We present a case of a 34-year-old female with Hypertrophic Cardiomyopathy (HCM) without family history of HCM or sudden cardiac death, diagnosed 13 years earlier with a mutation in TNNC1 gene (ALA8VAL substitution, encoding troponin C protein). Usually she was at class II of New York Heart Association (NYHA) functional class; she was medicated with 20 mg of bisoprolol and 200 mg of disopyramide. Her last transthoracic echocardiography (TTE) showed a severe asymmetric left ventricle hypertrophy (LVH), a left ventricle outflow tract (LVOT) obstruction with peak pressure gradient of approximately 80 mmHg at rest, and a moderate to severe mitral regurgitation (MR) due to systolic anterior motion (SAM) of anterior mitral valve leaflet. After counseling with her cardiologist and obstetrician, she decided to get pregnant. Disopyramide was withdrawn and it was decided to augment dose of bisoprolol to 30 mg/day to control LVOT obstruction. The first and second trimesters of pregnancy were uneventful. At 30 weeks of gestation, she presented de novo fetal growth restriction (2.5th centile) and vasodilation of middle cerebral artery (<5th centile); the dose of bisoprolol was diminished to 15 mg/day and the patient was admitted to nursery to supervise pregnancy. At the hospital, the patient maintained hemodynamic and echocardiographic stability without new fetal complications. At 33 weeks of gestation, she was medicated with dexamethasone for fetal lung maturation. One week later, due to sustained deterioration of fetal, placental growth, and fetal cerebral flow, the patient was transferred to a tertiary center with capability to cardiac mechanical support. TTE was repeated and exhibited a severe asymmetric LVH (maximum left ventricle wall thickness of 29 mm at level of basal septum), a LVOT obstruction with peak pressure gradient of approximately 90 mmHg at rest, moderate MR due to SAM of anterior mitral valve leaflet, and preserved biventricular systolic function (Fig. 1 and supplementary data). Intravascular fluid administration was started to avoid hypovolemia. One day after admission in the tertiary center, because of pathologic fetal cardiotocography, an emergent caesarean section was performed at 34 weeks and 4 days of gestation. The patient delivered a female newborn with 1,470 g; Apgar score at 1, 5 and 10 min of 8, 9 and 9, respectively. The patient presented a good clinical evolution, without maternal or neonate complications and was discharged 5 days after delivery medicated with 20 mg of bisoprolol per day.
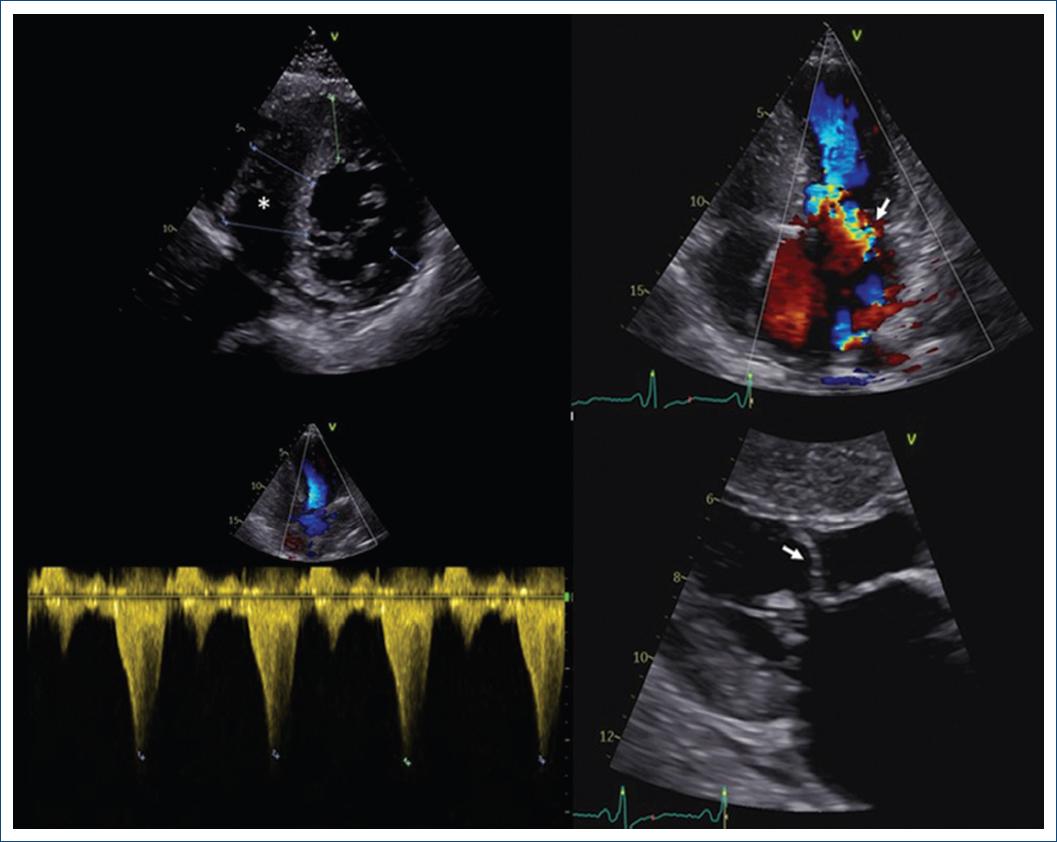
Figure 1 Transthoracic echocardiogram performed at 34 weeks of gestation showing a
preserved biventricular systolic function with severe asymmetric LVH presenting
a maximum LV wall thickness of 29 mm at level of basal septum (*, upper left
panel), a severe left ventricle outflow tract obstruction with peak pressure
gradient of approximately 90 mmHg at rest (lower left panel) and a moderate
mitral regurgitation ( , upper right panel) due to
systolic anterior motion of anterior mitral valve leaflet (
, upper right panel) due to
systolic anterior motion of anterior mitral valve leaflet ( , lower right planet).
, lower right planet).
One year after discharge, the patient is in NYHA class II with no cardiovascular events or hospitalizations. Her son started long-term follow-up in cardiology clinic and TTE performed at 2 months after birth exhibited a structurally normal heart.
Discussion
HCM is a frequent genetically determined heart muscle disease characterized by LVH that is not solely explained by abnormal loading conditions. LVH can be general or local, frequently asymmetric and located in the LVOT. The widespread use of echocardiography has led to a growing number of young women diagnosed with HCM planning to conceive1. In a normal pregnancy cardiac output increase 40-50%; this effect is due to increased stroke volume during first and second trimesters and due to increased heart rate during third trimester2. The increase of plasma volume is also an important change during pregnancy, which leads to physiological anemia thanks to hemodilution; other hemodynamic modification is hypercoagulability and a reduction in systemic vascular resistance3. Despite the increased risk of premature birth and the occurrence of symptoms in up to 48% of pregnant women with HCM, pregnancy is usually well tolerated4. The maternal mortality rate in these patients is 0.5% and the fetal mortality is comparable to the general population2. This good tolerance, at least in part, is due to the increase of plasma volume during pregnancy, which may reduce the LVOT gradient. In addition, hypovolemia is poorly tolerated, so special attention should be taken to blood loss and to hypovolemia caused by anesthetics during delivery2. Follow-up frequency during pregnancy depends on the risk assessment of HCM. Most women with HCM can be evaluated clinically and by TTE each trimester. As in the presented case, patients with high-risk profile defined by symptomatic HCM pre-pregnancy, diastolic dysfunction, history of arrhythmia, or CARPREG or ZAHARA score ≥ 1 should have a more strict follow-up, at least monthly, since they are at higher risk of complications during pregnancy3. Although severe LVOT obstruction has been classically considered a risk factor, recent reports from ROPAC registry showed no difference in adverse outcomes in these patients1. Justification for advising against pregnancy (WHO Class IV) in HCM is only present in a small minority of women with significant left ventricle (LV) dysfunction or severe symptomatic LVOT obstruction4. Concerning drug withdrawal before pregnancy, beta blockers are considered safe during pregnancy and should be continued if already used before pregnancy2. Beta-1-selective drugs are preferred and, as we saw in this report, careful should be taken with side effects such as fetal growth restriction, bradycardia, and hypoglycemia4. In general, antiarrhythmic medications should be avoided if possible during the first trimester. Disopyramide, despite being a category C drug from the former FDA classification, should only be used when potential benefits outweigh risks because it is related to some relevant adverse effects, namely, uterine contraction and placental abruption4,5. Low-risk cases may have a spontaneous labor and vaginal delivery, but cesarean section should be considered in patients with severe LVOT obstruction, pre-term labor while on oral anticoagulation or severe HF2.
Conclusions
This case highlights that pregnancy in patients with HCM is generally well tolerated, even in those with significative LVOT obstruction. Hypovolemia should be avoided, especially during labor and delivery. Follow-up frequency during pregnancy depends on the risk assessment of HCM and beta blockers are considered safe and should be continued if already used before pregnancy.











 text new page (beta)
text new page (beta)


