Introduction
ST-segment elevation myocardial infarction (STEMI) needs prompt diagnosis and reperfusion treatment to reduce infarct size, improve outcomes, and reduce mortality. Reperfusion therapy must be administered in all patients with STEMI presenting within 12 h of symptom onset1. Nevertheless, the demonstrated benefit of reperfusion therapy, a significant proportion of STEMI, does not receive this therapy and only a small fraction is initially considered ineligible. The failure to provide reperfusion therapy includes late arrival, uncertain admission diagnosis, early ST resolution2, and health system infrastructure-related deficiencies, mainly in low-to-middle-income countries3.
The absence of reperfusion therapy in STEMI has been associated with more complications and with poorer in-hospital and long-term outcomes4,5. However, few studies have assessed predictors of in-hospital mortality in patients with STEMI who did not receive reperfusion therapy. Therefore, our aim of this study was to analyze the differences in survivors and non-survivors with non-reperfused STEMI and to identify the predictors of in-hospital mortality.
Materials and methods
This was a retrospective cohort study from October 2005 to August 2020 of patients admitted to the Coronary Care Unit of the National Institute of Cardiology in Mexico City with non-reperfused STEMI. We recorded baseline demographic data, history, clinical characteristics, laboratory test, coronary angiographic results, and in-hospital outcomes. Patients with STEMI were identified based on clinical characteristics, electrocardiographic changes, and biochemical markers of cardiac necrosis (isoenzyme of creatinine kinase, creatinine phosphokinase, or troponin I), according to the standard definitions of the European Society of Cardiology and American College of Cardiology6.
Patients with non-reperfused STEMI were categorized into survivors and non-survivors, and we identified the causes of the lack of reperfusion therapy. The authors obtained informed consent from the patients referred in the article.
Statistical analysis
All continuous variables were analyzed for distribution with Kolmogorov-Smirnov’s test. Continuous variables were reported as mean and standard deviation or median and interquartile range. Categorical variables were reported as frequencies and percentages. Statistical differences between groups were assessed, either using the Chi-square or Fisher’s exact tests, for categorical variables, and Student’s t test or Mann-Whitney U-test, for continuous variables.
Cox regression analyses with stepwise selection were performed to adjust for factors associated with in-hospital mortality. The covariates included in the multivariate analysis were those associated with in-hospital mortality in the univariate analyses. These included all demographic characteristics, medical history, and clinical features at presentation that had p < 0.05, as well as those previously recognized as established predictive factors. Odds ratios (ORs) with 95% confidence intervals were calculated for variables in both univariate and multivariate analyses. Statistically significant differences were assumed when p < 0.05. SPSS software version 13 (Chicago, IL, USA) was used for statistical analyses.
Results
From 23,493 patients admitted to the coronary care unit, 6663 had STEMI as their initial diagnosis. Among these patients, 4221 (36.7%) were ineligible because they received reperfusion therapy and 2442 were non-reperfused STEMI (Fig. 1). Mortality among reperfused STEMI was 7.2% and 12.7% in non-reperfused STEMI (log-rank p = 0.000) (Fig. 2).
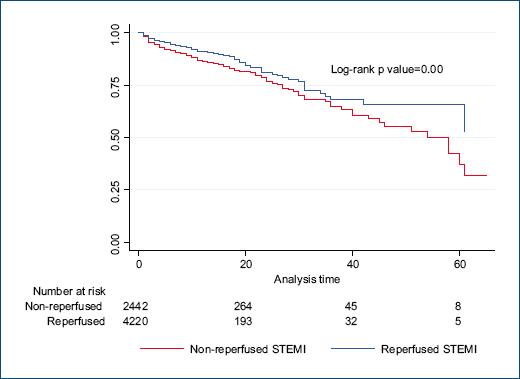
Figure 2 Kaplan–Meier analysis showing survival among reperfused and non-reperfused ST-elevation myocardial infarction.
The main reasons for non-reperfusion were delayed presentation (96.1%) followed for uncontrolled comorbidities (cancer, dementia, heart failure, and renal failure) (2.3%) and recent surgery or trauma (0.5%). (Table 1).
Table 1 Reasons for non-reperfused STEMI
| Variables | n | % |
|---|---|---|
| Delayed presentation (≥ 12 h) | 2346 | 96.1 |
| Uncontrolled comorbidities | 55 | 2.3 |
| Recent surgery or trauma | 13 | 0.5 |
| Active bleeding | 10 | 0.4 |
| Misdiagnosis | 8 | 0.3 |
| Use of anticoagulants | 5 | 0.2 |
| Coagulation disorders | 3 | 0.1 |
| Uncontrolled hypertension | 1 | 0.05 |
| Cerebrovascular event < 1 year | 1 | 0.05 |
We analyzed the patients according to survival, and from 2442 patients, 311 (12.7%) died during hospitalization. Non-survivors compared with survivors were more often older, women, with history of diabetes, hypertension, and atrial fibrillation. At presentation, non-survivors were more likely to have high-risk features, including lower systolic blood pressure, higher heart rate, worse Killip-Kimball class, lower left ventricular ejection fraction, higher blood glucose levels, higher NT-proBNP, and renal dysfunction (Table 2).
Table 2 Clinical characteristics and laboratory tests in non-reperfused STEMI
| Variable | Total (n = 2442) | Survivors (n = 2111) | Non-survivors (n = 311) | p |
|---|---|---|---|---|
| Age (years) | ||||
| Median (IQR) | 60 (53-69) | 60 (53-68) | 66 (58-74) | 0.00 |
| Body mass index (kg/m2) | ||||
| Median (IQR) | 26.8 (24.6-29.4) | 26.9 (24.7-29.4) | 26.5 (24-29) | 0.07 |
| Men, n (%) | 1966 (80.5) | 1726 (81.8) | 240 (72.5) | 0.00 |
| Women, n (%) | 476 (19.5) | 385 (18.2) | 91 (27.5) | |
| Diabetes, n (%) | 1092 (44.7) | 894 (42.3) | 198 (59.8) | 0.00 |
| Current smoking, n (%) | 791 (32.4) | 698 (33.1) | 93 (28.1) | 0.07 |
| Previous smoking, n (%) | 714 (29.2) | 619 (29.3) | 95 (28.7) | 0.84 |
| Hypertension, n (%) | 1207 (49.4) | 1016 (48.1) | 191 (57.7) | 0.00 |
| Dyslipidemia, n (%) | 720 (29.5) | 628 (29.7) | 92 (27.8) | 0.51 |
| Prior myocardial infarction, n (%) | 295 (12.1) | 247 (11.7) | 48 (14.5) | 0.14 |
| Prior PCI, n (%) | 131 (5.4) | 109 (5.2) | 22 (6.6) | 0.29 |
| Prior CABG, n (%) | 28 (1.1) | 25 (1.2) | 3 (0.9) | 1 |
| Previous stroke, n (%) | 60 (2.5) | 52 (2.5) | 8 (2.4) | 1 |
| Atrial fibrillation, n (%) | 33 (1.4) | 22 (1) | 11 (3.3) | 0.00 |
| Heart failure, n (%) | 119 (4.9) | 96 (4.5) | 23 (6.9) | 0.07 |
| Previous treatment with acetylsalicylic acid, n (%) | 484 (19.8) | 413 (19.6) | 71 (21.5) | 0.41 |
| Previous treatment with statin, n (%) | 333 (13.6) | 288 (13.6) | 45 (13.6) | 1 |
| Systolic blood pressure (mmHg) | ||||
| Median (IQR) | 120 (110-140) | 124 (110-140) | 106 (90-120) | 0.00 |
| Heart rate (lpm) | ||||
| Median (IQR) | 80 (70-95) | 80 (70-92) | 88 (69-102) | 0.00 |
| Delay to treatment (hh:mm) | ||||
| Median (IQR) | 42:00 (19:30-85:32) | 42:00 (19:42-87:49) | 40:43 (18:00-77:34) | 0.06 |
| Killip-Kimball n (%) | ||||
| I | 1204 (49.3) | 1139 (54) | 65 (19.6) | 0.00 |
| >II | 1238 (50.7) | 972 (46) | 266 (80.4) | |
| Infarction location n (%) | ||||
| Anterior | 1227 (50.2) | 1049 (49.7) | 178 (53.8) | 0.17 |
| Non-anterior | 1215 (49.8) | 1062 (50.3) | 153 (46.2) | |
| Left bundle branch block, n (%) | 79 (3.2) | 60 (2.8) | 19 (5.7) | 0.01 |
| Right bundle branch block, n (%) | 142 (5.8) | 107 (5.1) | 35 (10.6) | 0.00 |
| NT-proBNP at admission (pg/ml) | ||||
| Median (IQR) | 2764 (971-6705) | 2340 (900-5331) | 9451 (4604-22257) | 0.00 |
| Glucose at admission (mg/dl) | ||||
| Median (IQR) | 136 (109-208) | 132 (108-194) | 184 (130-285) | 0.00 |
| Troponin at admission (pg/ml) | ||||
| Median (IQR) | 15.7 (4.6-41) | 15 (4.3-37.5) | 23.4 (5.8-61.2) | 0.00 |
| CK-total | ||||
| Median (IQR) | 522 (190-1364) | 501 (185-1301) | 675 (228-1763) | 0.00 |
| CK-MB | ||||
| Median (IQR) | 24.5 (5.7-94) | 22.83 (5.3-90.7) | 32.3 (8.1-124.5) | 0.00 |
| Hemoglobin (g/L) | ||||
| Median (IQR) | 14.4 (12.9-15.7) | 14.6 (13-15.8) | 13.8 (12-15.) | 0.00 |
| Platelets (103/mL) | ||||
| Median (IQR) | 219 (180-265) | 220 (182-266) | 211 (165-260) | 0.00 |
| Leukocytes (103/mL) | ||||
| Median (IQR) | 10.83 (8.5-13.5) | 10.6 (8.4-13.1) | 12.4 (9.8-15.7) | 0.00 |
| Na (mEq/L) | ||||
| Median (IQR) | 136 (134-139) | 136 (134-139) | 136 (132-138) | 0.00 |
| K (mEq/L) | ||||
| Median (IQR) | 4.2 (3.9-4.5) | 4.1 (3.9-4.5) | 4.5 (3.9-5) | 0.00 |
| Albumin (g/dL) | ||||
| Median (IQR) | 3.6 (3.2-3.9) | 3.6 (3.3-3.9) | 3.3 (3-3.6) | 0.00 |
| Total cholesterol (md/dL) | ||||
| Median (IQR) | 155 (127-185) | 156 (128-186) | 143 (118-176) | 0.00 |
| HDL (mg/dL) | ||||
| Median (IQR) | 34.7 (28.6-41.5) | 35 (29-41.6) | 33 (25-41.3) | 0.00 |
| LDL (mg/dL) | ||||
| Median (IQR) | 95 (72-120) | 96 (73.4-121.6) | 83.5 (63-111) | 0.00 |
| Triglycerides (mg/dL) | ||||
| Median (IQR) | 135 (104-175) | 136 (105-176) | 131 (94-166) | 0.03 |
| C reactive protein (mg/dL) | ||||
| Median (IQR) | 33 (10.6-107) | 29.9 (10-99.4) | 62.1 (23.4-161.2) | 0.00 |
| Creatinine (mg/dL) | ||||
| Median (IQR) | 1 (0.8-1.36) | 1 (0.8-1.2) | 1.6 (1-2.5) | 0.00 |
| Glomerular filtration rate (ml/min) | ||||
| Median (IQR) | 75.25 (49.45-75.25) | 79.46 (55.47-103.29) | 40.93 (25.93-68.68) | 0.00 |
| Ejection fraction (%) | ||||
| Median (IQR) | 45 (37-54) | 48 (40-55) | 35 (26-45) | 0.00 |
IQR: interquartile range, PCI: percutaneous coronary intervention, CABG: coronary artery by-pass graft.
Regarding treatment, there were differences among survivors and non-survivors in the proportion of antithrombotic and anticoagulant therapy. Besides, non-survivors were significantly less likely to receive beta-blockers and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers but were significantly more likely to receive intravenous diuretics (Table 3).
Table 3 Medical treatment in non-reperfused STEMI
| Variable | Total, n (%) (n = 2442) | Survivors, n (%) (n = 2111) | Non-survivors, n (%) (n = 311) | p-value |
|---|---|---|---|---|
| Acetylsalicylic acid | 2401 (98.3) | 2084 (98.7) | 317 (95.8) | 0.00 |
| P2Y12 inhibitor | 1506 (61.7) | 1319 (62.5) | 187 (56.5) | 0.03 |
| Heparin | 1482 (60.7) | 1235 (58.5) | 247 (74.6) | 0.00 |
| Enoxaparin | 882 (36.1) | 818 (38.7) | 64 (19.3) | 0.00 |
| Tirofiban | 58 (2.4) | 51 (2.4) | 7 (2.1) | 0.73 |
| ACE inhibitor/ARB | 2032 (83.2) | 1893 (89.7) | 139 (42) | 0.00 |
| β-blockers | 1332 (54.5) | 1279 (60.6) | 53 (16) | 0.00 |
| Statins | 2270 (93) | 1979 (93.7) | 291 (87.9) | 0.00 |
| Spironolactone | 318 (13) | 296 (14) | 22 (6.6) | 0.00 |
| Intravenous nitrate | 804 (32.9) | 714 (33.8) | 90 (27.2) | 0.01 |
| Intravenous diuretics | 1247 (51.1) | 1026 (48.6) | 221 (66.8) | 0.00 |
| Oral diuretics | 130 (5.3) | 126 (6) | 4 (1.2) | 0.00 |
ACE: angiotensin-converting enzyme, ARB: angiotensin receptor blocker.
The left main coronary artery disease as well as three-vessel disease was more common in non-survivors (8.7% vs. 5%, p = 0.03, and 41% vs. 26% p = 0.00, respectively).
Non-survivors were significantly less likely to undergo coronary angiography, percutaneous coronary intervention, and had more coronary artery bypass graft, Swan-Ganz catheter, intra-aortic balloon pump, hemodialysis, mechanical ventilation, and temporary pacemaker when compared with survivors. Besides, in-hospital heart failure, reinfarction, advanced atrioventricular block, atrial fibrillation, bleeding, and stroke occurred more frequently in non-survivors (Table 4).
Table 4 Invasive procedures and clinical outcomes in non-reperfused STEMI
| Variable | Total, n (%) (n = 2442) | Survivors, n (%) (n = 2111) | Non-survivors, n (%) (n = 311) | p-value |
|---|---|---|---|---|
| Angiography | 1747 (71.5) | 1564 (74.1) | 183 (55.3) | 0.00 |
| PCI | 979 (47.5) | 886 (50) | 93 (32.5) | 0.00 |
| CABG | 82 (3.5) | 54 (2.6) | 31 (9.4) | 0.00 |
| Swan-Ganz catheter | 102 (4.2) | 43 (2) | 59 (17.8) | 0.00 |
| IABP | 144 (5.9) | 55 (2.6) | 89 (26.9) | 0.00 |
| Hemodialysis | 42 (1.7) | 17 (0.8) | 25 (7.6) | 0.00 |
| Mechanical ventilation | 217 (8.9) | 55 (2.6) | 162 (48.9) | 0.00 |
| Temporary pacemaker | 198 (8.1) | 120 (5.7) | 78 (23.6) | 0.00 |
| In-hospital heart failure | 63 (2.6) | 40 (1.9) | 23 (6.9) | 0.00 |
| Acute pulmonary edema | 65 (2.7) | 29 (1.4) | 36 (10.9) | 0.00 |
| Cardiogenic shock after admission | 79 (3.2) | 13 (0.6) | 66 (19.9) | 0.00 |
| Recurrent angina | 71 (2.9) | 57 (2.7) | 14 (4.2) | 0.12 |
| Reinfarction | 41 (1.7) | 16 (0.8) | 25 (7.6) | 0.00 |
| Advanced atrioventricular block | 87 (3.6) | 51 (2.4) | 36 (10.9) | 0.00 |
| Atrial fibrillation | 91 (3.7) | 71 (3.4) | 20 (6) | 0.01 |
| Major bleeding | 32 (1.3) | 17 (0.8) | 15 (4.5) | 0.00 |
| Minor bleeding | 32 (1.3) | 21 (1) | 11 (3.3) | 0.00 |
| Stroke | 26 (1.1) | 14 (0.7) | 12 (3.6) | 0.00 |
PCI: percutaneous coronary intervention, CABG: coronary artery by-pass graft; IABP: intra-aortic balloon pump.
Finally, we performed a Cox regression model for the prediction of in-hospital mortality, in which we found that the main factors associated with this outcome were: Age > 65 years, systolic blood pressure < 100 mmHg, Killip-Kimball ≥ II, right bundle branch block, glucose > 180 mg/dL, decreased glomerular filtration rate, left ventricular ejection fraction < 40%, and absence of coronary angiography (Table 5).
Table 5 Cox regression analysis for mortality prediction in non-reperfused STEMI
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% confidence interval | p-value | Hazard ratio | 95% confidence interval | p-value | |
| Gender (male) | 1.48 | 1.16-1.89 | 0.001 | |||
| Age ( ≥ 65 years) | 2.25 | 1.81-2.80 | 0.000 | 1.38 | 1.07-1.78 | 0.013 |
| Diabetes | 1.73 | 1.39-2.16 | 0.000 | |||
| Hypertension | 1.30 | 1.04-1.62 | 0.017 | |||
| Previous atrial fibrillation | 3.06 | 1.67-5.59 | 0.000 | |||
| Systolic blood pressure < 100 mmHg | 0.97 | 0.97-0.98 | 0.000 | 2.26 | 1.75-2.91 | 0.000 |
| Heart rate > 100 bpm | 1.00 | 1.00-1.01 | 0.056 | |||
| Killip-Kimball ≥ II | 3.58 | 2.72-4.70 | 0.000 | 1.71 | 1.22-2.40 | 0.002 |
| Left bundle branch block | 1.79 | 1.12-2.85 | 0.014 | |||
| Right bundle branch block | 1.72 | 1.21-2.45 | 0.002 | 1.68 | 1.16-2.43 | 0.006 |
| Glucose ≥ 180 mg/dL | 2.06 | 1.66-2.56 | 0.000 | 1.45 | 1.14-1.86 | 0.002 |
| Creatinine depuration 30-59 mL/min | 3.59 | 2.75-4.69 | 0.000 | 2.10 | 1.55-2.84 | 0.000 |
| Creatinine depuration < 30 mL/min | 7.09 | 5.35-9.38 | 0.000 | 3.41 | 2.42-4.80 | 0.000 |
| Left ventricle ejection fraction < 40% | 3.26 | 2.52-4.21 | 0.000 | 1.97 | 1.48-2.61 | 0.000 |
| Anterior myocardial infarction | 0.84 | 0.68-1.04 | 0.127 | |||
| Left main coronary disease | 0.87 | 0.52-1.44 | 0.600 | |||
| Absence of coronary angiography | 0.52 | 0.41-0.65 | 0.000 | 1.45 | 1.13-1.87 | 0.003 |
Discussion
In our study, we found a great proportion of non-reperfused STEMI, mainly due to delayed presentation to hospital services, which was associated with adverse outcomes and increased mortality. The main predictors of in-hospital mortality were age, low systolic blood pressure, right bundle branch block, high blood glucose, decreased glomerular filtration rate, and left ventricular ejection fraction.
A non-reperfused STEMI mainly occurs in patients who present to medical attention beyond 12 h of symptom onset; this 12 h cutoff point was set based on studies that demonstrated no benefit and increased bleeding risk of thrombolysis in late presenters. In many studies around the world, the proportion of non-reperfused STEMI has been calculated as low as 8.5% to as high as 40% and the main reasons for the absence of reperfusion have been: age > 75 years, prior heart failure of myocardial infarction, prior stroke, active bleeding, traumatic cardiopulmonary resuscitation, use of anticoagulants, and suspicion of acute aortic syndrome7. We must highlight that our study has lower STEMI mortality than the reported for Mexico because our center has all the tools for evaluation, treatment, and prompt reperfusion.
The most recent recommendations from the European Society of Cardiology state the importance of the reduction in the delay of the first medical contact and STEMI diagnosis, which should be < 10 min. Besides, medical systems must be logistically prepared to give treatment – thrombolysis or PCI – in the first 12 h and ideally in the first 2 h of symptom onset8. Even though the great amount of evidence and recommendations, reperfusion strategies are not always given to all patients because of multiple logistic, social, and economic reasons, and as an example, in Mexico, the proportion of non-reperfused STEMI has been estimated to be of 44%3. The main recommendations for non-reperfused STEMI, according to the newest available guidelines, state the following: (1) PCI should be done if the patient has recurrent symptoms, hemodynamic instability or life-threatening arrhythmias, (2) if the patient presents between 12 and 48 h of symptom onset PCI should be routinely done, and (3) PCI should not be attempted if the infarct-related artery has been occluded for more than 48 h8.
One of the main benefits of reperfusion therapy has been the reduction of mechanical complications in STEMI patients, which now are as low as 1.5%1,9,10. Nevertheless, globally, nearly 17-36.8% of all STEMI do not receive reperfusion treatment2,11,12. In our study, this percentage is higher, mainly because of the difficulties for getting rapid medical attention in one of the most crowded cities of the world and because of the fragmentation of the medical services. Furthermore, the first medical contact delay is very important in Mexico not only due to logistical issues but mainly because of a lack of education regarding the importance of attending promptly to medical services after symptom onset.
In this study, we found a wide variety of reasons for no reperfusion, being the most important the presence of uncontrolled comorbidities, mistakes in the diagnosis, and active bleeding. The CRUSADE quality improvement initiative studied 8578 patients and found that 10.3% had a documented contraindication for reperfusion therapy and 7.2%, that were eligible for reperfusion, received no reperfusion attempt. Similar to our analysis, we have to state that in the last group, the main reasons for not attempting reperfusion were older age, heart failure at presentation, presentation at a non-cardiac surgical center, prior stroke, and female sex. Furthermore, not all reasons are medically taken because of a clinical condition, besides in many opportunities, the family or the patient refuses treatment by means of no resuscitation orders, mainly due to severely decompensated comorbidities11,12.
In our study, the main reason for not attempting reperfusion therapy was the delay beyond 12 h from symptom onset and the arrival to medical attention, which is an indicator that the patient does not have enough information to attend promptly to medical services. This issue is of great importance, as it is an opportunity for the Mexican Public Health Administration to use the communication media to spread more information regarding STEMI and the importance of getting a fast to medical attention, especially in people with risk factors.
Mortality among non-reperfused STEMI has been reported to be 11.7–14.4%, which is similar to what we found in Mexican population. Furthermore, it has also been calculated that being ineligible for reperfusion has an OR for mortality of 3.85. The highest mortality rates have been reported in patients with reperfusion contraindication (OR 1.77) and in eligible patients in which no reperfusion treatment was attempted (OR 1.64)2,11,12.
Regarding gender issues, we found that women have a lower frequency of non-reperfused STEMI, nevertheless, they have higher mortality than men. There could be multiple explanations to these facts, but mainly it can be due to longer life expectancy and concomitant appearance of comorbidities that predispose to STEMI.
In our analysis, we found a similar proportion of anterior and non-anterior STEMI. It has been established that anterior STEMI caused by proximal occlusion of the left descending coronary artery have worse prognosis because it irrigates a large myocardial territory and is more prone to cause ventricular dysfunction and remodeling. In other studies, it has been found that 36% of STEMI are caused by the left anterior descending occlusion, which contrasts with our findings of 50%. This is relevant because outcomes such as reinfarction, hospitalization for heart failure, and death are more frequent with occlusion of this artery and must be monitored in the follow-up13.
The right bundle branch block can indicate a proximal left anterior descending artery occlusion; nevertheless, this electrocardiographic factor has been relegated because the left bundle branch block is thought to have a worse prognosis. In our study, we found that patients presenting with the right bundle block had worse survival if they had no reperfusion therapy.
Primary outcomes after a non-reperfused STEMI are straightly related to the baseline characteristics of each patient. It has been described that the main predictors for death, reinfarction, and heart failure were: Previous history of heart failure (HR 2.06), peripheral vascular disease (HR: 1.93), diabetes (HR: 1.49), rales (HR: 1.88), low ejection fraction (HR: 1.48 for each 10%), and low filtration rate (HR: 1.11 for each 10 ml/min)14. These risk factors are similar with the ones we reported in our study, nevertheless for us, the most important were: Killip-Kimball ≥ II, diminished glomerular filtration rate, low systolic blood pressure, right bundle branch block, low left ventricular ejection fraction, and absence of coronary angiography.
Reperfusion networks are needed to improve short- and long-term outcomes in STEMI, mainly in low-to-middle-income countries15. With the creation and implementation of these networks, non-reperfused STEMI should diminish in the near future to overcome the great public health burden, such as heart failure and disability-adjusted life years. Finally, we must highlight that gender in STEMI has been an inconclusive as women have been underrepresented. In our study, we found that women have high mortality rates comparable to other studies16, therefore, we must look forward to do more research to improve outcomes in this population.
The main limitations of our study are that, even though our hospital is a national referral center, it is a single-center experience, so data cannot be extrapolated to the whole population. Besides, data were obtained from a clinical registry from the coronary unit that was not created specifically for acute coronary syndromes and thus some variables are missing.
Conclusion
In patients with non-reperfused STEMI, mortality and adverse outcomes occur more frequently. Non-survivors with STEMI were more likely to be older, female, with diabetes and hypertension, and developed more frequently heart failure, reinfarction, atrioventricular block, bleeding, and stroke. The main predictors for in-hospital mortality were: Renal dysfunction, systolic blood pressure < 100 mmHg, and left ventricle ejection fraction < 40%. There is a lack of contemporary reperfusion treatments in low-to-middle-income countries and this lag must be surmounted with policies that make readily available these therapies to every person with STEMI.











 nueva página del texto (beta)
nueva página del texto (beta)



