Introduction
Craniosynostosis is characterized by a premature sutural fusion that can occur as a sole entity or associated with other anomalies. As a syndrome, craniosynostosis is a heterogeneous condition related to more than 180 syndromes1. Apert syndrome (AS) (OMIM 101200) was first described in 1906 by Dr. Eugene Apert, a French pediatrician, who designed it as acrocephalosyndactyly type I2,3. Craniosynostosis occurs in approximately 1/65,000 to 200,000 live births with Apert syndrome2,3-5, which represents 3% of all craniosynostosis. This syndrome affects equally male and female patients3,5. Two different types of mutations have been found on the fibroblast growth factor receptor-2 gene (FGFR2, OMIM 176943, NM_001144916.1) in several syndromic craniosynostoses, including AS. Inheritance pattern of AS is autosomal dominant, and over 98% of cases have de novomutations2-7.
Clinical features of AS, including craniosynostosis3, are characterized by bilateral coronal suture fusion (acrocephaly)2 with a diminished anteroposterior diameter, flat occiput3, and abnormal cranial base development2, prominent forehead, hyperteleorism3,6, downward sloping palpebral fissures6, proptosis3,6, strabismus4, depressed nasal bridge3, midface hypoplasia3,4,6, low-set ears8, a trapezoidal-shaped mouth6, prominent mandible3, high-arched or cleft palate3, bifid uvula2, delay in dentition, abnormal and crowded dentition3,6 and pharynx defects frequently result in airway compromise8, symmetrical syndactyly of the hands and feet3,5,6, symphalangism and radio-humeral fusion. The multiple abnormalities of the central nervous alterations include hydrocephalus2, ventriculomegaly2,4, alterations of the septum pellucidum2, corpus callosum2,4, and limbic structures2. Additionally, cardiac, gastrointestinal, urogenital, vertebral anomalies4 and short stature have been reported4,5. Furthermore, psychomotor development may be delayed3,6, with variable degrees of neurocognitive impairment2,8; blindness and hearing loss6 can be observed. A multidisciplinary approach is required for the management of this entity due to this multisystem involvement3.
In this work, we report two Venezuelan female patients with clinical features of AS with heterozygous mutations (c.755C>G; p.Ser252Trp) in the FGFR2 gene, with the objective of recognizing this uncommon entity through clinical findings, highlighting interdisciplinary medical evaluation, and providing timely genetic counseling for the family.
Methods
Both patients diagnosed with AS were clinically evaluated in the Unit of Medical Genetics, Department of Pediatrics, University of The Andes, Mérida, Venezuela. Diagnostic molecular genetic tests were performed in the Department of Medical Biology and Genetics, Akdeniz University Medical School, Antalya, Turkey, in concordance with the institutional review board protocols approved by the ethics committees under the most recent version of Helsinki Declaration. Signed informed consent was obtained from the parents of the patients.
Genomic DNA of the patients and the parents were isolated from peripheral blood samples for diagnostic molecular genetic analysis by a modified non-enzymatic method from Lahiri and Nurnberger9. Amplification of genomic DNA was performed using previously described primers and conditions in a standard polymerase chain reaction10. DNA sequencing analysis was performed using the Big Dye Terminator Kit v3.1 (Applied Biosystems) and an ABI 3130XL Genetic Analyzer (ABI Prism, USA). The sequencing data were compared with GenBank (NM_022976) sequences by using NCBI blast suite (https://blast.ncbi.nlm.nih.gov). Mutation nomenclature was done based on Human Genome Variations Guidelines.
Case reports
Case 1
A three-day-old newborn female patient with craniosynostosis and symmetric syndactyly of hands and feet. Healthy and non-consanguineous parents, a 27-year-old mother and a 24-year-old father. She was born at term at 38 weeks of gestation by vaginal delivery after a complicated pregnancy with urinary tract infection, which was treated. Weight at birth, 2,840 g (-1 standard deviation (SD)); length, 50 cm (-0.1 SD); head circumference, 38 cm (> 97th percentile). Apgar scores of 7 at 1 minute, and 9 at 5 minutes. No family history of similar alterations or any other congenital anomalies were reported.
Physical examination of the patient revealed abnormal acrocephaly, prominent frontal region, and flat occiput. She also had ocular proptosis, hypertelorism, and down-slanting palpebral fissures. In addition to these symptoms, she had midfacial hypoplasia, broad nasal root, depressed nasal bridge, thick nose with a bulbous tip, open mouth with crossbow-shaped lips and intraorally cleft soft palate; also, low ear implantation, overfolded helix, dysplasia of the auricle and short neck (Fig. 1A). She had symmetrical syndactyly of hands (Fig. 1B), feet and bilateral pes cavus.
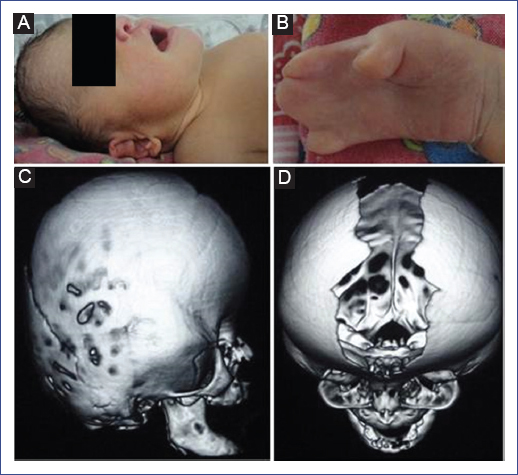
Figure 1 A. Acrocephaly, prominent frontal region, depressed nasal bridge, bulbous tip, open mouth, low ear implantation, overfolded helix, dysplasia of the auricle and short neck. B. Cutaneous syndactyly of the hand. C. Computed tomography of the skull in 3D shows diminished anteroposterior diameter. D. Complete closure of both coronal sutures and diastasis of the parietal and metopic sutures.
The newborn screening tests results were normal. 3D-Computed tomography of the skull showed asymmetry with increased cross-sectional and diminished anteroposterior diameters. Complete closure of both coronal sutures and diastasis of the parietal and metopic sutures (Figs. 1C and 1D) were observed. Besides, facial hypoplasia and hypertelorism were evident, without other alterations. Transthoracic echocardiogram showed patent foramen oval and patent ductus arteriosus with subsequent successful closure. Abdominal ultrasound was normal. The molecular genetic analysis for exons IIIa and IIIc of FGFR2 gene (Fig. 2) revealed a heterozygous missense mutation (c.755C>G; p.Ser252Trp).
Case 2
A two-month-old female patient with craniosynostosis and symmetric syndactyly of hands and feet. She was born at term at 40 weeks of gestation by cesarean delivery without complications. Healthy and non-consanguineous parents, a 23-year-old mother and a 24-year-old father. Weight at birth, 3,390 g (0.6 SD); length, 52 cm (2.1 SD); and head circumference, 37.8 cm (> 97th percentile). Apgar scores of 8 at 1 minute, and 9 at 5 minutes. No family history of similar alterations or any other congenital anomalies were reported.
As a result of physical examination, abnormal acrocephaly, prominent frontal region and flat occiput, ocular proptosis, hypertelorism, and down-slanting palpebral fissures were observed. Additionally, the patient showed midfacial hypoplasia broad nasal root, depressed nasal bridge, thick nose with a bulbous tip, open mouth with crossbow-shaped lips and intraorally high arched palate. Short neck and symmetrical syndactyly of hands and feet were also determined (Fig. 3).
The newborn screening tests results were normal. Transthoracic echocardiogram showed large ostium secundum atrial septal defect with moderate hemodynamic repercussion and small muscular ventricular septal defect. Abdominal ultrasound was normal. Genetic analysis of the patient revealed a heterozygous mutation (c.755C>G; p.Ser252Trp) in the FGFR2 gene.
Discussion
Mutations in the FGFR2 gene can be found in several syndromic craniosynostoses, including Apert (OMIM 101200), Crouzon (OMIM 123500), Pfeiffer (OMIM 101600), Beare-Stevenson (OMIM 123790) and Jackson-Weiss (OMIM 123150) syndromes1,11. Genetic mutations in AS were discovered for the first time in 1995 by Wilkie, et al.2; they occur as a result of heterozygous mutations in FGFR2 gene located at 10q25.3-264,7, which encodes a tyrosine kinase receptor gene that regulates multiple cellular activities, such as cell growth, differentiation, and embryonic development13. Two adjacent missense mutations-c.755C>G and c.758C>G, resulting in p.Ser252Trp (66%) and p.Pro253Arg (32%) respectively2,5,8,11,12,14-are related to AS. These mutations occur in a highly conserved region in the immunoglobulin-like extracellular subdomains of exon IIIa of FGFR2 gene in >98% of the cases of AS8,11,14. The first mutation is tightly associated with a more severe craniofacial phenotype11,13and cleft palate13, while the second is associated with more severe syndactyly11,13. Of the two cases reported here, only case 1 presented cleft palate. Other uncommon mutations in FGFR2 gene have been described in AS, such as c.756_758delGCCinsCTT15, c.755_757delCGCinsTCT16, c.755_756CG>TC, c,755_756CG>TT17, partial gene deletion, and Alu element insertion18.
AS is an entity with an autosomal dominant inheritance pattern, with 98% of cases due to de novo mutations2. These causative mutations are transmitted in the paternal chromosome, which is why advanced paternal age could be a risk factor for this entity2,8,13. However, the parents of the two cases described in this article are not of advanced age.
Craniosynostosis is a group of various symptoms that exhibit distinctive clinical findings with a wide range of clinical manifestations; the severe ones could result in neonatal death. Syndromic craniosynostosis is the hereditary form of alterations of the skull associated with extracranial phenotypes such as the central nervous system, cardiac and limbs malformations8. Both of the present cases showed congenital heart disease. Therefore, it is suggested that the cardiovascular evaluation should be part of the medical studies. The significant phenotypic variability observed in AS is not only due to genetic alterations, but also the environmental or supplemental genetic factors2. Thus, a team of clinicians and medical geneticists is required for diverse evaluations1.
Prenatal diagnosis of AS is based on the ultrasonographic findings of abnormal skull shape, which include prematurely ossified coronal sutures, widely separated metopic suture, midfacial hypoplasia, and bony or cutaneous syndactyly of extremities19. The recurrence risk of having a child with this entity for an affected parent is of 50%20. Since the presence of unaffected/healthy parents, the condition described here is accepted as sporadic. The diagnosis is usually based on the physical features of the patients, and the molecular genetic analysis may be very helpful to confirm the diagnosis4.
In the case of a patient diagnosed with AS, an interdisciplinary medical evaluation consisting of assessments by Neurosurgery, Neuropediatrics, Stimulation Therapies, Psychology, Ophthalmology, Otorhinolaryngology, Maxillofacial Surgery, Cardiology, Orthopedics, and Medical Genetics is necessary. In the cases presented here, the molecular studies performed on the parents did not show the mutation. In cases with de novo mutations, the risk is 50% for the descendants of those affected and not for their siblings; however, germinal mosaicism cannot be rule out.
In conclusion, two cases of AS are presented in order to highlight the differences in clinical findings. These cases were recognized by the different treating physicians who intervened in their interdisciplinary evaluation. The interpretation of the FGFR2 mutations in patients with clinical features of syndromic craniosynostosis offers a significant benefit regarding prognosis, genetic counseling, and prenatal diagnosis.











 nueva página del texto (beta)
nueva página del texto (beta)




