Introduction
The abrupt compromise of the renal function, which leads to fluids, electrolytes, and waste products disturbances, is known as acute kidney injury (AKI) 1. The incidence of AKI is increasing in hospitalized critically ill patients 2. In a multinational study, 26% of patients (4,683) admitted to the intensive care unit developed AKI. Severe cases were associated with an increased mortality 3.
Up to 30% of the newborns admitted to the neonatal intensive care units develop some degree of kidney injury, being an independent risk factor for poor outcome 4. However, the lack of standard definitions makes it difficult to diagnose and analyze the real impact of AKI, although even mild renal impairment conducts to important clinical consequences 5.
In preterm infants, necrotizing enterocolitis (NEC) is a leading cause of mortality 6. The incidence in the United States is 1.1 per 1000 live births, with a mortality of 50% on its more severe forms 7. A significant number of survivors have profound neurodevelopment delay and a high impact on treatment costs and the quality of life 8.
Bell’s staging 9 has traditionally been used to assign the severity of NEC. However, other risk factors such as peritonitis, sepsis, respiratory failure, and AKI have been described to contribute to its high mortality 10.
AKI and NEC are two conditions tightly related, both frequently observed to develop simultaneously in preterm newborns 11. NEC is not limited to the gastrointestinal tract and leads to a systemic inflammatory response predisposing to AKI 12. The relation between these two conditions increases mortality in newborns.
This study aimed to analyze the risk factors to develop AKI in patients diagnosed with NEC and to compare the mortality between infants with and without AKI.
Methods
This study was designed as a retrospective cohort. A chart review of infants admitted to the neonatal intensive care unit was conducted from January 2012 to December 2017, including patients with the diagnosis of NEC regardless of the gestational age. Exclusion criteria comprised insufficient essential data for the diagnosis of AKI and NEC severity staging. This study was approved by the Hospital Ethical Committee. The informed consent was not required.
AKI was defined according to the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guideline for Acute Kidney Injury staging 13. According to these staging criteria, serum creatinine and urine output were considered. AKI is divided into three stages: stage 1 is defined as the increase in serum creatinine ≥ 0.3 mg/dl or the increase of 1.5 to 1.9 times baseline or urine volume < 0.5 ml/kg/h for 6 to 12 hours. Stage 2 is defined as the increase in serum creatinine 2 to 2.9 times baseline or urine output < 0.5 ml/kg/h for more than 12 hours. Lastly, stage 3 is characterized as the increase in serum creatinine 3 times baseline or ≥ 4 mg/dl or urine output < 0.3 ml/kg/h for more than 24 hours or anuria for more than 12 hours.
Baseline creatinine was considered as the lowest serum creatinine level at least 72 h before the diagnose of NEC; it was compared to the highest creatinine level during the development of NEC.
NEC was classified according to Bell’s modified criterio 14. All stages were included.
The patients were divided into two groups: with and without AKI. Data such as gender, birth weight, gestational age, Apgar score at 1 and 5 min, basal creatinine level, and sepsis were compared between no AKI and AKI groups. The quantitative variables were analyzed with independent t-test and qualitative variables using the χ2 test and Mann-Whitney U test.
AKI stages 2 and 3 were grouped and defined as severe AKI for the analysis of risk factors and mortality.
Univariate logistic regression was conducted for each variable, and significant variables (with a p-value of 0.25 or lower) were included in a multivariate logistic regression to assess independent risk factors for AKI development. Survival was evaluated using a Kaplan-Meier curve with the log-rank test and the hazard for mortality with a Cox regression model; a p-value <0.05 was considered statistically significant. IBM SPSS Statistics (IBM Corp. Released in 2013. IBM SPSS Statistics for Windows, Version 21.0. Armonk NY: IBM Corp.) was used for statistical analysis.
Results
A total of 39 patients met the inclusion criteria, 19 females (48.7%) and 20 males (51.3%), with a mean birth weight of 1,618 g and 33 weeks of gestational age (WGA). Fifteen patients developed some degree of AKI (38.5%), of which 53.3% corresponded to severe AKI.
The mean birth weight was 1,686.3 g in the AKI group and 1575.4 g in the no AKI group. The mean gestational age differed by one week between both groups (33.7 vs. 32.6 WGA, respectively). Baseline serum creatinine showed no statistical difference between groups (p = 0.958). Apgar scores at 1 and 5 min showed no significant difference between groups (Table 1).
Table 1 Characteristics of newborns with necrotizing enterocolitis
| No AKI | AKI | p value | OR | p value | |
|---|---|---|---|---|---|
| Male, n (%) | 13(54.2) | 7 (46.6) | 0.648 | 1.351 | 0.649 |
| Female, n (%) | 11(45.8) | 8 (53.4) | |||
| Birth weight (g), mean (SD) | 1575.4 (617.2) | 1686.3 (561.3) | 0.576 | 1.000 | 0.565 |
| Gestational age (weeks), mean (SD) | 32.6 (2.98) | 33.7 (3.98) | 0.355 | 0.91 | 0.250 |
| APGAR 1 min, median | 7.0 | 7.0 | 0.268 | 0.594 | 0.078 |
| APGAR 5 min, median | 9.0 | 8.0 | 0.057 | 0.383 | 0.255 |
| Basal creatinine (mg/dl), mean (SD) | 0.5 (0.219) | 0.49 (0.514) | 0.958 | 0.950 | 0.956 |
| Positive blood culture, n (%) | 7 (29.1) | 3 (20) | 0.524 | 1.647 | 0.526 |
| Sepsis, n (%) | 10(41.6) | 8 (53.4) | 0.477 | 4.200 | 0.117 |
| Use of vasopressors, n (%) | 2(8.3) | 4 (26.6) | 0.123 | 0.250 | 0.321 |
| Bell’s stage 2B or greater, n (%) | 6 (25) | 11 (73.3) | 0.003 | 8.250 | 0.005 |
AKI: acute kidney injury; OR: odds ratio; SD: standard deviation.
For the analysis of risk factors in the univariate logistic regression, NEC stage 2B or higher showed increased odds to develop any stage of AKI (OR: 8.25, p = 0.005), and 21 times increased odds to develop severe AKI (p = 0.009). Sepsis, gestational age, Apgar score at 1 min, and the severity of NEC were selected to analyze independent risk factors.
In the multivariate logistic regression, for every decreasing point in Apgar at 1 min, the odds of developing some degree of AKI were 1.67 (p = 0.021). Moreover, for every increasing grade in the severity of NEC, the odds increased 84% for any stage of kidney failure and 0.91 times for severe AKI (p values of 0.034 and 0.027, respectively) (Table 2).
Table 2 Independent risk factors for acute kidney injury and severe acute kidney injury
| AKI | Severe AKI | |||||
|---|---|---|---|---|---|---|
| OR | 95%CI | p value | OR | 95%CI | p value | |
| Sepsis | 2.947 | (0.458‑18.972) | 0.255 | 3.879 | (0.506‑29.746) | 0.192 |
| Gestational age | 1.465 | (1.01‑2.116) | 0.044 | 1.098 | (0.801‑1.504) | 0.561 |
| APGAR 1 min | 0.374 | (0.162‑0.862) | 0.021 | 0.868 | (0.593‑1.270) | 0.466 |
| NEC severitya | 1.841 | (1.047‑3.236) | 0.034 | 1.917 | (1.076‑3.413) | 0.027 |
AKI: acute kidney injury; NEC: necrotizing enterocolitis; OR: odds ratio; CI: confidence interval; APGAR: Appearance, Pulse, Grimace, Activity and Respiration.
aaccording to Bell’s staging.
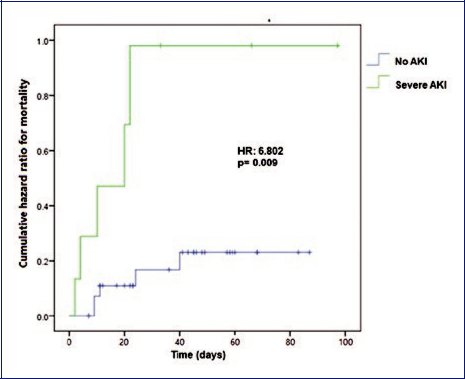
The overall mortality was 25.6%. The mortality was 46.7% in the AKI group and 12.5% in the without AKI group (p = 0.017) but increased up to 62.5% in the severe AKI (stages 2 and 3) group with a p-value of 0.007 when compared to the rest of the patients (16.1%). The survival at 30 days showed to be lower in the AKI group with a p-value of 0.005 (Figure 1).
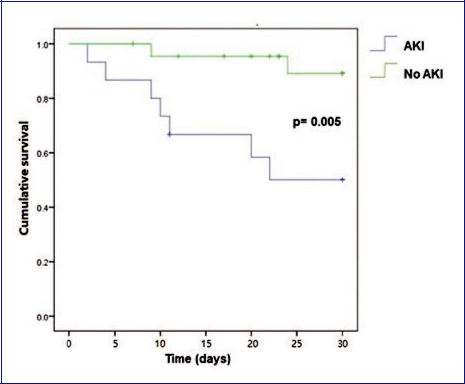
Figure 1 Survival plot of infants with necrotizing enterocolitis (acute kidney injury vs. no acute kidney injury).
The AKI hazard ratio (HR) for mortality was 4.70 (p = 0.025) compared to no AKI. When AKI stages 1 and 2 were compared alone, no significant increase in HR was observed (2.49, p = 0.31 and 1.76, p = 0.62, respectively). Conversely, AKI stage 3 showed an HR increase of 42.21 times for mortality (p = 0.001). Furthermore, when compared to the rest of the patients, AKI stage 3 showed an HR of 5.04 (p = 0.011). Severe kidney failure was related to an increase in mortality (HR= 6.802, p = 0.009), with the significant contribution of AKI stage 3 patients with a mortality of 100% (Figure 2).
Discussion
To the best of our knowledge, this study is the first to analyze the mortality of AKI in NEC patients in a Latin-American country.
In the study conducted by Li et al. 15 in which NEC in term infants was addressed, kidney failure occurred in 2.8% of the patients, which was associated with a higher frequency in the no survivor group. Similar to our findings, gestational age and birth weight showed no association as risk factors for mortality. However, when compared to the present study, a significant difference in the occurrence of kidney failure was reported, which may be attributed to the inclusion of preterm, as well as term infants.
Criss et al. observed that 54% of the patients with NEC had AKI. In their analysis, no risk factors were significantly related to the development of kidney failure. The mortality appeared to be higher in patients with kidney injury with an HR = 2.4 (p = 0.009) 16. In this work, not only the hazard for AKI was analyzed but for the different stages, finding that the HR increases proportionally to kidney failure severity.
In a study published in 2018, including infants with stage 2 NEC or higher, AKI was reported in 42.9% of the patients. Bell’s stage 3, lower gestational age, maternal preeclampsia/eclampsia, and the use of nephrotoxic antibiotics were reported as independent risk factors for AKI, with a mortality of 69.7% 17. Similar to our study, the severity of NEC showed to be an independent risk factor. However, maternal factors and exposure to nephrotoxic drugs were not addressed due to the deficient chart registry.
Despite the differences with other reports, AKI was found to increase mortality in patients with NEC in this study. A possible explanation for the variations in mortality could be the availability of resources for diagnosis and treatment in different hospitals.
The role of gestational age, birth weight, and other factors in survival seemed to be inconsistent. However, the severity of NEC appears to be the principal risk factor to develop AKI.
Some limitations in this analysis are the small sample size and an inadequate chart registry. NEC and AKI continue to be important complications in newborns, especially in preterm infants. NEC by itself is a risk factor to develop AKI, and kidney injury increases the mortality in these patients.
In conclusion, every newborn with NEC should be evaluated to recognize AKI early and provide adequate treatment to avoid fluid, electrolytes, and acid-base disturbances, and maintain adequate homeostasis.
Further studies with a larger number of patients are necessary to identify modifiable risk factors and impact in the prevention of these conditions, as well as more reports from developing countries to assure a better registry of these patients.











 nueva página del texto (beta)
nueva página del texto (beta)