Prosthetic valve thrombosis
Valve thrombosis is an always standing concern in prosthetic valves. Although it is an infrequent event (between 0.3 and 8% per patient/year), it holds considerable risks, for example, heart failure and embolic events, mainly brain infarcts, and also morbidity and mortality related to cardiac surgery1.
We present the case of a 62-year-old female with two previous surgeries at mitral valve, due to rheumatic heart disease. At presentation, she complained of progressive dyspnea, lower limb edema and fever. She was non-adherent to her anticoagulation regimen. Transthoracic echocardiography showed high prosthetic gradients (mean gradient 19 mm Hg) and velocities (V Max 319 cm/seg) (Fig. 1) suggesting stenosis through the valve. She was taken to transesophageal echo. It confirmed the stenosis and also showed blocking of the posterior tilting disk, multiple globular soft echo density masses in both tilting disks, and left atria. These findings confirm prosthetic valve thrombosis2. Then, she deteriorates into atrial fibrillation with rapid ventricular rate and is transferred to the intensive care unit. Heart team decided that she is not an optimal candidate for thrombolytic therapy due to high burden of thrombus in echo and risk of hemodynamic instability. She is taken to surgery; findings are abundant pannus and obstructive prosthetic valve thrombosis (Fig. 2). A #29 Medtronic Mosaic bioprosthetic valve is implanted (to avoid future need of anticoagulation) with no complications. Pathology study confirms previous findings, and specimen cultures are negative. During follow-up, she remains in good condition.
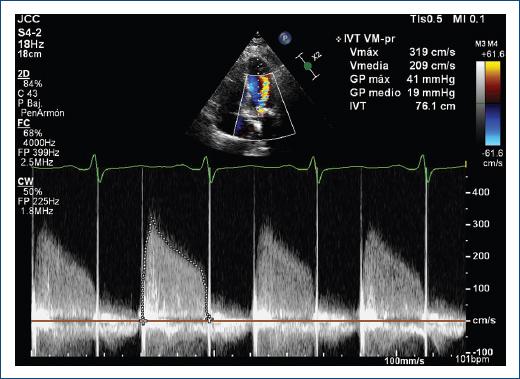
Figure 1 Continuous wave Doppler in mitral valve mechanical prosthesis, showing high transprosthetic flow velocities and gradients.
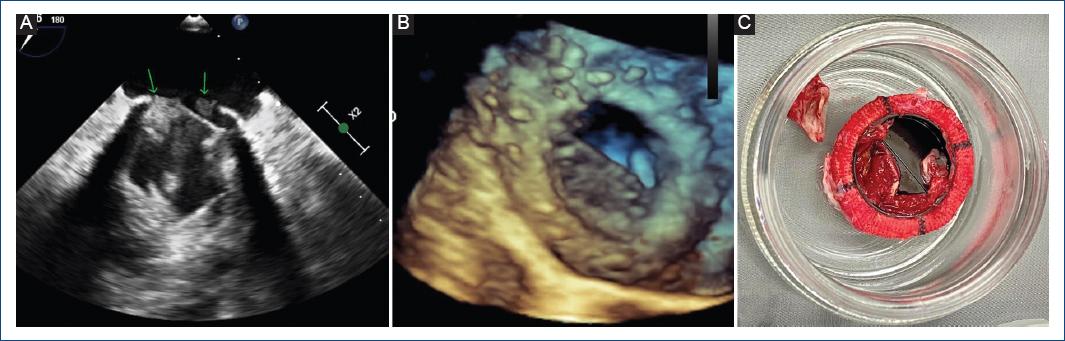
Figure 2 A: prosthetic valve thrombosis in 2D image (arrows). B: 3D rendering (transesophageal echocardiogram), and C: post-operative in vivo explanted valves showing prosthetic valve thrombosis.
This clinical case report highlights the important relationship between subtherapeutic anticoagulant regimen and prosthetic mechanical valve thrombosis (PVT). Definitive diagnosis is made with clinical criteria (acute onset of dyspnea and pulmonary edema) and cardiac imaging (echocardiography shows: high velocities and gradients and reduced or no disk opening) or histopathology (thrombus in surgical specimen). Surgery in left PVT is warranted in large thrombus (> 0.8 cm2) NYHA class III-IV, left atrial thrombus, and pannus1. In lack of these criteria, slow infusion thrombolysis and echocardiographic follow-up is recommended.
Conclusion
Prosthetic valve thrombosis diagnosis is initially suspected on a clinical scenario, then supported by cardiac imaging, it occasionally needs surgery, to confirm diagnosis, and treat the cause2.











 nueva página del texto (beta)
nueva página del texto (beta)


