale (Hamburg, Germany) model 703, with a capacity of 150 kg and a precision of 0.5 g, and integrated telescopic rule, model 220 (measurement range: 60-200 cm, minimum precision of 0.5 cm).
- Height was determined with the child standing erect with the back against the stadimeter, facing forward, with the Frankfurt plane parallel to the ground. Heels, spine, and occiput were supported on a rigid plane, and arms were extended along the trunk.
- BMI was calculated according to the international known equation = weight (kg)/height2 (m2). We used the Center for Disease Control tables for gender and age to classify children's data. We considered measurements as adequate when found between the 10-85th percentiles. BMI < 10th percentile was classified as low weight; BMI 86-95th percentiles were identified as overweight, and BMI > 95th percentile was classified as obesity12,13. The nutritional intervention for these children was carried out by certified nutritionists and pediatricians and was continuously verified throughout their follow-up period.
Follow-up and surveillance
We closely followed the infants' and children's food intake and exercise activities throughout the study. The infants' appointments were every 3 months during the first year of life, every 6 months in the next 5 years, and every year until 8 years of age. The parents received many academic presentations on how to monitor children's food intake and seek medical consultation in the case of illness or doubts about food intake. During the appointments, we asked the parents about food intake and exercise schedules according to age and gender and the abuse of snacks with high carbohydrates and fats. Bad habits regarding excessive consumption of candies, sodas, hypercaloric snacks intake, or sedentary lifestyle were corrected.
Statistical analysis
Continuous data were presented as means and standard deviations. The variance homogeneity test was performed with Levene's test. For comparison of means, we used the one-way analysis of variance (ANOVA) with Scheffé's post-hoc test (for unbalanced groups). Categorical variables were presented as percentages and analyzed using the Χ2 test.
For the BMI analysis, obesity and overweight were combined. Odds ratios (OR) were calculated for each group in each age period. The same analysis was performed for the low weight (< 10th percentile). A p-value < 0.05 was considered significant.
Results
Overall characteristics
From 8,993 children recruited for the follow-up, 323 (3.5%) fulfilled the inclusion criteria and were born from mothers with type 1 DM, 2 DM, or GDM, and CG. From these children, 266 (2.9%) corresponded to some type of DM during pregnancy, with the following distribution: type 1 DM, n = 95 (29.4%); type 2 DM, n = 70 (21.7%); GDM, n = 101 (31.3%); while CG was formed with 57 infants (17.6%).
Maternal variables
The mean age of mothers with DM was significantly higher than control mothers (32 ± 6 vs 22 ± 6 years, p < 0.001). The number of gestations was distributed as follows: first pregnancy (primigravida), n = 115 (35.6%); second gestation, n = 95 (29.9%); third gestation, n = 51 (15.7%); fourth gestation, n = 34 (10.6%); fifth gestation or more, n = 28 (8.7%).
Frequency of pre-eclampsia in mothers with DM during pregnancy was 27.9% (p < 0.001) and was distributed as follows: pre-eclampsia/type 1 DM, 7.1% (odds ratio (OR) 7.1; 95% confidence interval (CI) = 2-24.8, p < 0.001); pre-eclampsia/type 2 DM, 11.3% (OR 11.3; 95% CI = 3.2-39.7, p < 0.001); pre-eclampsia/GDM, 9.9% (OR 9.9; 95% CI = 2.9-34, p < 0.001). In addition, 16 mothers with DM (5%) died at some point of follow-up, most of them from the type 1 DM group (n = 9, 2.8%) (Table 1).
Table 1 Alterations in mothers with diabetes mellitus and control group
| Variable | Type 1 DM (n = 95) (29.4%) | Type 2 DM (n = 70) (21.7%) | Gestational DM (n = 101) (31.3%) | Control group (n = 57) (17.6%) | Total n = 323) (100%) | p-values |
|---|---|---|---|---|---|---|
| Preeclampsia | 27 (8.4%) | 27 (8.4%) | 36 (11.1%) | 3 (0.9%) | 93 (28.8%) | 0.001 |
| Use of prenatal steroids | 23 (7.1%) | 21 (6.5%) | 39 (12.1%) | 3 (0.9%) | 86 (26.6%) | 0.001 |
| Cesarean | 85 (26.3%) | 66 (20.4%) | 97 (30%) | 55 (17%) | 303 (93.8%) | 0.19 |
| Deceased mothers | 9 (2.8%) | 3 (0.9%) | 4 (1.2%) | 0 (0.0%) | 16 (5%) | 0.06 |
DM, diabetes mellitus.
p = χ2.
Neonatal variables
The mean gestational age at birth was significantly lower for infants of mothers with DM than the CG (32.8 ± 3.1 vs. 36.4 ± 2.2 weeks, p <0.001), and 82% were late preterm infants (32-37 weeks) (p < 0.001). Birthweight was significantly lower for children of mothers with DM than CG (1,637 ± 600 vs. 2,208 ± 518 g, p < 0.001) (Table 2). Birthweight classification showed a high frequency of eutrophic preterm infants (64.9%, n = 209), followed by hypotrophic preterm infants (15.5%, n = 50) (Table 3). Additionally, 94 infants were born by cesarean section.
Table 2 General characteristics in offspring of mothers with diabetes mellitus and control group
| Variable | Type 1 DM (n = 95) (29.4%) | Type 2 DM (n = 70) (21.7%) | Gestational DM (n = 101) (31.3%) | Control group (n = 57) (17.6%) | Total (n = 323) (100%) | ANOVA p-values |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Gestational age (weeks) | 33.1 ± 2.8 | 33.4 ± 3.1 | 32.0 ± 2.5 | 36.4 ± 2.2 | 33.5 ± 3.1 | 0.001 |
| Birthweight (g) | 1660 ± 563 | 1745 ± 690 | 1507 ± 547 | 2208 ± 518 | 1727 ± 626 | 0.001 |
| Maternal age (years) | 31 ± 6 | 34 ± 5 | 33 ± 6 | 22 ± 6 | 31 ± 7 | 0.001 |
| Apgar score (1 min) | 6 ± 2 | 6 ± 2 | 6 ± 2 | 6 ± 2 | 6 ± 2 | 0.49 |
| Apgar score (5 min) | 8 ± 1 | 8 ± 1 | 8 ± 1 | 8 ± 1 | 8 ± 2 | 0.14 |
| Male | 50 (16%) | 34 (10%) | 53 (16%) | 28 (8.7%) | 165 (51%) | |
| Female | 45 (14%) | 36 (11%) | 48 (15%) | 29 (9.3%) | 158 (49%) | 0.93* |
| Term infant | 6 (1.9%) | 11(3.4%) | 11(3.4%) | 30 (9.3%) | 58 (18%) | |
| Premature infant | 89 (27.6%) | 59 (18.3%) | 90 (27.9%) | 27 (8.4%) | 265 (82%) | 0.001* |
DM, diabetes mellitus; ANOVA, analysis of variance; SD, standard deviation.
*χ2.
Table 3 Neonatal morbidity in offspring of mothers with diabetes mellitus and controls
| Variable | Type 1 DM (n = 95) (29.4%) | Type 2 DM (n = 70) (21.7%) | Gestational DM (n = 101) (31.3%) | Control group (n = 57) (17.6%) | Total (n = 323) (100%) | p-values |
|---|---|---|---|---|---|---|
| Eutrophic term infant | 7 (2.2%) | 8 (2.5%) | 6 (1.9%) | 14 (4.3%) | 35 (10.9%) | 0.002 |
| Hypotrophic term infant | 1 (0.3%) | 3 (0.9%) | 3 (0.9%) | 16 (5.0%) | 23 (7.1%) | 0.001 |
| Hipertrophic premature infant | 2 (0.6%) | 2 (0.6%) | 1 (0.3%) | 1 (0.3%) | 6 (1.8%) | 0.84 |
| Eutrophic premature infant | 63 (19.6%) | 49 (15.2%) | 74 (23%) | 23 (7.1) | 209 (64.9%) | 0.001 |
| Hypotrophic premature infant | 22 (6.8%) | 8 (2.5%) | 17 (5.3%) | 3 (0.9%) | 50 (15.5%) | 0.02 |
| Pulmonary surfactant use | 25 (7.9%) | 21 (6.7%) | 44 (14%) | 1 (0.3%) | 91 (28.9%) | 0.001 |
| Neonatal hypoglycemia | 7 (2.2%) | 8 (2.5%) | 4 (1.4%) | 2 (0.6%) | 21 (6.5%) | 0.18 |
| Neonatal hypocalcemia | 2 (0.6%) | 6 (1.9%) | 0 (0%) | 0 (0%) | 8 (2.5%) | 0.002 |
| Neonatal hyperbilirubinemia | 51 (15.8%) | 32 (9.9%) | 52 (16.1%) | 5 (1.5%) | 140 (43.3%) | 0.001 |
| Intraventricular hemorrhage | 12 (3.7%) | 11 (3.4%) | 7 (2.2%) | 1 (0.3%) | 31 (9.6%) | 0.03 |
| Bronchopulmonary dysplasia | 14 (4.3%) | 10 (3.1%) | 16 (5%) | 0 (0%) | 40 (12.4%) | 0.02 |
DM, diabetes mellitus.
p= χ2.
Neonatal morbidity
Regarding neonatal morbidity, 26% of children received pulmonary maturation regimens with prenatal steroids. Pulmonary surfactant was used in 28.9% of infants, significantly more frequent in offspring of mothers with DM (p < 0.001). Hypoglycemia and hypocalcemia during the neonatal period were present in 6.5% and 2.5%, respectively. The main neonatal morbidities presented as follows: hyperbilirubinemia (43.3%), intraventricular hemorrhage (9.6%), and bronchopulmonary dysplasia (12.4%), which were significantly more frequent in infants from DM mothers (Table 3).
BMI and nutrition status in children
We found an adequate BMI in 58%, overweight in 6.5%, and obesity in 3.2% in children at 2 years of age (Figure 1). O/O was present in children of mothers with type 1 DM in 8.7%, type 2 DM in 13.6%, GDM in 8.2%, and CG in 6%, with no significant differences between groups.

Figure 1 Nutritional status of children at 2 and 4 years of age according to the percentage of distribution of body mass index (BMI) in offspring of mothers with diabetes mellitus (DM) and controls.
At 4 years of age, O/O was observed in offspring of mothers with type 1 DM in 15.1%, type 2 DM in 15.2%, GDM in 5.2%, and CG in 6%, with no significant differences among groups (Figure 1).
We found an adequate BMI of 47.6% at 6 years of age. We observed an increase in the frequency of overweight (10.6%) and obesity (11%): O/O was present in children of mothers with type 1 DM in 31.1%; type 2 DM in 14.8%; GDM in 16.7%; and the CG in 17.2%, with no significant differences (Figure 2).
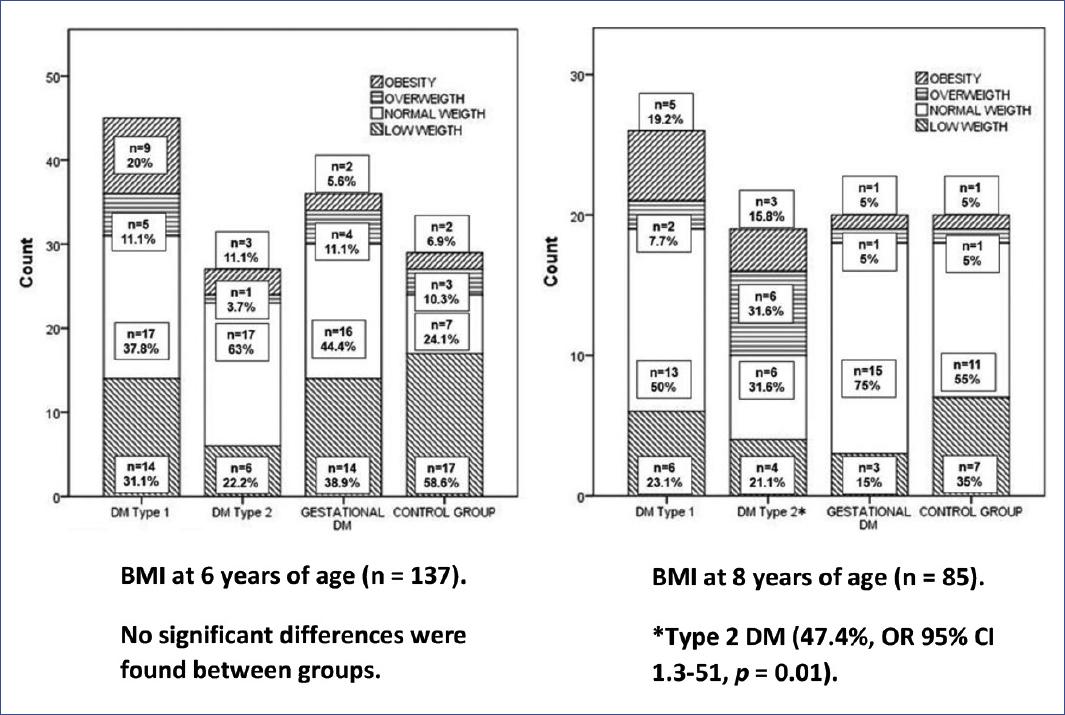
Figure 2 Nutritional status of children at 6 and 8 years of age according to the percentage of distribution of body mass index (BMI) in offspring of mothers with diabetes mellitus (DM) and controls.
At 8 years of age, O/O occurred in children of mothers with type 1 DM in 26.9% (p = 0.21); type 2 DM in 47.4% (p = 0.01); GDM in 10% (p = 0.77); while in the CG, O/O was observed in 10% of the children. These findings mean that 2.5 of each ten infants from mothers with type 1 DM had O/O. One of every two children of mothers with type 2 DM had O/O (47.4%, OR 8.25; 95% CI 1.3-51, p = 0.01) (overweight 31.6%, obesity 15.8%). One of 10 children of mothers with GDM and from the CG had O/O.
Administration of prenatal steroids for lung maturation was not associated with overweight or obesity. Children with low BMI (percentile < 10th) were always present in all groups with a frequency of 31.5% (Figures 1 and 2).
Discussion
Main findings
We found that one of two children from mothers with type 2 DM could have a higher frequency of O/O at 8 years of age. Prenatal steroids administration for lung maturation was not associated with O/O. We also found a high frequency of preeclampsia in mothers with DM, mainly in mothers with type 2 DM, with high mortality in mothers with type 1 DM.
Clinical relevance
Our data show that children from mothers with DM during pregnancy have a lamentably and impressive high frequency of O/O. This result must alert physicians to perform a closer follow-up of these children in managing food intake and exercise promotion to reach a better quality of life. Prenatal steroids for lung maturation could be administrated safely with no risk for O/O in children. Furthermore, obstetricians must pay attention to mothers with DM because they could develop a high frequency of preeclampsia.
Maternal morbidity and mortality
Worldwide, the prevalence of PDM and GDM is increasing due to higher rates of O/O in women and an older maternal reproductive age1,2. Glycemic control, diet, exercise, and early prenatal care in pregnant women with DM in our institution was carried out by a multidisciplinary team with gynecologists, obstetricians, maternal-fetal medicine specialists, endocrinologists, nutritionists, social workers, psychologists, and other specialists, suggesting that even more control is needed because alterations still occur with significant frequency.
The frequency of preeclampsia in mothers with DM was high (28%)with a higher risk in mothers with type 2 DM, which is considered one of the leading causes of preterm birth, maternal-fetal morbidity, and mortality14,15. For example, Yu et al. found that preeclampsia has a higher incidence in women with type 1 DM than the non-diabetic population (20% vs. 5%)16. The mechanisms that contribute to this effect are not well established. High glucose levels during pregnancy with DM can trigger intracellular changes that cause cytotrophoblast dysfunction, predisposing to abnormal placental vascular development and preeclampsia.
Five percent of mothers with DM died during follow-up, with higher mortality of mothers with type 1 DM, possibly due to the chronic condition and complications; however, mothers with type 2 DM and GDM also presented significant mortality, suggesting the need for a close and effective prenatal control.
Infantile morbidity and mortality
During the neonatal period in offspring, morbidities were mainly hyperbilirubinemia, intra-ventricular hemorrhage, and bronchopulmonar dysplasia, which correspond to alterations associated with premature birth, and prevailed significantly in the groups of mothers with DM. Some authors suggest that optimal perinatal control could minimize these morbidities, although it will be difficult to abolish them completely6.
Children's BMI
An adequate BMI (59 %) predominated in all the studied groups and periods. Unhealthy weight (overweight, obesity, and low-weight) was present in each group and all periods, with a clear tendency of O/O increase with age and an inverse trend for low-weight.
Overweight predominated in children of 2 and 4 years and increased in children of 6 and 8 years. This finding suggests that early overweight precedes obesity at school age. Thus, the proportion of overweight in pre-school children deserves attention because it is an early high-risk indicator of the influence of O/O at 4 years of age, which progresses to a higher proportion of children with obesity at school age, with a high proportion in the offspring of mothers with types 1 and 2 DM. This fact is important from a prevention point of view since it represents a window of opportunity to modify the natural history of the appearance of O/O and an excellent time to implement primary prevention programs.
Deierlein et al. found that fetal exposure to maternal glucose concentrations in the high normal range was associated with the development of O/O in offspring at 3 years of age, regardless of pre-gestational BMI7. This result is consistent with our data because predictive indicators of O/O in children are potentially preventable. Therefore, early identification is crucial because it progresses with age and is characterized by an imbalance between intake and energy expenditure.
Studies that evaluated unhealthy weight in offspring of mothers with DM have reported inconsistent associations. The Northwestern University Diabetes in Pregnancy Study reported that weight in offspring of mothers with GDM increased after 5 years of age and that 50% of the children had a weight > 90 percentile at 8 years of age17. We found similar results, although in the offspring of mothers with type 2 DM (one of two with O/O). This finding is consistent with a new report in children of 2-5 years of age, where O/O was observed in two of ten of them (17% and 5.8%, respectively)18. However, the frequency of O/O in offspring of mothers with DM is higher. Obesity is also observed worldwide, and this trend likely results from changes in nutritional behaviors and physical activity patterns. Evidence links dietary and lifestyle factors, which invade domestic and school environments with the risk of O/O19.
In the present study, the children of mothers with GDM in all the analyzed periods showed O/O with no significant differences compared to the CG. At 8 years of age, only one of 10 children from a mother with GDM showed O/O. Both GDM and CG stand out for the tendency to progressively increase O/O during the studied period. However, other studies conducted in China found that maternal GDM increased cardio-metabolic risk in early childhood at 8 years of age but not at 15 years of age20. Another study suggested that the O/O in offspring is explained mainly by maternal pre-pregnancy BMI21. As these data contrast with our results, more research is needed to clarify this controversy.
Offspring of mothers with GDM showed the same percentage of O/O as children of the CG. This finding suggests that the consequences of long-standing changes induced by DM are more adverse in these children. Thus, fewer complications were present in infants from the newly acquired DM in pregnancy. However, more studies are needed to confirm the effect of GDM on childhood O/O. By the experience of the study, we suggest that the problem of childhood O/O might be related not only to pathological or genetic maternal history but also with environmental factors such as demographic and family factors, eating and exercise habits, socioeconomic condition, maternal BMI, maternal education, and nutrition education2,5.
The increased frequency of O/O in offspring of mothers with type 2 DM at 8 years of age is noticeable compared with the other groups4. A possible explanation may be that these mothers had a higher genetic predisposition, worse nutritional habits, and fewer sports activities that influenced their children's development.
By the time they reach childbearing age, young women with DM or carbohydrate intolerance may perpetuate a vicious intergenerational cycle22. In terms of postnatal interventions, breastfeeding seems to have a protective effect against DM. The beneficial effects appear to be through bioactive nutrients found only in breast milk: higher protein content and a slower postnatal growth pattern than formula-fed infants23. In a retrospective study, Crume et al. analyzed the impact of breastfeeding in infant adiposity after PDM and GDM. They reported that breastfeeding for 6 months or more compared to < 6 months was associated with significantly lower BMI, waist circumference, and visceral and subcutaneous adipose tissue at 6-13 years of age24.
Conversely, the percentage of offspring of mothers with DM with low weight was 31%. The frequency of low-weight infants was constantly maintained in all groups and at all ages6,17. In Mexico, low-weight in infants is a long-standing food-nutritional problem that has not been solved yet and may be present in this studied sample.
Proposed hypothesis
Our results suggest fetal metabolic programming in offspring of mothers with DM that reorganizes fetus for hyperglycemia. After birth, children developed particular hunger for sugars and fats. Around 8 years of age, when children are more active in food search, they developed O/O. However, it would be hard to test this hypothesis without considering the transmission of learned lifestyles. This idea is in partial agreement with other authors25 and deserves more research in future studies.
Limitations and strengths
Sample losses through time due to desertion were 18.2% at 8 years of follow-up. Confusing variables such as pre-gestational maternal obesity, poor nutrition habits, sedentary lifestyle, socioeconomic and educational level, and short breastfeeding must be controlled. Pre-, peri-, and postnatal interventions must be considered in reducing the risk of type 2 DM, obesity, and cardiovascular disease in offspring. As polymorphisms associated with overweight/obesity were not searched, they cannot be ruled out. Despite these facts, our results are significant and reflect an increasing public health concern.
Mothers with DM during pregnancy were found at high risk for preeclampsia development. DM during pregnancy also represents a long-term high-risk for O/O in offspring at 8 years of age. Our data cautiously suggests fetal metabolic programming for hyperglycemia in children with mothers with PDM.











 nueva página del texto (beta)
nueva página del texto (beta)


