Introduction
During the first 2 years of life, the foundations for the optimal growth and development of every human being are laid. Adequate nutrition at this age is essential since it is when more physical, metabolic, and mental changes are developed in less time1. During this period, a higher risk of nutritional deficiencies and deficit or excess of energy consumption will impact on metabolic programming1,2. Poor nutrition at this stage will condition health in later stages of life, being a risk factor for chronic diseases in adulthood, such as obesity, type 2 diabetes mellitus, hypertension, allergies, among others3, in addition to diminishing intellectual performance, concentration and execution in work activities, as well as reproductive health2.
For the proper nutrition and development of children, the United Nations Children’s Fund, the World Health Organization (WHO), and other national and international organizations4-6 recommend exclusive breastfeeding (EBF) until the age of 6 months and complementary feeding (CF) together with breast milk (BM) from this age onward as the most cost-effective preventive intervention on the life of a child4.
CF is defined as the process of introducing foods other than BM when this is no longer sufficient to satisfy the nutritional needs of the infant1,7,8. However, some discrepancies exist in the recommendations of CF, such as the age of initiation, sequence of introduction, consumption of allergens, sugary drinks, and portions7,9-14.
Aiming to create unified criteria, and to adapt it to the Mexican context, a consensus of experts created the Guidelines for CF Practices in Healthy Infants (GCFHI) in 2016, as a reliable source of information for Mexican pediatricians7. According to the consensus, the CF should start at 6 months of age, offering at the beginning food sources of iron and zinc, such as meats and fortified cereals, with the introduction of solids, individually, cooked, without salt, sweeteners, or flavorings7.
This study aimed to understand the current practices of mothers and pediatricians regarding breastfeeding (BF) and CF, as well as their differences and similarities with the current national recommendations.
Methods
Across-sectional study that consisted of two surveys was conducted. The first survey was designed for mothers and the second one for pediatricians living in Mexico. The purpose of the survey was to acknowledge the current practices of mothers and pediatricians regarding BF and CF, as well as their differences and similarities with the current international recommendations.
Thirteen of the 16 points listed in the GCFHI were considered, excluding development milestones, baby-led weaning practice, veganism, and vegetarianism, which are implicit in other questions. Each point was written as a question, maintaining a medical language for pediatricians and a plain language for mothers. The surveys were sent to pediatricians, who were members of the Mexican Association of Pediatrics and the National Confederation of Pediatrics of Mexico, throughout the country by e-mail, who, in turn, sent the version of the survey for mothers of healthy children. The survey was applied anonymously, at convenience and with a snow-ball methodology15. Data of the surveys were collected between April and September of 2018. Mothers of healthy infants between 6 and 24 months of age and Spanish-speaking pediatricians residing in Mexico treating healthy infants were included in the study. A total of 104 pediatricians participated (100% were included) and 377 mothers were included in the study (96 mothers were excluded because their child’s age did not meet the inclusion criteria).
Surveys were conducted for pediatricians and mothers. The exclusive BF variable for mothers was constructed with the following questions: Are you currently BF your baby? How long did you or do you plan to breastfeed your baby? Do you supplement or supplemented BM with formula? If yes, at what age?
Infants who were fed exclusively with BM for at least 6 months were included in this variable. Mothers who supplemented feeding with substitutes from birth or before 6 months were excluded from the variable.
For pediatricians, this variable was built with the following questions: Do you recommend EBF in healthy babies? If yes, up to what age? Do you recommend supplementing a healthy baby with milk formula? If yes, beginning at what age? At what age do you recommend beginning with CF?
As for CF, the variable of fortified cereals in the question “Which food did you start CF with?” was only included in the survey for pediatricians to avoid an error of measurement, assuming that some mothers would not know the difference between fortified and unfortified cereals. Concerning allowed and not allowed foods, the variable “sweeteners” was questioned only to pediatricians, assuming that some mothers would not know which foods contain sweeteners.
Statistical analysis
Data were analyzed with descriptive statistics. Frequencies were calculated for the categorical or dichotomous variables and mean and standard deviation for continuous variables. The recommendations of the pediatricians and the actions of the mothers regarding BF, up to what age, complementation with formula, and the beginning of CF were compared using χ2 and Student’s t-test for the categorical and continuous variables.
Age, sex, and education level groups were used to compare the characteristics of the participating mothers and pediatricians. Age was categorized for both groups (from 15 to 25, from 26 to 35, from 36 to 45, and older than 45 years). Sex was categorized as male or female for pediatricians. Education level was categorized in elementary school, middle school, high school, college, and postgraduate degrees. The age of the pediatricians was used as a covariate categorized as < 45 years and > 45 years. Response frequencies were used for the elaboration of the graphics. Statistical analysis was performed with the statistical package Stata 14 (StataCorp, 2014. Stata Statistical Software: release 13. College Station, TX: StataCorp LP).
Results
Table 1 shows the baseline characteristics of the population included in the study (pediatricians and mothers). In this sample, 52.9% of pediatricians were men. The majority of pediatricians (45.2%) were ≥ 46 years old, followed by the age group of 36-45 years old (27.9%), and finally, the age group of 26-35 years old (26.9%). The group of mothers was younger than the group of pediatricians: 62.8% were between 26 and 35 years old and < 1% were older than 45 years. Besides, 76.7% of the mothers completed college or postgraduate degrees, 18.6% graduated from high school, and < 5% finished only middle school.
Table 1 Baseline characteristics of pediatricians (n = 104) and mothers (n = 377)
| Sex | Pediatricians (%) | Mothers (%) |
|---|---|---|
| Female | 47.1 | 100.0 |
| Age 15‑25 26‑35 36‑45 46+ |
0.0 26.9 27.9 45.2 |
18.8 62.8 17.5 0.9 |
| Schooling Middle school High school College or postgraduate |
0.0 0.0 100.0 |
4.8 18.6 76.7 |
The mean age of infants included in the sample is shown in Table 2.
Table 2 Age of infants considered in the study (n = 377)
| Age in months | Mean (95% CI) | Distribution (%) |
|---|---|---|
| 6‑11 | 7.8 (7.5‑8.1) | 41.9 |
| 12‑17 | 13.9 (13.6‑14.3) | 22.8 |
| 18+ | 18.8 (18.7‑18.9) | 35.3 |
95% CI: 95% confidence interval.
Table 3 shows the recommendation and practice of BF and CF between pediatricians and mothers. The GCFHI recommends EBF until 6 months of age. The results show that 91.3% of pediatricians recommended EBF, compared to 90.7% of mothers who perform it. However, 76% of pediatricians recommended supplementing the feeding with artificial formula before 6 months in some cases, while 34.4% of mothers supplemented the feeding with formula and 22.2% before 6 months of age. The mean onset of CF was 6.1 months (95% confidence interval [CI] 6.0-6.2) in the group of mothers and 5.7 months (95% CI 5.6-5.9) recommended by pediatricians. Finally, the mothers who were BF by the time of the survey (n = 290) had the intention of continuing with BF for more than 6 months, supplemented or not with formula. From a total of 87 mothers who were not BF any more by the time of the survey, 48.2% did it for < 6 months, supplemented or not with formula.
Table 3 Recommendations and practice of breastfeeding and complementary feeding among pediatricians and mothers
| Recommendations | Pediatricians | Mothers | GCFHI | p‑value |
|---|---|---|---|---|
| Recommends (pediatrician)/performs (mother) exclusive breastfeeding until 6 months of age (%) | 91.3 | 76.9 | 100 | 0.001 |
| Recommends (pediatrician) or complements (mother) with formula before 6 months of age (%) | 76.0 | 22.3 | 0 | < 0.001 |
| Complementary feeding onset in months (mean ± SD) | 5.74 ± 0.66 | 6.13 ± 0.92 | 6 | < 0.001 |
GCFHI: guidelines for complementary feeding in healthy infants; SD: standard deviation.p-values for the continuous variable were obtained with Student’s t‑test analysis.
Table 4 shows the recommendations of pediatricians according to age, regarding EBF, complement with BM substitutes, and age of onset of CF. It was observed that 91.3% of pediatricians ≤ 45 years old recommended EBF until 6 months of age, compared to 89.4% of those > 45 years old. In contrast, 84.2% of pediatricians ≤ 45 years old recommended supplementing with BM substitutes before 6 months old, compared with 66% of those > 45 years old (p = 0.030).
Table 4 Recommendations of the pediatricians according to their age regarding EBF
| Recommendations | Pediatricians ≤ 45 years old | Pediatricians > 45 years old | p‑value |
|---|---|---|---|
| Recommends EBF until 6 months of age | 93.0% | 89.4% | 0.513 |
| Recommends complementing with formula before 6 months of age | 84.2% | 66.0% | 0.030 |
| CF onset in months (mean ± SD) | 5.65 ± 0.69 | 5.85 ± 0.62 | 0.126 |
EBF: exclusive breastfeeding; CF: complementary feeding; SD: standard deviation. p-values for dichotomous variables were obtained with Chi‑square test analysis.
p-values for the continuous variables were obtained with Student’s t‑test analysis.
Figure 1 shows the most recommended foods by pediatricians or mothers for the initiation of CF. The results show that vegetables were the most recommended food by pediatricians and administered by mothers (87% and 91%, respectively); secondly, fruits were recommended by 64% of pediatricians, and 70% of mothers started CF with them. In contrast to the recommendations of the GCFHI, only 19% of pediatricians recommended initiating CF with cereals and 21% with iron-fortified cereals. Only 29% of mothers started with cereals, without specifying if they were fortified or not. Only 23% of the pediatricians recommended animal-source protein (meat, chicken, fish, and egg) for the beginning of CF and only 26% of the mothers started CF with this food.
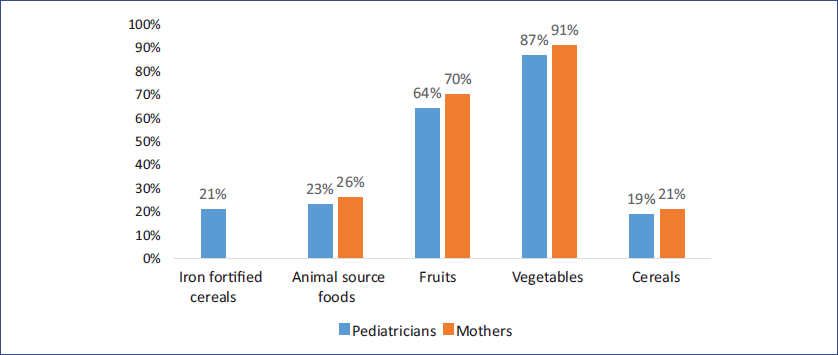
Figure 1 Most recommended foods for the onset of complementary feeding (CF) by pediatricians and mothers. Fortified cereals and animal-source foods are the ones that Guidelines for Complementary Feeding in Healthy Infants recommend for CF onset.
Figure 2 presents the recommendation of pediatricians for the ingestion of foods and beverages that have been indicated by the GCFHI as not suggested before 2 years of age (tea, atole, juices, sweet/added sugar, and sweeteners) and the age at which mothers introduced them to their children. It also presents the results for foods that are recommended from 6 months of age, such as pork, egg, citrus, and how often pediatricians recommend them and mothers use them. Around 60% of pediatricians follow this recommendation and do not recommend the intake of tea, atole, juice, sweets, added sugars, or sweeteners; however, broths were highly recommended. In general, mothers introduced this type of food between 6 months and 1 year of age or later. As for food such as pork, egg, or citrus, both pediatricians and mothers recommended or introduced them after 6 months of age, although about half of them delayed the introduction at 1 year of age or later. Furthermore, 79.8% of pediatricians do not recommend sweeteners, while 18.4% recommend them after 1 year of age (data not shown).
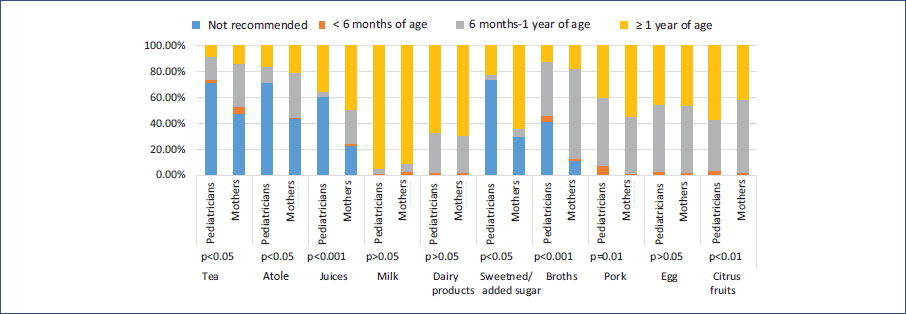
Figure 2 Age recommendation by pediatricians for the ingestion of foods and beverages not recommended by Guidelines for Complementary Feeding in Healthy Infants (GCFHI) before 2 years of age (teas, atole, juices, sweet/added sugar, and sweeteners) and other foods recommended by GCFHI from 6 months of age (pork, egg, and citrus), compared to the age mothers introduce them to infants. p-values were obtained with a χ2 test analysis.
Discussion
Regarding BF and CF, it was necessary to explore the practices of mothers and pediatricians and assess the differences and similarities with the GCFHI recommendations. In general, the interviewed pediatricians do not base their practices on current recommendations. Not all pediatricians recommend EBF and most of them recommend supplementing the feeding with BM substitutes before 6 months of age. For the interviewed mothers, 76.9% practiced EBF for 6 months, and from the mothers who were BF by the time of the survey (n = 290), 100% intended to continue this practice for longer than 6 months, complementing it or not with BM substitutes, accompanying the CF.
Vegetables were the main CF starting food pediatricians recommend and mothers choose (87% and 91%, respectively). The second most recommended food was fruit (64% for pediatricians and 70% for mothers), contrasting with the low percentage of pediatricians who recommended starting with iron-fortified cereals (21%) or animal-source foods (23%) that, according to the GCFHI, are the recommended choice to start CF.
It is estimated that Mexico has one of the lowest EBF rates within Latin America16,17. According to the data from the National Health and Nutrition Survey 201218, the prevalence of EBF in children < 6 months of age was 14.5%. In rural areas, it decreased from 36.9% in 2006 to 18.5% in 201217.
In 2015, Deming et al.19 conducted a study describing the transition of food for children aged 0-4 years and reported that 85% of the caregivers, mostly the mother, had elementary or middle education. In contrast, the present results showed that 76.7% had college or post-graduate degrees. In their sample, the percentage of infants aged 0-3.9 months who received EBF was 15%, which decreased to 4% at 4-5.9 months. The present findings showed that 23.1% received EBF for < 6 months of age. These differences could be explained by the specific characteristics of the sample, such as higher education and being a patient at the private sector, or by external factors, such as health campaigns or awareness.
The EBF is the most effective way to give the infant a complete diet until 6 months of age, for which GCFHI and the WHO recommend it. BM provides all the necessary nutrients for the optimal development of infants; it is safe and contains antibodies and living cells that reduce the risk of some diseases1,3,4,7,13,20. In addition, it decreases the incidence of type 2 diabetes mellitus, acute myocardial infarction, hypertension, and breast and ovarian cancer in mothers21. While GCFHI and the WHO recommend EBF for 6 months, the present results showed that 91.3% of the pediatricians recommend the EBF up to 6 months. However, most pediatricians indicate BM substitutes before 6 months of age, and younger pediatricians (≤ 45 years) tend to make this recommendation more than those > 45 years. Inadequate training in this matter, which is not developed from the college medical education in Mexico, causes that health-care providers promote diet with formula17. Furthermore, possible conflicts of interest with the infant formula industry and earnings associated with its inadequate promotion, unethical publicity, and easy access to BM substitutes in public and private media can lead to the acceptance and recommendation of formulas before 6 months of age17.
Conversely, 78.6% of the mothers reported BF and begining CF, according to the recommendations of their pediatrician, although only 76.9% of them gave EBF for 6 months. Multiple social and cultural factors influence the early abandonment of the EBF, such as the lack of adequate spaces in the workplace, lack of awareness of the benefits of the EBF, binomial separation at birth, the indication by the pediatrician to supplement with formula, and the discrimination of mothers who breast-feed in public17,21,22.
Agreater effort from the health-care system must be made so that pediatricians and health-care providers, in general, are well-trained, updated, and adhere to the recommendations. It has been reported that when health providers are sensitized to the EBF and trained, they offer support to mothers in this process, and the rates of EBF increase by 15%, being the most successful strategy to improve the duration of both EBF and total BF. To achieve higher rates of EBF, the need for training on this subject among health professionals is urgent17,23.
Feeding must be complemented after 6 months of age because BM is no longer sufficient for the nutritional needs of the infant8. Pediatricians recommend starting CF on average at 5.7 months of age, while mothers did so at 6.1 months of age (p < 0.001), which is in line with the GCFHI recommendations. Delaying CF beyond 6 months leads to the risk of growth retardation, malnutrition, anemia, and zinc deficit13. There is no scientific evidence of a benefit regarding the sequence of food introduction. The GCFHI recommends assuring the intake of iron and zinc through CF by the daily consumption of animal-source foods or fortified cereals from 6 months of age3,7. These results showed that only 23% of pediatricians and 26% of mothers started with animal-source products and 21% of pediatricians recommended starting with fortified cereals. Thus, 44% of pediatricians recommended starting CF with food sources of high bioavailability iron, contrasting with the results of Deming et al.19, where only 3-4% of infants aged 6-11.9 months had consumed fortified cereals, and 2-18%, meat. On the contrary, 87% and 91% of pediatricians and mothers initiated CF with vegetables, which could be a strategy to encourage fondness for vegetables from an early age24; however, the iron contained in the vegetables is in a non-heme form, which decreases its bioavailability3,7. Iron deficiency anemia at this age is a frequent problem due to insufficient intake, coupled with high iron requirements. This condition in the infant, who has a faster growth and brain development, can have consequences in the maturation of the nervous system in both its morphological development and its biochemical function, resulting in delayed cognitive functions, alterations in the auditory and visual evoked potentials, among others25. Iron deficiency anemia, micronutrient deficiencies, and malnutrition continue to be health problems in our country, especially at this age. Promoting CF according to the recommendations of the GCFHI ensures the sufficient intake of nutrients and promotes a balanced and healthy diet from infancy, which will help to decrease micronutrient deficits, malnutrition, and childhood obesity7,16.
In Mexico, the prevalence of overweight and obesity in children under 5 years of age is 5.8% for females and 6.5% for males26. In addition, 33.2% of children between 5 and 11 years of age are overweight or obese27, largely due to a poor quality of food and excess of energy consumption, especially through sugary drinks and industrialized foods. Deming et al.19 concluded that 63% of 12-month-old infants consumed sugary drinks, increasing to 78% at 24 months, while 46% of mothers had offered sugary drinks before 1 year of age in the present sample. Before 2 years of age, the intake of sugary drinks, such as soft drinks, juices, and flavored water, or sweeteners, is not recommended since they favor the liking for sweet flavors, building bad eating habits from an early age, and increasing the risk of developing overweight and obesity during childhood, adolescence, and adulthood1,7,13,19,20. GCFHI does not recommend drinks such as atole, tea, broths, and smoothies before 2 years of age since no nutritional benefits have been demonstrated on these products, are highly energetic, and most of them are sweetened7. The results show that over 60% of pediatricians do not recommend these products before 2 years of age, while about half of the mothers introduced them before the first year of age (p < 0.05), with juices being introduced particularly early (p < 0.001). It was also observed that around 80% of pediatricians did not recommend sweeteners at all, but the rest recommended sweeteners after 1 year of age.
Some foods are commonly avoided due to myths or beliefs related to the development of allergies or diseases. However, it has been shown that they are adequate at this age and provide essential nutrients. Among these foods are citrus fruits, which are an essential source of ascorbic acid7, well-cooked pork, and well-cooked eggs, which are sources of protein and iron with excellent bioavailability. The late introduction of egg is related to an increased risk of developing allergies7,13. For this reason, GCFHI recommends introducing these products from 6 months of age. In this study, less than 50% of pediatricians recommended such foods before the first year of age, demonstrating once again the lack of updating of the Mexican pediatricians in this regard, while mothers started with them a little earlier. For example, the introduction of citrus fruits is delayed until 1 year of age or later by 60% of pediatricians, while 60% of mothers started them between 6 months and 1 year of age (p < 0.01).
This study has some limitations. First, the sample size is small, both for pediatricians and mothers, and most of the mothers included had a high level of education, which could influence their BF and CF practices. However, the participants came from different states of the country, so the sample showed regional variability. Second, the questionnaire was self-applied, which may increase the measurement error. In any case, this error would be non-differential between mothers and pediatricians. The fact that the pediatricians sent the surveys to the mothers could have caused a response bias since they could have answered what they thought their pediatrician expected. However, the survey was anonymous, so it may be assumed that the presence of this bias was low. Third, the characteristics of the mothers included in this study may not be representative of all mothers in Mexico, since 76.7% had college or post-graduate degrees, which could influence decision-making regarding the feeding of their children, and even the possibility of going to a private consultation with a pediatrician. Fourth, the presence of confusion in this study cannot be ignored since the socioeconomic status or other sociodemographic variables were not included, which, in the case of mothers, are factors that could influence their BF and CF habits. Fifth, since it was a survey made at convenience and with a snowball methodology, the number of pediatricians and mothers who received the survey as well as the non-response rate was unknown. Sixth, no distinction was made between pediatricians working in the public or private sector, their institution or state, data which may have influenced their recommendations.
The nutrition during the first 2 years of life is essential for promoting adequate growth and development of the infant, metabolic programming, and prevention of chronic diseases in adulthood, which represents the leading cause of death in Mexico. Although no specific rules exist for infant feeding, some recommendations indicate EBF for 6 months and adequate CF after this age. Many of the interviewed pediatricians did not base their practices on current recommendations: they recommended complementing the feeding with BM substitutes before 6 months of age and mostly with the delay of iron source food intake until 7-9 months, reflecting an inadequate training and update in this area.
The practices of the interviewed mothers differed from the pediatrician’s recommendations, particularly on the duration of EBF (about 30% for < 6 months), which is probably influenced by other psychosocial factors. It is imperative to reinforce efforts to maintain EBF for 6 months and continue it together with CF, as well as to promote that from the beginning of the CF, the adequate consumption of macro- and micro-nutrients should be encouraged, since they extend benefits to infants and mothers, and reduces costs of diseases attributed to poor nutrition in the health-care sector.











 nueva página del texto (beta)
nueva página del texto (beta)


