Servicios Personalizados
Revista
Articulo
Indicadores
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Boletín médico del Hospital Infantil de México
versión impresa ISSN 1665-1146
Bol. Med. Hosp. Infant. Mex. vol.67 no.2 México mar./abr. 2010
Artículo original
Evaluation of information provided to patients' relatives in an ambulatory pediatrics unit of a tertiary-care hospital
Rosa-Georgina Cabrales-Martínez, Edgar Bustos-Córdova, Yolanda Naranjo-López, Amapola Adell-Gras, and Jerónimo Sánchez-Medina
Consulta Externa, Hospital Infantil de México "Federico Gómez", México D.F., México
Autor de correspondencia:
Dr. Edgar Bustos-Córdova
Correo electrónico: edgarbus@yahoo.com.mx
Fecha de recepción: 10-07-09.
Fecha de aceptación: 22-01-10.
Abstract
Background: There is a high degree of misinformation given to the relatives of patients treated in the Ambulatory Pediatrics Unit at the Hospital Infantil de México Federico Gómez. The factors that contribute to this problem are diverse. Therefore, the practice implications as inadequacies in physician/patient communication lead to poor knowledge about a patient's illness and treatment. Attempts to improve the delivery of information may improve patient satisfaction and treatment compliance. The aim of this study was to quantify the percentage of patients' relatives who know the diagnosis, prognosis, and treatment of the patient's principal illness.
Methods: Using a face-validated questionnaire designed by the investigators, we inquired into the extent of information about the illness and treatment given to the relatives of patients attending the Ambulatory Pediatrics Unit at the Hospital Infantil de México Federico Gómez.
Results: Only 81, 75, and 68% of the participants were able to name the patient's illness, the affected organ, and the prognosis, respectively. The therapeutic drugs were correctly named by 85% of the participants. Only 72% of the relatives of patients who previously underwent surgery knew the name of the surgical procedure and 66% were able to briefly describe the procedure.
Conclusions: This study shows that communication between parents and pediatricians is limited. The implementation of new measures adapted to the individual case of each institution can contribute to improve the situation.
Key words: patient information, patient participation, communication barriers, persuasive communication.
Introduction
Most factors included in the complex phenomena of patient medical care depend on good communication between physicians and patients. Good communication generally leads to an optimal relationship between physician and patient, improves their level of satisfaction1-3 and even impacts on their clinical outcome.4 By improving communication, a lower index of errors with increased compliance with treatment is possible. It is possible to make decisions more freely by providing the patient with complete information regarding the clinical condition.
Communication can be affected by different factors. A complex situation for the physician is present when many different physicians are involved in a patient's care and each of them provides individual information. Such is the case with respect to patients who require care by different specialists. At the Hospital Infantil de México Federico Gómez, we have confronted this situation because the complexity of the patients' illnesses requires medical attention by a multidisciplinary team of specialists. Although receiving information from different sources could complement the process, this phenomenon frequently has the opposite effect when the same information is given using different words. This may lead to confusion on the part of the patients' relatives, particularly if we treat a lower socioeconomic population.
The information assimilated by patients' relatives has seldom been evaluated in our environment. Moguel has undertaken this evaluation as part of an investigation about patient's relatives' medical satisfaction.5 The investigators found that one-third of the users did not understand their illness and that there was little correlation between the diagnosis registered in the medical chart and the one mentioned by the patients.
A fundamental aspect is the possibility that the patients' relatives receive information from someone other than the treating physician. Patients' relatives frequently confound or misinterpret the information obtained from the Internet, magazines, or television.6 This can be difficult to overcome.
It is very important to know the level of the relative's assimilated information, which allows us to define the present situation in order to plan strategies to improve the quality of communication.
We believe that there is a high percentage of misinformation among the patient's relatives with respect to the illness, medications, and general treatment, although the actual situation is not known. The objective of this study was to quantify the percentage of patients who know the diagnosis, prognosis, and treatment of their principal illness. As far we know, there is no previous report regarding this in the medical literature.
Patients and methods
An observational, descriptive study was performed by means of an inquiry into the knowledge of the relatives of patients who attended the Ambulatory Pediatrics Unit at the Hospital Infantil de México Federico Gómez. The purpose was to explore the degree of knowledge about the patient's illness and treatment. The evaluation instrument was a questionnaire designed by the investigators.
Face validation of the information recollection instrument
No similar instrument exists in the published literature, which had been previously validated or tested to be universally accepted as a gold standard in this subject. It was decided to manage a procedure to validate the instrument, as described in the literature.7-11 The face validation process was managed in the following ways:
1. A preliminary questionnaire was elaborated based on the researchers' experiences, which should be answered strictly according to the operative definitions previously agreed upon.
2. The researchers evaluated the instrument and made corrections and suggestions to modify the document based on their collective experiences.
3. Pretest was developed in which the instrument was applied to a group of patients' relatives in the study population. The answers were carefully evaluated, as well as the difficulties in answering questions, and the instrument's practical applicability was determined. Corrections were made and a new version of the questionnaire was created.
4. The instrument was provided to a group of experts in the validation of instruments (two from the institution and one external) who evaluated each of the components of the questionnaire separately. They qualified the following: a) comprehension, b) clarity, c) concrete answers, d) ease in answering the components, e) compatibility with the objective, and f) possible consistency.
The experts were asked to suggest possible changes and to make comments. Based on this information, modifications to the questionnaire were made and a third version was obtained.
5. A second pretest was carried out with the third version of the instrument, which permitted some final modifications to be incorporated into the fourth and final version (the version utilized herein) (Fig. 1).
Once the instrument was face validated, the questionnaire was applied personally by one of the investigators who read the questions directly to the patient's relatives and recorded the answers in the described format.
A total of 100 surveys were included. The sample size was calculated using a previously published formula.12 For an expected proportion of 60%, which is the most approximated in a similar study previously published by our institution,5 it was decided to accept a maximum discrepancy of 10% according to the formula.
We included girls and boys from 0 months to 11 years 11 months of age who attended the Ambulatory Pediatrics Unit and had a clinical file with at least six consultations in some of the subspecialties or in the Ambulatory Pediatrics Unit and/or one hospitalization, assuring that the mother, father, or the primary caregiver was present. Patients from the Oncology and Nephrology Units were excluded because these patients have specific and personalized information that would create a skew with respect to the remainder of the patients. Patients without complete clinical files were excluded. None of the subspecialists was directly interviewed. The answers were compared with the information from the medical chart in order to evaluate their veracity. The prognoses of the patients were not measured or called in question.
Only descriptive analysis was carried out by calculating averages, percentages, and standard deviations.
Information was treated confidentiality and no informed consent was required.
Results
One hundred patients' relatives from the general population attending the Ambulatory Pediatrics Unit during January 2008 to June 2008 were sequentially polled. The ages were expressed in months, the youngest patient being 2 months old and the oldest patient being 11 years and 3 months old (mean: 4 years and 7 months) (Table 1). All patients had been previously seen in our Department. The time of attendance at the Hospital varied from 1 month to 10 years 9 months (mean: 2 years 9 months).
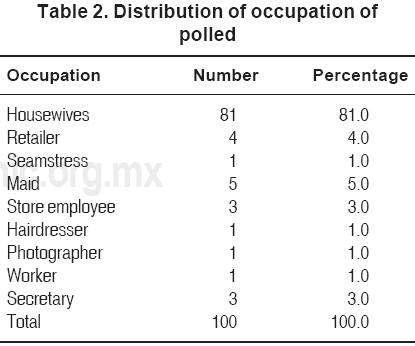
The age of the polled participants varied from 16-77 years (mean: 33.2 years). In 97% of the patients, the patient's mother was polled and only in three cases was the grandmother questioned. The education of the polled relatives was on average 9 years of schooling. Regarding occupation, 81% of the patient's relatives were housewives. The rest of the relatives reported other occupations from housekeepers to commercial activities (Table 2).
The specialties that managed the patients included in the study were divided into the following: adolescents, cardiology, immunodeficiency clinic, dermatology, endocrinology, gastroenterology, genetics, hematology, Infectious Diseases Clinic, pneumology, surgical specialties (general surgery, cardiovascular surgery, plastic surgery, tumor surgery, neurosurgery, ophthalmology, orthopedics, and urology), and general pediatrics (Table 3). Thirty eight percent of the patients were referred by the genetics service, which is the service that sends most of the patients to the Ambulatory Pediatrics Unit.

The number of specialists who treated the patients, in addition to the Ambulatory Pediatrics Unit, was from 1-14 (mean: 4.4). This included specialists who treated patients at any time while being monitored in the hospital as well as the specialists actively treating the patient. The mode was five specialties, which occurred in 18% of the population. Forty-nine percent of the patients previously were treated at another hospital.
A large percentage of the participants (89%) knew the name of the patient's illness and in most of cases (81%) they were able to refer to it correctly according to the diagnosis that was written down in the medical chart (Fig. 2). When asked what organ was affected by the illness, only 75% of the participants could properly identify the organ. Only 58% of the informants knew with certainty the prognosis of the illness; similarly, only 53% knew the risk of death associated with the illness.
Surgery was performed on 36% of the patients. Of these patients, 72% of the participants knew the name of the procedure. When asked about the procedure that was actually carried out, the percentage of the polled relatives who gave the correct answer was reduced to 66% (Fig. 3).

Forty-seven percent of the patients used different medications. From this group, 85% of the participants named all of the medications that were administered to the patient, 6.3% of the participants could partially name the medications, and 8.5% of the participants could not remember any of the medications (Fig. 4).

Discussion
A fundamental aspect in medical practice is the quality and certainty in the assimilation of information that the physician communicates to the patients and/or the patient's relatives. It is expected that the information is clear and appropriate, so much among the physicians as between them and their patients. It is expected that the information includes the patient's clinical condition, the possible evolution of the condition, and the treatment options. Good communication can influence better adherence to treatment, greater patient satisfaction, and a reduction of anxiety in the patient and patient's relatives.
The survey distributed as part of the current study yielded similar results to that of a preliminary study and reflects the unfavorable situation that is experienced by patients and their relatives.5 Recently, two studies showed similar disinformation when patients and patient's relatives were asked about their illness ("stroke"13 and chronic kidney disease14) even if they attended the medical facility for long periods. This is particularly significant in today's environment because patients actively participate in making decisions with regard to treatment.
The ethical aspects of medical practice do not omit the importance of patient participation in decision-making. This could not be possible without good and complete information because informed consent has assumed greater importance in the ethical and legal aspects of medical practice.15
Patient medication education in the hospital is a challenging task. Especially worrisome in our results is the patient knowledge regarding medications. A recent study proved that patient education supported by written educational materials for persons taking multiple medications for chronic diseases was beneficial in improving patient understanding of medications.16 Educating patients during their hospital stay on a daily basis has shown to be very helpful.17
In order to avoid errors in the interpretation of prescriptions, it would be helpful if the physician considered in advance the suppositions and beliefs of the patient and the patient's relatives. The consequences can be fatal if there are errors in prescription interpretation.18
Early education to chronically ill patients and relatives offers them diverse benefits including greater participation in their treatment, a positive effect in the evolution of the illness, and better therapeutic adherence.1-4 Patients cared for in a tertiary-care hospital and treated by high-level academic physicians expect to receive substantial information; nevertheless, our results are discouraging. We hypothesize that information received by the patient's relatives proceeded from different subspecialists, which may confuse them.
An alternate aspect not analyzed in the current study is the gap between patient expectations and the need for information and that which is actually received. The literature shows how important this problem is.19-21 Although patients in this hospital are almost exclusively representative of a lower socio-economic status, we see more patients from other social spheres, thus creating heterogeneity in information need and assimilation method. This preliminary study may be the basis for new studies that explore this problem.
Physician-patient communication: A complex process
The information disseminated to the patients' relatives is a very important component in the physician/ patient relationship and is frequently one of the most difficult problems to undertake. Affective and emotional factors have been considered to be important in the development of the complex communication process between physicians and patients.22,23 As was the case in this study, the greatest challenge occurs in large and complex medical centers where multi-disciplinary teams of physicians are involved in patient care.
It is important not only to know the patient's information needs with regard to their health, but also to offer treatment options for each case. Along the information process, the degree of comprehension by the patient and the judgment capability should be taken into account, as well as the way the physician communicates with the patients. Some investigators have remarked about the importance of including the patient in the information process and avoiding the excessive use of technical medical terminology in order to preserve the essential message.24
This aspect could explain, but not justify, the high percentage of misinformation shown in this study. The health professional responsible needs adequate training to detect the patient's problems and necessities to assist the patient in understanding the illness and the treatment to follow. One of the aspects that may influence successful communication process between the physician and the patient is the level of the parent's education. Our results reflect this condition. Other studies found similar conclusions.25 The survey revealed the low educational level of our population. This result was not unexpected because this is an institution dedicated to the care of patients who generally have a low socioeconomic status. Under these circumstances, transmitting the information correctly is a great challenge.
The institution in which this study was carried out is overcrowded and it is often difficult to provide a suitable amount of time for each patient. The time devoted to provide appropriate information is a fundamental factor to transmit a complete message and to permit patients to express their complaints and doubts. In the institutional and private environment, this factor may be one of the most difficult to surpass. The necessary time of attention for each individual patient depends on a great number of factors.26
Another essential aspect is outside sources of information to which the patient has access. The popular beliefs and the information communicated by relatives or acquaintances is an undeniable reality. Some investigators concur that patients frequently become confused or misinterpret information contained in mass communication media.27
Access to a large quantity of medical information via the Internet has complicated the process even more. The veracity of the information to which the patients have access is not always the best. In addition, there may be errors in the interpretation of what is read, or information may have been obtained after some manipulations with various goals.6,28
On the other hand, the presence of more than one relative during the interview could be considered disturbing in some cases. It may also be taken as an advantage to positively influence the physician/patient relationship and aid in the correct transmission of information.29
Diverse approaches to the problem
With concerns about the communication problem between physicians and patients and the conflict generated by the lack of information to patients, diverse approaches by medical groups and health systems have been proposed. It is important that health care personnel receive optimal training to provide adequate information to patients with regard to illnesses and treatments.
In Australia, the National Patient Safety Education Framework (NPSF) has been developed from the Australian Council for Safety and Quality in Health Care.30 This program has been designed to help medical schools and health organizations, as well as physicians in private practice, to develop aptitudes to work in a safe manner. Some of the topics that this program covers include effective communication, seeking to combine the patient's care among parents (or attendants) and physicians, communicating risks and adverse effects during the administered treatments, obtaining consents and being respectful of cultures and habits. Once initiated, this program has been successfully applied to medical students and postgraduate students in Australia.
A cross-sectional survey performed in four medical schools concluded that training and extensive supervised patient contact, especially if this teaching takes place in the initial years of the curriculum, improves communication skills.31
Another example would be the Forum for Applied Cancer Education and Training, directed by oncologists in the UK, which emphasizes the physician's communication skills.32
Features and models of training have been proposed for different kinds of clinical situations such as oncology patients,32,33 critically ill patients,34 or those with diverse cultural barriers.35
Training models of simulated physicians and patients have demonstrated their usefulness as a training method for personnel with very little experience.36,37
The use of information in printed format has also been verified,38 demonstrating its efficiency in cases where the patient has to make a decision with regard to treatment. Under these and other circumstances, the decisions may be influenced by adequate information received in pamphlet form. On the other hand, this measure can reduce the time used in the medical consultation to provide certain information about illnesses or specific topics of general importance.
This preliminary study should prompt new studies that will allow better definition of the information problem so as to be able to take advantage of the intent carried out in other countries as well as to implement new measures adapted to the individual case of each institution.
This study shows that communication between parents and pediatricians is limited. Poor understanding of the parents about the diagnosis, prognosis or treatment is worthy of further investigation including educational and patient-centered interventions aimed at improving the ability of pediatricians to communicate with both patients and parents. There is a high degree of misinformation among patients' relatives whose children are cared for at the Ambulatory Pediatrics Unit at the Hospital Infantil de México Federico Gómez. Contributing factors may be diverse, with the same consequences. Further research is necessary to explore in our environment the necessities of the population for medical communication. Implementation of new measures adapted to the individual case of each institution can contribute to improve the situation. This exploratory study may be the basis for new investigations that allow this process to be completed and to make decisions that contribute to improve the problem.
Practice implications
There are deficiencies in the physician/patient communication process that could be improved by regulating the information content. This could be useful, mainly in tertiary-care hospitals where many different physicians treat the same patients. Consequences of misinformation are diverse. Many attempts have been made to improve the complex process of physician/patient communication. This situation could also favor the creation of new educational programs at the university level to train residents, nurses, and students in this process.
Confidentiality statement
I confirm all patient/personal identifiers have been removed or disguised in order that patient/person(s) described are not identifiable and cannot be identified through details of this report.
References
1. Stricker KH, Kimberger O, Schmidlin K, Zwahlen M, Mohr U, Rothen HU. Family satisfaction in the intensive care unit: what makes the difference? Available at: http://www.ncbi.nlm.nih.gov/pubmed/19730813? Intensive Care Med 2009;35:2015-2017 [Epub ahead of print] [ Links ]
2. O'Regan C, Ryan M. Patient satisfaction with an emergency department psychiatric service. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19725372 Int J Health Care Qual Assur 2009;22:525-534. [ Links ]
3. Beckett MK, Elliott MN, Richardson A, Mangione-Smith R. Outpatient satisfaction: the role of nominal versus perceived communication. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19656231 Health Serv Res 2009;44(5 Pt 1):1735-1749. Epub. 2009:27. [ Links ]
4. Charlton CR, Dearing KS, Berry JA, Johnson MJ. Nurse practitioners' communication styles and their impact on patient outcomes: an integrated literature review. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18638178 J Am Acad Nurse Pract 2008;20:382-388. [ Links ]
5. Moguel PG, Serrano SA, Juárez N, Saucedo G. La satisfacción de los usuarios de la consulta externa del Hospital Infantil de México "Federico Gómez": Un parámetro importante para el entendimiento del tratamiento y la enfermedad de los niños. Cal Aten Sal 1996;3:12-17. [ Links ]
6. Underhill C, McKeown L. Getting a second opinion: health information and the Internet. Health Rep 2008;19:65-69. [ Links ]
7. Babbie ER. Prepruebas y estudios piloto. In: Babbie ER. Métodos de Investigación por Encuesta. México D.F.: Fondo de Cultura Económica; 1988: pp. 248-268. [ Links ]
8. Baena MI, Calleja MA, Romero JM, Vargas J, Zarzuelo A, Jiménez-Martín J, et al.The validation of a questionnaire for the identification of problems arising. Ars Pharmaceut 2001;42:147-169. [ Links ]
9. Chavez-Ayala R, Andrade-Palos P, Rivera-Rivera L. Validación de un cuestionario para la medicion de las creencias sobre el climaterio. Salud Publica Mex 2002;44:385-391. [ Links ]
10. Britten N. Qualitative interviews in medical research. BMJ 1995;311:251-253. [ Links ]
11. Arribas MC. Diseño y validación de cuestionarios. Matrona Profesion 2004;5:23-29. [ Links ]
12. Méndez RI, Namihira GD, Moreno AL, Sosa de Martínez C. Diseño estadístico. In: Mendez RI, et al. El Protocolo de Investigación. México: Ed Trillas; 1984. pp 11-27. [ Links ]
13. Pérez-Lázaro C, Iñíguez-Martínez C, Santos-Lasaosa S, Alberti-González O, Martínez-Martínez L, Tejero-Juste C, et al. Study into what the population knows about strokes and vascular risk factors. Rev Neurol. 2009;49:113-118. [ Links ]
14. Finkelstein FO, Story K, Firanek C, Barre P, Takano T, Soroka S, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int 2008;74:1178-1184. [ Links ]
15. Messes NG. Professional-patient relationships and informed consent. Postgrad Med 2004;80:277-283. [ Links ]
16. Lewis NJ, Bugdalski-Stutrud C, Abate MA, Blommel M, Wu CH, Gaither CA. The Medication Assessment Program: comprehensive medication assessments for persons taking multiple medications for chronic diseases. J Am Pharm Assoc (2003) 2008;48:171-180. [ Links ]
17. Nurit P, Bella BC, Gila E, Revital Z. Evaluation of a nursing intervention project to promote patient medication education. J Clin Nurs 2009;18:2530-2536. [ Links ]
18. Briten N, Stevenson AF, Barry AC, Barber N, Bradley CP. Misunderstanding in prescribing decisions in general practice: qualitative study. BMJ 2000;320:484-488. [ Links ]
19. Suhonen R, Nenonen H, Laukka A, Valimaki M. Patient's informational needs and information received do not correspond in hospital. J Clin Nurs 2005;14:1167-1176. [ Links ]
20. Zuaenepoel L, Hoorens V, Peuskens J, Laekeman G, UZA-Psychiatry Research Group. The "extent of information desired"-scale in psychiatric in-patients: a behavioral approach. Patient Educ Couns 2006;62:72-78. [ Links ]
21. Damghi N, Khoudri I, Oualili L, Abidi K, Madani N, Zeggwagh AA, et al. Measuring the satisfaction of intensive care unit patient families in Morocco: a regression tree analysis. Crit Care Med 2008;36:2084-2091. [ Links ]
22. Galassy JP, Chamber R, Ware WB. The patient reactions assessment: a brief measure of the quality of the patient-provider medical relationship. Psychol Assess 1992;4:346-351. [ Links ]
23. Suchman AL, Markakis K, Beckman H, Frankel R. A model of empathic communication in the medical interview. JAMA 1997;277:678-682. [ Links ]
24. O'Neill O. Some limits of informed consent. J Med Ethics 2003;29:4-7. [ Links ]
25. Fredericks S, Guruge S, Sidani S, Wan T. Patient demographics and learning needs: examination of relationship. Clin Nurs Res 2009;18:307-322. [ Links ]
26. Blumenthal D, Causino N, Chang YC, Culpepper L, Marder W, Saglam D, et al. The duration of ambulatory visits to physicians. J Fam Prac 1999;48:264-271. [ Links ]
27. Grassi, M. Patient information is often misleading (letters). BMJ 1999;319:786. [ Links ]
28. Wyatt J. Information to patients. JR Soc Med 2000;93:467-471. [ Links ]
29. Schilling LM, Scatena L, Steiner JF, Albertson GA, Lin CT, Cyran L, et al. The third person in the room: frequency, role, and influence of companions during primary care medical encounters. J Fam Pract 2002;51:685-686. [ Links ]
30. Walton MM, Elliott SL. Improving safety and quality: how can education help? Med J Aust 2006;184(10 Suppl):S60-S64. [ Links ]
31. Baerheim A, Hjortdahl P, Holen A, Anvik T, Fasmer OB, Grimstad H, et al. Curriculum factors influencing knowledge of communication skills among medical students. BMC Med Educ 2007;7:35. [ Links ]
32. Maidment IR. What is FACET? Eur J Cancer Care 2005;14:466-475. [ Links ]
33. Merkaert I, Libert Y, Razavi D. Communication skill training in cancer care: where are we and where are we going? Curr Opinion Oncol 2005;17:319-330. [ Links ]
34. Azoulay E, Pochard F, Moreau D, Fieux F, Thiery G, Le Gall JR, et al. Informing family members of critically ill patients. Clin Pulm Med 2002;9:330-334. [ Links ]
35. Carrillo EJ, Green AR, Betancourt RJ. Cross-cultural primary care: a patient based approach. Ann Int Med 1999;130:829-834. [ Links ]
36. Lorin S, Rho L, Wisniversky J, Nierman DM. Improving medical student intensive care unit communication skills: a novel educational initiative using standardized family members. Crit Care Med 2006;34:2386-2391. [ Links ]
37. Stevens A, Hernandez J, Johnsen K, Dickerson R, Raij A, Harrison C, et al. The use of virtual patients to teach medical students history taking and communication skills. Am J Surg 2006;19:806-811. [ Links ]
38. Roseman T, Joos S, Koerner T, Heiderhoff M, Laux G, Szecsenyi J. Use of a patient information leaflet to influence patient decisions regarding mode of administration of NSAID medications in case of acute low back pain. Eur Spine J 2006;15:1737-1741. [ Links ]














