Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Boletín médico del Hospital Infantil de México
versão impressa ISSN 1665-1146
Bol. Med. Hosp. Infant. Mex. vol.68 no.6 México Nov./Dez. 2011
Artículo original
Coexistence of obesity and anemia in children between 2 and 18 years of age in Mexico
Pompilio Torres Ornelas1, Juan José Evangelista Salazar2, Homero Martínez-Salgado3,4
1 Departamento Estatal de Calidad en Salud, Secretaría de Salud y Bienestar Social, Colima, México
2 Departamento de Pediatría, Hospital General de Zona y Medicina Familiar No. 1, Instituto Mexicano del Seguro Social, Colima, México
3 Dirección de Investigación Médica, Hospital Infantil de México Federico Gómez, México D.F., México
4 RAND Corporation, Santa Monica Office, Santa Monica, California
Correspondence:
Dr. Homero Martínez Salgado
Dirección de Investigación Médica Hospital Infantil
de México Federico Gómez, México, D.F., México
E-mail: homero@rand.org
Received for publication: 9-21-11.
Accepted for publication: 10-20-11.
Abstract
Background. According to the most recent national nutrition survey (ENSANUT 2006) in Mexico, 18.4% of the population aged 5 years or older was obese, and 19.6% of those children aged 1 year or older were anemic. Although these are two of the most highly prevalent conditions, coexistence of both conditions has not been previously described at the national level.
Methods. We carried out a secondary data analysis to determine the frequency of anemia in different categories of body mass index (BMI) and the frequency in which obesity and anemia co-occurred in children between 2 and 18 years of age. We included data from 29,893 children <18 years of age.
Results. The highest prevalence of anemia was found among children with low BMI (13.1%), whereas in obese children the corresponding prevalence was 9.6%. Only 1.3% of children presented obesity and anemia, and its coexistence was observed mainly in children <5 years of age (p = 0.001). Being female and being <9 years of age were the two factors significantly associated with the phenomenon under study.
Conclusions. The risk for coexistence of obesity and anemia varied according to the gender and age of the children. Integral nutrition education programs are required to simultaneously address both of these issues.
Key words: coexistence, obesity, anemia, children.
Introduction
In recent years there has been a relatively new phenomenon described in countries undergoing the nutrition transition; this phenomenon is related to the combination of undernourished children and overweight adults.1 This situation has been found to coexist frequently in the same family and generates a "double burden" of malnutrition at the household level.2 Both in Asia and Latin America, it is not uncommon to find overweight or obese women who are the mothers of undernourished children. Mexico does not escape this unhealthy situation.3,4 These women, although obese, often also present with different micronutrient deficiencies as a result of unbalanced diets that are rich in calorie-dense foods but deficient in essential nutrients.4,5 Actually, in several countries the co-occurrence of anemia and obesity has been described as a paradox of the nutrition transition. The paradox is that an improvement in the economic and social environment with the consequent increase in access to a larger variety of food and health services is not necessarily accompanied by an improvement in the health status of the population.3-6
Overweight/obesity and iron deficiency are two of the most common health problems worldwide. Both are more prevalent among persons from lower socioeconomic groups who consume low-cost, calorie-dense foods, rich in refined sugar, fat, and preservatives, but low in essential micronutrients.7 In Mexico, the most recent national nutrition survey has shown that children >5 years of age have a prevalence of obesity of 18.4%. This prevalence increases with age, is different according to gender, and shows differences related to the locality of residence (urban/rural).6 Anemia affects 19.6% of children >1 year old and as is the case with obesity, the prevalence is affected by gender and by place of residence. Anemia prevalence is higher between 1 and 2 years of age,8 during adolescence,9 and in pregnant women;9 in older ages, it shows trends toward increments similar to those found with obesity.7
Even when obesity and anemia affect important segments of the population with prevalence high enough to be considered public health problems,7,10,11 coexistence of these two conditions has not previously been described in Mexico at the national level. The objective of the present study was to determine the prevalence of anemia in children between the ages of 2 and 18 years old in Mexico according to categories of body mass index (BMI).
Methods
We conducted a secondary analysis of data collected by the National Institute of Public Health (INSP) for the National Health and Nutrition Survey 2006 (ENSANUT). A full description about the methods used, sampling framework, sample size, and field procedures may be found in the original description of the study.7 In brief, the survey was designed following a cluster randomized selection of households based on information provided by the National Institute of Statistics, Geography and Informatics (INEGI) to provide a representative sample of the country. To access the database, the authors followed the established procedure to request access to the data from INSP, which provided information on 71,469 participants of both genders and all ages.
For the present analysis, we included males and females between 2 and 18 years of age who had complete information for our analyses. We excluded BMI data from males or females between 2 and 11 years of age when values were <10 kg/m2 or >38 kg/m2, females declared to be pregnant, and adolescent males or females whose BMI was <10 kg/ m2 or >58 kg/m2. We also excluded data, regardless of age or gender, when hemoglobin values were <40 g/l, males <12 years old or females between 12 and 18 years of age with hemoglobin values >185 g/l and males >12 years old with hemoglobin values >200 g/l.
Study variables included the following:
• Age—we defined four categories: children <5 years of age, children between 5 and 9 years of age, children between 10 and 14 years of age and children between 15 and 18 years of age.
• Gender.
• Body mass index (BMI) categories—BMI results from dividing body weight (in kg) by the square of height in meters (kg/m2) and classified by age and gender according to the recommendations by the World Health Organization.12,13 According to BMI, the child's nutritional status was classified as low when it was <-2 standard deviations (SD), normal when it was between -2 and +1 SD, overweight when it was between +1 and +2 SD, and obese when it was >2 SD.
• Hemoglobin value to identify anemia—cut-off value for hemoglobin was adjusted according to altitude above sea level of the child's place of residence. When altitude was >1000 m above sea level, we used the equation recommended by Ruiz-Argüelles and Llorente-Peters14 except for females 12 years of age or older, in which case we used that recommended by Cohen and Haas.15 Altitude above sea level was defined from the catalogue for states, municipalities, and locales published by INEGI.16 Anemia was thus defined at the individual level when the altitude-adjusted cut-off value was below the thres-hold, adjusting for child's age and gender.
• Socioeconomic status—categorized in four strata according to the number of monthly minimum wages of the household. Stratum I included households with monthly income ≤2 minimum wages, stratum II were households with >2 and ≤4 minimum wages, stratum III were households with >4 and up to ≤7 minimum wages, and stratum IV were households with >7 minimum wages.
• Place of residence—urban or rural according to the size of the locality, over or under 2,500 inhabitants, respectively.
• Coexistence of obesity and anemia.
We carried out data analyses using the statistical package SPSS v.17.0. Descriptive statistics included frequency of distribution and percentages. Bivariate analyses were carried out by means of a χ2 statistic with 95% confidence intervals. Multivariate analyses were carried out resorting to dichotomous logistic regression with a model that included gender, age group, socioeconomic stratum, and rural/urban locality as independent variables, and the coexistence of overweight/obesity and anemia as the dependent variable.
Results
We analyzed data from 29,893 individuals located in the 31 states of Mexico and the Federal District. Of these individuals, 14,822 (49.6%) were female and 15,071 (50.4%) were male. When analyzing according to age groups, 4,736 (15.8%) were between 2 and 5 years old, 9,727 (32.5%) were between 5 and 9 years old, 10,470 (35.0%) were between 10 and 14 years old, and 4,960 (16.6%) were between 15 and 18 years old. Considering a household's monthly income, 15,854 belonged to stratum I (53%), 6,407 to stratum II (21.4%), 6,095 to stratum III (20.4%), and 1,537 to stratum IV (5.1%). Regarding place of residence, 18,399 subjects resided in urban areas (61.5%) and 11,494 resided in rural areas (38.5%). For BMI, 536 cases (1.8%) were low; 19,179 (64.2%) were normal; 6,218 cases (20.8%) were overweight; and 3,960 cases (13.2%) were classified as obese. The lowest prevalence of obesity (10.0%) was found in children <5 years of age, whereas the highest prevalence of obesity (15.4%) was found in the age group of 10-14 years old (χ2 = 159.27, p <0.001, Table 1). In relation to the altitude of the locality of residence, 16,178 cases (54.1%) lived at >1000 m above sea level and, applying the correction to the hemoglobin cut-off value, 3,358 cases (11.2%) were found to be anemic.
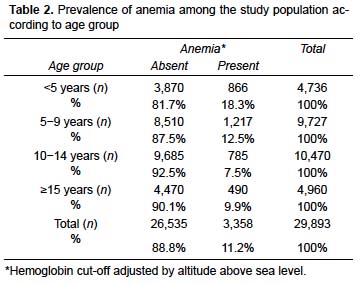
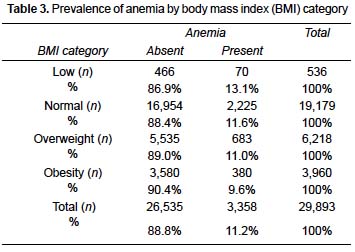
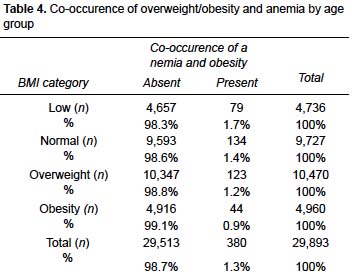
Anemia varied by age group, with the highest prevalence (18.3%) found in children <5 years of age (χ2 = 407.80, p <0.001, Table 2). Anemia also varied by BMI status, with the highest prevalence (13.1%) among those with low BMI and the lowest prevalence (9.6%) among those with obesity (χ2 = 15.43, p =0.001, Table 3). When overweight and obese children were grouped, the prevalence of anemia was 10.4%. Obesity and anemia co-occurred in only 380 cases, corresponding to 1.3% of the overall sample. The highest prevalence (1.7%) was found among children <5 years of age, whereas the lowest prevalence (0.9%) was found among those between 15 and 18 years of age (χ2 = 15.43, p = 0.001, Table 4).
Logistic regression analysis showed gender (female) and age group (<5 years of age, between 5 and 9 years of age) to be significant risk factors for the co-occurrence of obesity and anemia, whereas belonging to the two lower socioeconomic strata, corresponding to less than two minimum wages and between two and four minimum wages, lowered this risk (Table 5).
Discussion
The evidence published so far about the association between obesity and anemia has been inconsistent. Even with few published studies, their findings may be classified in three groups: (1) those that found no relationship between hematologic variables when comparing obese and nonobese individuals;17,18 (2) those that found differences, which may be subdivided according to the following: a) those that compare mean values of hemoglobin, hematocrit, and serum ferritin to conclude that obese individuals have higher values as compared to non-obese individuals,4,19-21 b) those that, comparing prevalence of anemia in different BMI groups, conclude that obese individuals have a higher risk of anemia than non-obese individuals;4,5,22-24 and (3) those that, without making comparisons, describe the frequency of anemia in individuals with obesity.4,22,23,25-27
Such variability in results, with findings that seemingly contradict one another, may be due to lack of a biological explanation regarding this relationship, which could be a result of a complex set of environmental and individual variables including differences in economic, social, cultural, and health variables.23,25-27 Therefore, there may be differences between study results because of methodological differences as well as contextual variables, including time and place. Thus, Fricker et al. conducted their study in 1990;20 King et al. carried out their study in Guatemala in 1997;21 Ávila-Curiel et al. studied their population in Mexico in 2002;25 Pinhas-Hamiel et al. carried out their study in Israel in 2003;24 Nead et al. carried out their study in the U.S. in 2004;28 Al-Hashem, in Arabia in 2007;19 and Ernst et al. in Switzerland in 2008.22
In our own study there were several relevant findings. First, the highest prevalence of anemia was found among children with low BMI, and this combined with the finding that the highest prevalence of anemia coexisting with obesity was found in children <5 years of age. Next, there was an increased risk for the coexistence of anemia and obesity associated with gender. Females <5 years of age and those between 5 and 9 years of age were more vulnerable to this condition despite the fact that the prevalence of obesity among these age groups was not the largest in the study sample.
These three findings are particularly relevant when considering the likely causes for our findings as well as potential interventions. We believe that both overweight/obesity and anemia share nutrition as a common origin. Anemias from nutritional origin are the most common type of anemias found worldwide and can be due to a deficiency of one or more micronutrients in the diet. Iron deficiency has often been invoked as the most common one in nutritional anemia and results from inadequate intake and/or low bioavailability of iron in food. Other micronutrient deficiencies may also cause nutritional anemia, including insufficient folic acid, vitamin B , and zinc.11,29-31
Likewise, the most common cause of overweight and obesity is excessive caloric intake in relation to food consumption; this is usually associated with a lack of physical activity.10,32
As shown in other studies, an increase in food consumption does not necessarily lead to better dietary quality.33 This is precisely what leads to a double burden of malnutrition, manifested on the one hand as overweight/obesity and on the other by a deficiency in one or more micronutrients, which lead to limitations in physical growth and functional performance.2,22,28,34 Actually, micronutrient deficiencies have been referred to by some authors as the "hidden hunger"33 because the person whose diet is deficient in specific micronutrients does not feel the need to ingest that micronutrient. This is markedly different from the feeling of hunger triggered by hypoglycemia, which motivates the individual to search for calorie-rich foods. On the other hand, obesity has been referred by some authors as "the most widely extended form of malnutrition." It affects developing countries disproportionally, particularly those segments of the population with more constraints in the elasticity of their expenditures, which does not allow them to select and consume a varied and well-balanced diet.1-4,6,35
Looking at our other main findings, we should highlight the presence of anemia in children with low BMI. This may be the result of an overall deficient diet, limited in macro and micronutrients, a situation commonly found among segments of the population with limited resources and limited information about how to balance their diet based on foods that are available and affordable. In our analyses, we found a reduced risk ("protective effect") for the co-occurrence of obesity and anemia among the population in the two lower economic strata. It is also important to highlight that in this study, as in many other studies looking at health and nutrition in developing countries, we found that gender and age are two important and significant risk factors related to health inequalities. In our case, females and children <9 years of age were more vulnerable for the double burden of malnutrition addressed in this article.
For purposes of comparison of our results and those from other studies, we want to stress the need to correct hemoglobin values by altitude over sea level in order to define the cut-off for anemia. Although this has been noted by other authors,36 this correction is not done systematically. We also want to highlight the use of the most recent growth curves published by WHO for children and adolescents to classify BMI satus.12,13
In our view, the topic under study is far from being exhausted. There is still much to be done to understand whether the health risks posed for the individual by overweight/obesity and anemia are combined or synergized when both conditions co-occur. From a clinical point of view, nutrition education programs must be reevaluated and better focused to improve knowledge that will lead to better food consumption based on a complete and wellbalanced diet that may support a good nutritional status, ideally associated with healthy lifestyle practices.
As a general recommendation for screening programs for anemia, we highlight the need to include individuals who are overweight or obese because these conditions neither represent "overnutrition" nor do they eliminate the risk of finding one or more nutritional deficiencies traditionally associated with undernutrition. Based on our findings, females and children <9 years of age should receive special attention because these proved to be the most significant risk factors for the co-occurrence of the two conditions under study. In cases where anemia and overweight/obesity co-occur, it is necessary to install an integral treatment, including a solid component of nutrition education, which may improve dietary intake while simultaneously fostering behavior changes that can be sustained in the long term to address these two common public health problems.
References
1. Caballero B. A nutrition paradox—underweight and obesity in developing countries. N Engl J Med 2005;352:1514-1516. [ Links ]
2. Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obesity 2005;29:129-136. [ Links ]
3. Barquera S, Peterson K, Must A, Rogers B, Flores M, Houser R, et al. Coexistence of maternal central adiposity and child stunting in Mexico. Int J Obes (Lond) 2007;31:601-607. [ Links ]
4. Eckhardt C, Torheim LE, Monterrubio E, Barquera S, Ruel MT. The overlap of overweight and anaemia among women in three countries undergoing the nutrition transition. Eur J Clin Nutr 2008;62:238-246. [ Links ]
5. Batista M, de Souza A, Miglioli T, Carvalho M. Anemia e obesidade: um paradoxo da transição nutricional brasileira. Cad Saúde Pública 2008;24(suppl 2):S247-S257. [ Links ]
6. Fraser B. Latin America's urbanisation is boosting obesity. Lancet 2005;365:1995-1996. [ Links ]
7. Olaiz-Fernández G, Rivera-Dommarco J, Shamah-Levy T, Rojas R, Villalpando-Hernández S, Hernández-Ávila M, Sepúlveda-Amor J. Encuesta Nacional de Salud y Nutrición 2006. Resultados por Entidad Federativa. Cuernavaca, México: Instituto Nacional de Salud Pública–Secaretaría de Salud; 2007. [ Links ]
8. Villalpando-Hernández S, Shamah-Levy T, Ramírez-Silva CI, Mejía-Rodríguez F, Rivera JA. Prevalence of anemia in children 1 to 12 years of age. Results from a nationwide probabilistic survey in Mexico. Salud Publica Mex 2003;45(suppl 4):S490-S498. [ Links ]
9. Villalpando-Hernández S, García-Guerra A, Ramírez-Silva CI, Mejía-Rodríguez F, Matute G, Shamah-Levy T, et al. Iron, zinc, and iodide status in Mexican children under 12 years and women 12-49 years of age. A probabilistic national survey. Salud Publica Mex 2003;45(suppl 4++):S520-S529. [ Links ]
10. Secretaría de Salud. Norma Oficial Mexicana NOM-174-SSA1-1998. Para el manejo integral de la obesidad. Mexico; 2000. Available at: http://www.salud.gob.mx/unidades/cdi/nom/174ssa18.html [ Links ]
11. Martínez-Salgado H, Casanueva E, Rivera-Dommarco J, Viteri F, Bourges-Rodríguez H. La deficiencia de hierro y la anemia en niños mexicanos. Acciones para prevenirlas y corregirlas. Bol Med Hosp Infant Mex 2008;65:86-99. [ Links ]
12. De Onis M. WHO child growth standards for 0-60 months. Geneva: World Health Organization; 2006. [ Links ]
13. De Onis M, Onyango A, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for schoolaged children and adolescents. Bull WHO 2007;85:660-667. [ Links ]
14. Ruiz-Argüelles G, Llorente-Peters A. Predicción algebraica de parámetros de serie roja en adultos sanos residentes en alturas de 0 a 2,670 metros. Rev Invest Clin 1981;33:191-193. [ Links ]
15. Cohen J, Haas J. Hemoglobin correction factors for estimating the prevalence of iron deficiency anemia in pregnant women residing at high altitudes in Bolivia. Pan Am J Public Health 1999;6:392-399. [ Links ]
16. Instituto Nacional de Estadística y Geografía (INEGI). Catálogo de claves de entidades federativas, municipios y localidades, México. Available at: http://mapserver.inegi.org.mx/mgn2k/?c=646&s=est. [ Links ]
17. Scheer JC, Guthrie HA. Hemoglobin criteria with respect to obesity. Am J Clin Nutr 1981;34:2748-2751. [ Links ]
18. Seltzer CC, Mayer J. Serum iron and iron-binding capacity in adolescents. II. Comparison of obese and nonobese subjects. Am J Clin Nutr 1963;13:354-361. [ Links ]
19. Al-Hashem FH. Is it necessary to consider obesity when constructing norms for hemoglobin or when screening for anemia using hemoglobin levels? Saudi Med J 2007;28:41-45. [ Links ]
20. Fricker J, Le Moel G, Apfelbaum M. Obesity and iron status in menstruating women. Am J Clin Nutr 1990;52:863-866. [ Links ]
21. King J, Mazariegos M, Valdez C, Castañeda C, Solomons N. Nutritional status indicators and their interactions in rural Guatemalan elderly: a study in San Pedro Ayampuc. Am J Clin Nutr 1997;66:795-802. [ Links ]
22. Ernst B, Thurnheer M, Schmid SM, Schultes B. Evidence for the necessity to systematically assess micronutrient status prior to bariatric surgery. Obes Surg 2009;19:66-73. [ Links ]
23. Anaya-Loyola MA, Sosa-Álvarez C, Vergara-Catañeda H, Suaste-Duarte E. High prevalence of obesity in rural Mexican women. FASEB J 2006;20:A1033. [ Links ]
24. Pinhas-Hamiel O, Newfield RS, Koren I, Agmon A, Lilos P, Phillip M. Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int J Obes 2003;27:416-418. doi:10.1038/sj.ijo.0802224. [ Links ]
25. Ávila-Curiel A, Shamah-Levy T, Chávez-Villasana A, Galindo-Gómez C. Encuesta urbana de alimentación y nutrición en la zona metropolitana de la Ciudad de México 2002 (Estrato social Bajo). ENURBAL 2002. México D. F.: Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Instituto Nacional de Salud Pública; 2003. [ Links ]
26. Pajuelo J, Muñoz C, Ayquipa A, Ponciano W, López R. El sobrepeso, la obesidad y la anemia nutricional en la mujer adulta. An Fac Med Univ Nac Mayor San Marcos (Perú)2000;61:265-270. [ Links ]
27. Pajuelo J, Vergara G, De la Cruz G. Coexistencia de problemas nutricionales en niños de 6 a 9 años de edad, de centros educativos estatales de Matucana, Santa Eulalia y Lima. An Fac Med Univ Nac Mayor San Marcos (Perú) 2001;62:312-316. [ Links ]
28. Nead KG, Halterman JS, Kaczorowski JM, Auinger P, Weitzman M. Overweight children and adolescents: a risk group for iron deficiency. Pediatrics 2004;114:104-108. [ Links ]
29. World Health Organization, UNICEF. Joint statement by the World Health Organization and the United Nations Children's Fund. Focusing on anaemia. Towards an integrated approach for effective anaemia control. Geneva: World Health Organization; 2004. [ Links ]
30. Duque-López M, Flores-Hernández S, Flores-Huerta S, Méndez-Ramírez I, Muñoz S, Turnbull B, et al. Prevalence of anemia and deficiency of iron, folic acid, and zinc in children younger than 2 years of age who use the health services provided by the Mexican Social Security Institute. BMC Public Health 2007;7:345. [ Links ]
31. Villalpando-Hernández S, Pérez-Expósito AB, Shamah-Levy T, Rivera JA. Distribution of anemia associated with micronutrient deficiencies other than iron in a probabilistic sample of Mexican children. Ann Nutr Metabl 2006;50:506-511. [ Links ]
32. Organización Mundial de la Salud. Obesidad y sobrepeso. Nota descriptiva No. 311. Available at: http://www.who.int/mediacentre/factsheets/fs311/es/ [ Links ]
33. Trowbridge F, Harris SS, Cook J, Dunn JT, Florentino RF, Kodyat BA, et al. Coordinated strategies for controlling micronutrient malnutrition: a technical workshop. J Nutr 1993;123:775-787. [ Links ]
34. Fernald L, Neufeld L. Overweight with concurrent stunting in very young children from rural Mexico: prevalence and associated factors. Eur J Clin Nutr 2007;61:623-632. [ Links ]
35. Sebrell WH Jr. Changing concept of malnutrition. Am J Clin Nutr 1967;20:653-658. [ Links ]
36. Sullivan KM, Mei Z, Grummer-Strawn L, Parvanta I. Haemoglobin adjustments to define anaemia. Trop Med Int Health 2008;13:1267-1271. [ Links ]














