Introduction
The mean incidence of congenital heart disease ranges from 3 to 8/1000 live newborns, representing about 10% of all congenital malformations1. In general, this pathology is managed surgically. It can be done through definitive correction (which occurs in most cases) or palliative surgery in patients with biventricular pathology that require correction by stages or those who present heart disease where only one of the ventricles is functional (univentricular heart physiology)2.
There are several examples of this type of heart disease, including complex congenital cardiopathies that behave as a single functional ventricle (hypoplastic right ventricle and tricuspid atresia), heart disease with marked ventricular imbalance associated with baseline defect (double outlet right ventricle or unbalanced atrioventricular [AV] canal defects), and heart disease with multiple ventricular communications (“Swiss cheese” type)2. This type of heart disease with single ventricle physiology is clinically associated with cyanosis, signs of low output, or heart failure. Therefore, the definitive treatment is surgical through univentricular correction3.
At present, the worldwide consensus on developing palliation or univentricular correction should be performed in three stages. In a patient under 6 months of age, the pulmonary and systemic flow must be regulated; the overload and cyanosis might continue, although at a tolerable degree that allows adequate development. In those patients between 6 months and 2 years of age, bidirectional Glenn surgery is indicated, which is routinely used as a previous step to Fontan procedure, the third and final stage of univentricular correction4,5.
Glenn surgery is used as palliative surgery and consists of the anastomosis of the superior vena cava to the right pulmonary artery in an end-to-side manner6. Therefore, venous blood passage from the upper half of the body through the right ventricle is avoided. In this way, the single ventricle functions as an aspirating and expelling pump. In the aspirating phase, it passively performs the pulmonary circulation, while in the expelling phase, it is exclusively dedicated to the systemic circulation3,7. However, for this hemodynamic system to work, there must be low pulmonary resistance and low systemic ventricular end-diastolic pressure. Any condition that provokes an increase in these two variables will cause the system’s dysfunction with increased central venous pressure and the appearance of peripheral edema3,8,9.
Choussat criteria were initially formulated to perform univentricular correction under ideal conditions to obtain good results after surgery. These criteria include patients > 3 years old with pulmonary resistances < 2 Wood units, pulmonary artery pressure < 15 mmHg, ejection fraction > 45%, left ventricular end-diastole pressure < 10 mmHg, minimum mitral insufficiency, and adequate diameter of the pulmonary branches (McGoon index > 1.8; i.e., the relationship between the pulmonary branches and the descending aorta). These criteria facilitate the selection of patients and improve their survival10-12.
Some case series studies have reported the characteristics and evolution of patients undergoing Glenn surgical correction13-16.
A case series on 100 patients, ranging from 24 days to 15 years of age, where single ventricle was the most frequent heart disease were studied over 10 years. Eighty-three percent of the patients underwent heart surgery before the Glenn procedure; 15% were reported to show unsatisfactory results, including seven patients who underwent surgical reintervention, and eight died during evolution13.
In another analysis, 333 patients from 42 days to 16 years of age were followed over 12 years. The most frequent diagnosis was hypoplastic left ventricular syndrome and pulmonary atresia with an intact ventricular septum. In this study, 42 patients had an adverse outcome: 22 died later due to respiratory infections, with a 1-year survival rate of 89.8%14.
In a series of 270 patients between 76 days and 11 years of age, over 6 years, it was reported that 132 patients (49%) had single left ventricle morphology and 120 patients (44%) had single right ventricle morphology. In total, 72 patients presented complications: the most frequent were heart rhythm alterations, pleural effusion or chylothorax, respiratory complications, and surgical reintervention. The reported mortality was 0.7% (n = 2) at 1 month after surgery15.
In 2013, a series of 101 patients from 2 months to 9 years of age covering 5 years was reported. In this study, the most frequent diagnoses were tricuspid atresia (n = 24), single ventricle (n = 14), and heterotaxy (n = 13). Up to 74% of the patients had previous surgeries. In 35% of the cases, post-surgical complications were present, with a mortality of 3.9%16.
The current study aimed to describe the 35-year experience of a tertiary hospital regarding cardiac patients with univentricular physiology who underwent Glenn surgery.
Methods
A retrospective analysis of all patients undergoing Glenn surgery from 1980 to 2015 was performed at the Hospital Infantil de México Federico Gómez. All records in the clinical archive of patients who underwent the Glenn procedure were identified. The variables related to the patient, procedure, and post-operative period were recorded. The variables were divided into pre-surgical, intra-operative, and post-surgical. The pre-surgical variables were those related to the patient, such as age, gender, type of heart disease, previous palliative surgery, complications in the last palliative surgery, alterations in the pulmonary artery (stenosis, distortion in the central pulmonary artery, or marked hypoplasia of the pulmonary branches) documented by catheterization or by findings during surgery. Variables related to Choussat criteria were also considered. Among the intra-operative variables, the type of cavopulmonary shunt, the presence of antegrade flow, development of some technical complication during the procedure, time of extracorporeal circulation, and aortic clamping were considered. In addition, post-surgical variables considered were days of intubation, days of amine use, days of intensive care unit stay, and days of hospital stay, developing complications, and death.
Surgical mortality was defined as death occurring within the first 30 days after surgery. Late mortality was considered when the death occurred after the 30-day post-operative period and during follow-up. The follow-up period was from the time of surgery to the present-day or until patients underwent the third phase of univentricular correction (Fontan surgery or total cavopulmonary bypass), with a median follow-up of 13 years (0-32).
Results
From 1980 to 2015, 204 patients with congenital heart disease were scheduled for cavopulmonary anastomosis or Glenn surgery at the Hospital Infantil de México Federico Gómez. The variables studied showed a reasonably homogeneous behavior during data collection. Therefore, files with incomplete information were excluded from the study. A total of 104 patients were included, of which 54.8% (n = 57) were males. The median age was 48 months (5-180 months).
The most frequent diagnoses were tricuspid atresia IB in 19.2% (n = 20), AV discordance in 13.5% (n = 14), visceral heterotaxy (asplenia variety) in 11.5% (n = 12), tricuspid atresia IC in 7. 7% (n = 8), hypoplastic right heart syndrome in 7.7% (n = 8), double outlet right ventricle in 6.7% (n = 7), double inlet left ventricle in 5.8% (n = 6), pulmonary atresia in 4.8% (n = 5), and other heart disease in 15.3% (n = 16). Approximately half of the patients previously underwent palliative surgery: right modified Blalock Taussig systemic pulmonary fistula in 30 (28.8%), pulmonary artery cerclage in 20 (18.3%), atrioseptostomy in three patients (2.9%), central fistula in two patients (1.97%), and pulmonary artery branch angioplasty in one patient (0.96%).
The most common pathologies, the palliative surgeries performed, and the pre-surgical variables are summarized in table 1. The intra-operative variables (related to surgery) are shown in table 2. The post-surgical evolution (results and most frequent complications) are shown in table 3.
Table 1 Pre-surgical characteristics of 104 cardiac patients with univentricular heart physiology
| Median (minimum-maximum) | |
|---|---|
| Age (months) | 48 (5-180) |
| Males* | 57 (54.8) |
| Previous palliative surgery* | 56 (53.8) |
| Ejection fraction (%) | 68 (35-93) |
| Pulse oximetry saturation (%) | 71 (46-88) |
| Pulmonary vascular resistance (WU) | 2.3 (0.11-7.17) |
| Pulmonary arterial pressure (mmHg) | 11 (2-21) |
| End-diastolic pressure of the left ventricle (mmHg) | 5 (2-12) |
| Left atrial pressure (mmHg) | 4 (0-12) |
| Nakata index | 297 (130-644) |
| McGoon index | 2 (1.50-3.20) |
| Pulmonary branch hypoplasia* | 15 (14.4%) |
| AV valve insufficiency* | |
| Mild | 18 (17.44%) |
| Moderate | 2 (2.32%) |
| No insufficiency | 83 (80.23%) |
| Functional class* | |
| I | 14 (13.5%) |
| II | 62 (59.25%) |
| III | 28 (27.16 %) |
*n (%). AV: atrioventricular.
Table 2 Intra-operative characteristics of 104 cardiac patients with univentricular heart physiology
| Percentage (%) | |
|---|---|
| With antegrade flow | 51.9 |
| Unilateral Glenn | 87.5 |
| Extracorporeal circulation support | 89.69 |
| Aortic clamping | 26 |
| Circulatory arrest | 10.38 |
| Extracorporeal circulation time (min) | 90 (45-420)* |
| Aortic clamping time (min) | 15 (5-105)* |
| Circulatory arrest time (min) | 40 (5-60)* |
*Median (minimum-maximum).
Table 3 Post-surgical characteristics of 104 cardiac patients with univentricular heart physiology
| Median (minimum-maximum) | |
|---|---|
| Intubation (days) | 1 (0.33-15) |
| Management with amines (days) | 2 (1-15) |
| Antibiotics (days) | 3.5 (2-24) |
| Intensive care unit stay (days) | 4 (1-21) |
| Hospital stay (days) | 9 (2-120) |
| Oxygen saturation after Glenn surgery (%) | 86 (65-98) |
| Complications* | |
| Infectious | 16 (15.4) |
| Bleeding | 10 (9.6) |
| Arrhythmias | 9 (8.7) |
| Chylothorax | 7 (6.7) |
| Neurological | 7 (6.7) |
| Pleural effusion | 4 (3.8) |
| Other | 6 |
| Mortality* | 3 (2.9) |
*n (%).
The analysis of pre-surgical variables and morbidity showed the following relationship: 11 patients < 1-year-old were reported, and age was not evidenced as a risk factor in mortality; however, it was found to be related to morbidity, since the days of intubation, days of intensive care unit stay, and days of hospital stay increased compared to the reported mean in patients over 1-year-old (30 vs. 9 days).
Of the total number of patients <1-year-old, 82% presented some complications. The most frequent were arrhythmias, AV blocks, infections, chylothorax, and neurological complications, while in patients > 1-year-old, complications occurred in only 30%.
An ejection fraction lower than 60% was related to a higher incidence of pleural effusion and chylothorax by 40%. Severe AV valve failure was associated with a more extended hospital stay than no AV valve failure (30 vs. 9 days). One of the deaths was related to severe AV valve failure.
Moreover, the presence of severe hypoplasia of the pulmonary branches was related to increased extracorporeal circulation time (150 min vs. 90 min), as well as to the presence of bleeding and death (two of the three deceased patients presented severe hypoplasia of the pulmonary branches).
Among the most frequently reported complications were infections (15.4%), such as sepsis, ventilator-associated pneumonia, catheter-related sepsis, or urinary tract infection, which were successfully managed with antibiotic treatment. Only two patients presented acute renal failure, and only one of them required Tenckhoff catheter placement for 2 days.
Another major complication was bleeding (9.6%), which was reported during surgery: technical complications due to intricate anatomy, hypoplasia of the pulmonary branches, or firm adhesions. Of the patients who presented bleeding, 15% had severe hypoplasia of the pulmonary branches, which meant a longer pump-time and serious technical surgical difficulty.
Concerning the degree of complexity during surgery, 25% of patients presented technical complications, one or more occurring in the same patient. The most common were intricate anatomies (16.3%), such as persistence of left vena cava, which implied the performance of bilateral Glenn correction, double discordances, or dextrocardia; hypoplasia of pulmonary branches (14.4%), which required some enlargement technique, and firm adhesions (0.96%). Extracorporeal circulation time was longer in this last group of patients than the group of patients with no technical complications during surgery (150 vs. 90 min). The complications associated were increased risk of bleeding and death.
Arrhythmias occurred in 8.7% of all patients undergoing Glenn surgery, which were resolved with medical management. The presence of arrhythmias was associated with neurological complications, such as hypoxic-ischemic events, hemiparesis, and seizures. Of the patients who presented neurological complications, 60% presented some type of cardiac arrhythmia.
No risk factor was found to be associated with chylothorax; however, its presence resulted in an increased risk of sepsis and, therefore, increased days of antibiotic treatment.
Pleural effusion was related to the ejection fraction and lung pressure before surgery.
Notably, Glenn’s surgery with antegrade flow was related to the possibility of performing the surgery without extracorporeal circulation support. That is, patients who underwent Glenn without antegrade flow showed a greater necessity to be supported by an extracorporeal circulation machine during surgery (odds ratio [OR] = 10.3; 95% confidence interval [CI] 1.25-85.2). Similarly, patients with antegrade flow achieved better post-surgical oximetry saturation and shorter intubation time, while patients without antegrade flow showed lower saturation and more intubation days (OR = 6.1; 95% CI 1.5-23.4). These results should be the target of future research, in addition to the fact that antegrade flow has been described as decreasing the likelihood of developing pulmonary arteriovenous fistulas11,12,15.
Regarding mortality, only three patients out of 104 cases died. For that reason, we will describe each of the cases because we considered it unnecessary to perform multivariate analysis.
The reported mortality was 2.9% (3/104). Causes of death were bleeding, pulmonary hypertension, and ventricular dysfunction. The first case was a 5-year-old male patient diagnosed with visceral heterotaxy (polysplenia variety), with hypoplasia of pulmonary branches. Surgery was performed with extracorporeal circulation support, during which the patient presented bleeding and died in the operating room. The second case was a 9-month-old male diagnosed with an unbalanced AV canal and severe AV valve insufficiency. This patient underwent Glenn and AV valve repair. However, 2 days after surgery, the patient required reintervention to perform pulmonary artery cerclage due to significant dilation of the artery. The patient presented infectious complications treated with antibiotics appropriately and died after 33 days of in-hospital stay. Pulmonary arterial hypertension was considered the cause of death. The third case was a 7-year-old male diagnosed with tricuspid atresia IC with coarctation of the aorta and pulmonary artery confluence stenosis, who initially underwent coarctectomy and pulmonary artery cerclage. Later, branch and central fistula repair with a 6 mm tube were performed. A year later, a classic bilateral Glenn was performed due to a rupture of the pulmonary artery’s trunk; the patient presented acute renal failure as a complication in the post-surgical period, which required management with acute peritoneal dialysis; he also presented extrasystoles. The patient left the hospital 17 days after the surgery. He later presented systolic dysfunction with an ejection fraction (EF) of 22%, pulmonary artery pressure of 24 mmHg, and end-diastole pressure of 10 mmHg, so he was considered a non-candidate for Fontan surgery; an axillary fistula was performed, and he was listed as a candidate for a heart transplant. The patient died while waiting for a heart transplant donor, and ventricular dysfunction was considered the cause of death.
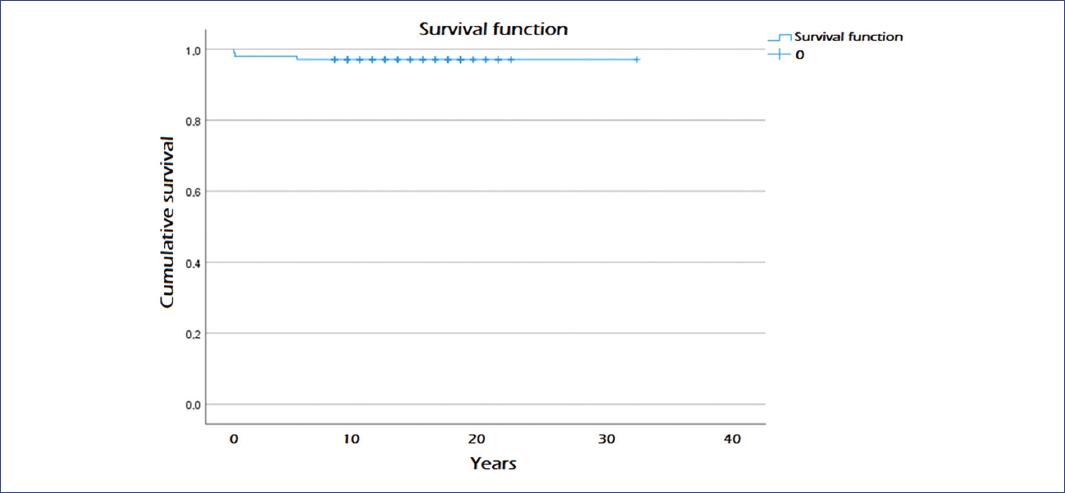
The total number of patients who underwent surgery was monitored from the intervention day to the present time or until they underwent Fontan surgery or total cardiopulmonary bypass. Of all the patients who have undergone Glenn surgery, 80.74% are awaiting Fontan surgery, maintaining a good state of health but with the deterioration of their functional class directly proportional to the time passed since Glenn surgery. Moreover, 9.6% of patients have successfully undergone total cavopulmonary anastomosis (Fontan procedure); 2.9% of patients have unsuccessfully attempted Fontan and died during the procedure; 4.8% were excluded from treatment with Fontan because they did not meet surgical criteria; 1% died without Fontan; and 0.96% died in the late post-operative period of Fontan procedure17. The 10-year survival rate was 97.1% (Fig. 1).
Discussion
Palliation for the treatment of congenital heart disease is intended to relieve signs, symptoms, or pathophysiological situations that increase the probability of death or the development of other irreversible or challenging alterations (pulmonary hypertension, cyanosis, or heart failure). In general, the implementation of these palliative procedures is provisional, while a definitive correction is performed. In some cases, these procedures can be definitive due to the complex nature of congenital heart disease2,3. In international literature, mortality results for this pathology have been reported from 0.7 to 10.2%: Kogon et al. in Atlanta (0.7%), Becerra et al. in Argentina (3.9%), Fernández et al. in Spain (8%), and Tanoue in Japan (10.2%)13-16.
In the present series, the pre-surgical diagnoses were very similar compared to other reports, as well as the main post-surgical complications, among which we mainly found the pleural effusion, chylothorax, and infections.
Enormous controversy exists concerning the age at the time of surgery; the current recommendation is to perform surgery on children over 6 months of age to decrease the occurrence of late arteriovenous malformations11. In our series, only 11 patients < 1 year of age were related to a more significant number of complications.
The pre-surgical variables related to morbimortality were ejection fraction, AV valve insufficiency, and hypoplasia of the pulmonary branches, but not pulmonary artery pressure, end-diastolic pressure, and left atrial pressure, which are the criteria currently used to perform Glenn surgery. Although 42 patients (40.3%) presented some of these high-risk criteria, no relationship with mortality was found. In this sense, we should consider the significant progress in critically ill pediatric patients’ management, which becomes a topic of interest to be considered in future research14-16,18-25.
Of the total number of patients who have undergone Glenn surgery, approximately 80% are waiting for Fontan surgery in good conditions. About 10% have successfully undergone this procedure, and 4.8% are ineligible for this surgery due to pulmonary hypertension diagnosed by cardiac catheterization. However, we could consider the oxygen consumption measured by a graded stress test in these patients as a diagnostic complement. This test provides objective information about the hemodynamic state of the patient at rest and during exercise. Interestingly, this field has not been widely explored in the pediatric population.
Another reason that makes patients not candidates for Fontan procedure after Glenn surgery is arteriovenous fistulas. It has been observed that performing Glenn surgery with antegrade flow decreases this condition; however, further studies are necessary to prove this result.
During Fontan surgery, 2.9% of patients died because of adhesions from previous surgeries. It is necessary to study other reasons why patients are not candidates for Fontan surgery to avoid them, since this procedure and Glenn’s surgery effectively improve the quality of life of patients with univentricular heart pathologies17.
Glenn surgery or cavopulmonary bypass is a palliative surgery used in univentricular congenital heart disease with excellent results. It significantly improves cyanosis, signs of low cardiac output, and decreases the presence of heart failure for a long time before the performance of total cavopulmonary bypass (Fontan procedure). This procedure has been observed to present a few complications and very low mortality (only 2.9%). Although this surgery presents some complications, we consider Glenn surgery to be safe and should be used for the treatment of this type of congenital heart disease.











 nueva página del texto (beta)
nueva página del texto (beta)