Introduction
Chronic thromboembolic pulmonary hypertension is a rare yet underdiagnosed pulmonary vascular disease, which is a sequela of pulmonary thromboembolism1 and corresponds to Group 4 of the classification of the World Health Organization2.
Although many of the patients who survive a pulmonary embolism present improvement overtime with resolution of the thrombotic load, there is a small group that develops chronic thromboembolic pulmonary hypertension3 due to a different natural history where resolution is limited, with organization and recanalization of the thrombus1. This is associated with changes in the small pulmonary arteries, which generates an increase in vascular resistance and pulmonary hypertension4.
From the epidemiological point of view, there are conflicting data regarding incidence and prevalence. However, recent reviews of hospital databases and clinical studies show that pulmonary hypertension occurs in 3.8-4% of patients who survive a pulmonary thromboembolism event3,5,6. With the above, an incidence of 3-5 cases per 100,000 cases in the United States and Europe can be estimated, with less than one-third of the cases being diagnosed3. Increased pressure and pulmonary vascular resistance (PVR) can lead to the development of the right heart failure and premature mortality7.
In selected patients with disease that is susceptible to surgical management, this is the treatment of choice, given the high probability of cure that such management achieves. Data from the different surgical groups show that patients present immediate and sustained improvement in pulmonary hemodynamics. The studies are consistent in the different series with improvement in PVR from values >800 dyn.s.cm−5 to less than 400 dyn.s.cm−5 8-10. Overtime, not only a decrease in pulmonary resistance has been noted but also an improvement in functional class demonstrated by walking for 6 min11. Data from Italy have shown similar results with sustained improvement in functional class in 97% of patients who were in the WHO functional Class III and IV before the procedure and reaching functional Class I in 74% at 4 years12.
The objective of this study was to analyze the clinical, hemodynamic results, and the risk factors for mortality in a cardiovascular referral center in Colombia.
Materials and Methods
A retrospective cohort study was conducted between January 2001 and November 2019 of patients undergoing pulmonary thromboendarterectomy in a cardiovascular care referral center. The patients were chosen for the procedure according to a multidisciplinary evaluation with the intervention of cardiovascular surgeons, cardiologists, specialists in heart failure, and pulmonologists from the pulmonary hypertension clinic, taking into account: functional class, accessibility of thrombotic lesions, hemodynamic status, and comorbidities. The pre-surgical evaluation including a detailed medical evaluation, with collection of clinical-demographic data, imaging studies (chest computed tomography, ventilation perfusion scan, echocardiography, and 6 min walk), and hemodynamic study. During the index hospitalization, data related to the surgical procedure and its complications, including mortality, were collected. Patient follow-up was carried out through visits between 1 and 6 months after the procedure, with clinical evaluation, echocardiography, catheterization (at the discretion of the treating physician), and a 6 min walk. Subsequent follow-ups were carried out depending on the clinical condition of the patient, as well as aspects related to their health insurance system. A telephone contact was made with the patients for the present work to obtain data on the clinical condition as variables of interest until November 2019.
The data included in the analysis were demographic, clinical, hemodynamic (pre-surgical, postsurgical, and follow-up), echocardiographic variables, as well as the characteristics related to the procedure.
Primary outcome: mortality at 30 days and 6 months. Secondary outcomes: change in hemodynamics during follow-up; echocardiographic change in follow-up; complications of the procedure. It was defined to carry out an analysis of mortality before and after the year 2015, year during which pulmonary hypertension group received training at the University of San Diego.
Continuous variables are presented as mean with standard deviation (DS) or as median and interquartile range (IQR) according to their distribution. For the analysis of the change in clinical, echocardiographic, and hemodynamic parameters, the Wilcoxon test was used for non-parametric continuous variables and the Chi-square test for categorical measures, p ≤ 0.05 was considered statistically significant. A multivariate logistic regression analysis of COX was performed to establish factors associated with mortality. The survival curve was calculated using the Kaplan–Meier method, applying the log-rank test to assess differences. All analyzes were carried out using the SPSS version 22.0 statistical program.
The present study was approved by the Institutional Ethics Committee and the Universidad Pontificia Bolivariana.
Results
Over an 18-year period, 73 patients underwent pulmonary thromboendarterectomy. The median age was 51 years, 55% of the patients were women. About 93% of the population had a history of pulmonary thromboembolism and 32% a history of thrombophilia, with antiphospholipid syndrome the most important condition (23%). The most frequent presenting symptoms were dyspnea and fatigue; 20% presented syncopal episodes, with a time between the onset of symptoms and their diagnosis of 12 months. The majority of the patients had marked symptoms, 79% being in functional Class III and IV (Table 1). The initial echocardiogram showed right ventricular dilation in 63%, with a median pulmonary artery pressure of 79 mmHg, tricuspid annular plane systolic excursion (TAPSE) of 16, and a quarter of the population had moderate-to-severe tricuspid regurgitation (Table 1 supplementary appendix). The mean pressure of the pulmonary artery was 50 mmHg in the right catheterization, with PVR of 640 dyn.s.cm−5 and systemic resistance of 1600 dyn.s.cm−5. About 46.5% of the population received specific treatment for pulmonary hypertension, sildenafil (n: 25; 34.2%), and bosentan (n: 11; 15%) being the most frequently used (14 in combination therapy and of these 6 received the sildenafil-bosentan combination). A little more than half were in anticoagulation management (60%), half were taking warfarin, and the remaining were direct anticoagulants (rivaroxaban and apixaban the most frequent). Before the procedure, two-thirds of the population received an inferior vena cava filter implant (Table 1).
Table 1 Baseline and surgical characteristics of the population
| Demographic and anthropometric | |
| Age, years [IQR] | 51 [39-61] |
| Male, n (%) | 33 (45) |
| BMI [IQR] | 24.6 [22.05-27.15] |
| Medical record | |
| Pulmonary embolism, n (%) | 68 (93) |
| Thrombophilia, n (%) | 23 (32) |
| Collagen disease, n (%) | 12 (16) |
| Symptoms | |
| Dyspnea, n (%) | 72 (99) |
| Fatigue, n (%) | 70 (96) |
| Edema, n (%) | 29 (40) |
| Chest pain, n (%) | 30 (41) |
| Hemoptysis, n (%) | 4 (6) |
| Syncope, n (%) | 14 (19) |
| Initial WHO functional class, n (%) | |
| – I | 0 (0) |
| – II | 15 (21) |
| – III | 44 (60) |
| – IV | 14 (19) |
| Symptom time at diagnosis, months [IQR] | 12 [6-48] |
| Diagnostic time to surgery, months [IQR] | 12 [4-48] |
| Symptom time to surgery, months [IQR] | 24 [8-64] |
| Pre-operative | |
| Anticoagulation, n (%) | 45 (60.8%) |
| – Warfarin | 24 (32.4%) |
| – Rivaroxaban | 11 (14.8) |
| – Apixaban | 9 (12.1%) |
| – Dabigatran | 1 |
| Inferior vena cava filter, n (%) | 50 (69) |
| Perfusion time, minutes [IQR] | 292 [244-326] |
| Aortic clamp time, minutes [IQR] | 120 [96-142] |
| Circulatory arrest time, minutes [IQR] | 64 [42-75] |
| Additional surgeries, n (%) | 17 (23.2%) |
| – Tricuspid plasty | 7 (41.1%) |
| – ASD closure | 4 (23.5%) |
| – Pulmonary artery plasty | 2 (11.7%) |
| – Coronary artery bypass graft surgery | 2 (11.7%) |
| Intraoperative complications, n (%) | 8 (10.9%) |
| – Vascular injuries | 7 (87.5%) |
| – Bronchial injuries | 1 (12.5%) |
| Mechanical ventilation time, days [IQR] | 2 [1-6] |
| Reperfusion edema, n (%) | 31 (43) |
| Post-operative vasoactive support | |
| – Dobutamine, n (%) | 39 (53) |
| – Norepinephrine, n (%) | 32 (43) |
| – Nitric oxide, n (%) | 25 (34) |
| – Vasopressin, n (%) | 5 (6.8) |
| – Milrinone, n (%) | 21 (29) |
| – Levosimendan, n (%) | 4 (6) |
| – Nitroprusside, n (%) | 3 (4) |
| Hospital stay | |
| – ICU, days [IQR] | 6 [3-13] |
| – Hospitalization, days [IQR] | 20 [14-29] |
Regarding of the surgical procedure, the median perfusion time was 292 min, the aortic clamp time was 120 min, and the circulatory arrest time was 64 min. Additional procedures were performed in 17 patients (23%), with tricuspid plasty and the correction of an atrial septal defect being the most frequent. Complications related to the procedure occurred in a minority of cases (10%), of which vascular lesions were the main ones; no patient died during the procedure (Table 1).
Half of the patients required inotropic support (n: 39; 53%) after the procedure and in a lesser percentage vasopressor support (n: 32; 43%). About 43% of the patients had reperfusion edema. The stay in the intensive care unit was 6 days, with a median of 2 days of mechanical ventilation and a total time of hospitalization of 20 days (Table 1).
When analyzing the echocardiographic behavior (Table 1 supplementary appendix), there are three moments in which the patients were evaluated: pre-surgery, immediately after the procedure during hospitalization and in outpatient follow-up. The parameters that showed variation were the diastolic diameter of the right ventricle, which decreased from 4.7 cm to 4.1 cm and finally 3.6 cm (p ≤ 0.001). Of 63 patients with right ventricular dilation in the initial study, only 21 patients continued with dilatation criteria in follow-up; something similar was noted in the systolic pressure of the pulmonary artery, which decreased from 76 mmHg to 45 mmHg after surgery, statistically significant change (p ≤ 0.001) and to 43 mmHg in the last available study. However, only 46 patients (63% of the total population) had an echocardiogram at follow-up, and of these 25 patients had pressures> 40 mmHg, which corresponds to 54%. The TAPSE showed a decrease in the immediate post-operative period to return to its initial value in the follow-up (16 mm; p = 0.002). Of the 18 patients with moderate-to-severe tricuspid regurgitation, only three remained with this criterion in the postsurgical echocardiogram and five in the outpatient echocardiogram (p = 0.004). No other significant changes were noted at the echocardiographic level.
Regarding the hemodynamic parameters (Table 2) after the surgical intervention, there was a significant decrease in parameters such as pulmonary artery systolic pressure (change of 46%; p = 0.008), mean pulmonary artery pressure (change of 40%; p ≤ 0.001), pulmonary artery diastolic pressure (43.8% change; p ≤ 0.001), systemic vascular resistance (SVR) (42.8% change; p ≤ 0.005), and PVR (79% change; p = 0.357); the cardiac index also increased (24% increase; p = 0.003). Only 22 patients had right catheterization during follow-up, since only those who remained symptomatic or had functional impairment were subjected to this study. Mean pulmonary pressures > 25 mmHg were found in 16 patients in this group, of which only seven had values >40 mmHg. When analyzing PVR, 13 had > 240 dyn.s.cm−5 (equivalent to> 3 Wood units), 4 had values > 500 dyn.s.cm−5 (equivalent to> 6.2 Wood units), and only 1 presented a value dyn.s.cm−5 (equivalent to > 12 Wood units). With these data, 21% of the patients had invasive evidence of residual pulmonary hypertension.
Table 2 Hemodynamic variables
| Parameter | Initial, (n = 72*) | Post-operative, (n = 68*) | Follow-up, (n = 22) | p |
|---|---|---|---|---|
| RAP mmHg | 10 [6-16] | 8 [4-10] | 6 [3-8] | 0.29 |
| PASP mmHg | 87 [80-100] | 47 [36-57] | 43 [32-53] | 0.008 |
| PADP mmHg | 32 [25-39] | 18 [15-23] | 18 [12-21] | < 0.001 |
| mPAP mmHg | 50 [44-59] | 30 [22-35] | 33 [27-40] | < 0.001 |
| PVR dyn.seg.cm-5 | 640 [12-876] | 136 [94-305] | 352 [186-473] | 0.357 |
| SVR dyn.seg.cm-5 | 1600 [1264-1865] | 916 [694-1161] | 1452 [955-1689] | 0.005 |
| Wedge mmHg | 13 [9-16] | 14 [12-28] | 11 [7-14] | 0.14 |
| CI, L/min/m2 | 2.4 [2.0-2.7] | 3.2 [2.6-3.7] | 3.2 [2.8-3.2] | 0.003 |
*Variables presented as median [IQR]. P value obtained from the Wilcoxon test for non-parametric continuous variables and X2 for categorical variables. PASP: pulmonary artery diastolic pressure; PADP: pulmonary artery systolic pressure; mPAP: mean pulmonary artery pressure; RAP: right atrial pressure; CI: cardiac index; SVR: systemic vascular resistance; PVR: pulmonary vascular resistance.
At discharge, 20.5% of the patients continued with the specific treatment for pulmonary hypertension, with sildenafil monotherapy being the strategy most used in these patients.
In the 6-month follow-up, there were four hospitalizations: two for cardiovascular causes (heart failure) and two non-cardiovascular (abdominal pain and infection of the surgical site).
The change in the clinical condition of the patients was evaluated by functional class and walking at 6 min at 6 and 12 months (data presented in Table 3). The baseline functional class of the patients was III and IV in 79% of the population; at 6 months, only 7% were in functional Class III and one patient reported a functional Class IV; 54% of the patients reported functional Class I and II. At 6 months, the patients increased their 6 min walk by 15% (approximately 70 m), something that was statistically significant (p = 0.04)
Table 3 Clinical variables
| Variable n (%) | Initial, (n = 72*) | 6 months, (n = 45*) | 12 months, (n = 25) | p |
|---|---|---|---|---|
| Class functional | 0.34 | |||
| I | 0 (0) | 23 (32) | 19 (26) | |
| II | 15 (21) | 16 (22) | 2 (3) | |
| III | 44 (60) | 5 (7) | 4 (6) | |
| IV | 14 (19) | 1 (1) | 0 (0) | |
| 6 min walk distance, mts [IQR] | 407 [321-493] | 475 [420-565] | 432 [366-484] | 0.04 |
*Variables presented as n (%) or median [IQR]. P value obtained from the Wilcoxon test for non-parametric continuous variables and Chi-square X2 for categorical variables.
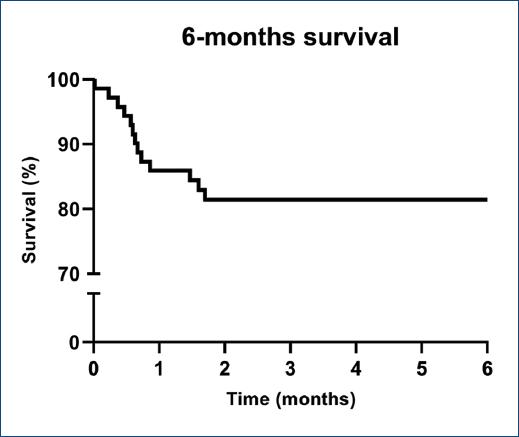
Regarding mortality, there were 14 events (19.17%) in the study period (Fig. 1 and table 4). Most of these (n: 9; 12.32%) occurred at 30 days (Fig. 2), septic shock being the main cause followed by cardiogenic etiology. The deaths during the first 6 months were 5; of these three dues to pulmonary infectious complications and in two of these events, the cause could not be established. An analysis was performed in two periods: between 2001 and 2014 and 2015 until 2019. In the first period, 18 procedures were performed with 6 deaths (33%). In the second period, 55 procedures were performed with eight deaths for a mortality rate of 14.54% with a tendency to a better result in patients operated in survival at 6 months, however, without differences statistically neither at 30 days nor at 6 months (Fig. 3).
Table 4 Aspects related to mortality
| Deaths n (%) | 14 (19.17%) |
|---|---|
| 30-day mortality, n (%) | 9 (12.32%) |
| Septic shock | 6 |
| Ventilator-associated pneumonia | 3 |
| Nosocomial pneumonia | 1 |
| Intestinal necrosis | 1 |
| Cardiogenic shock | 3 |
| Mortality at 6 months, n (%) | 5 (6.85%) |
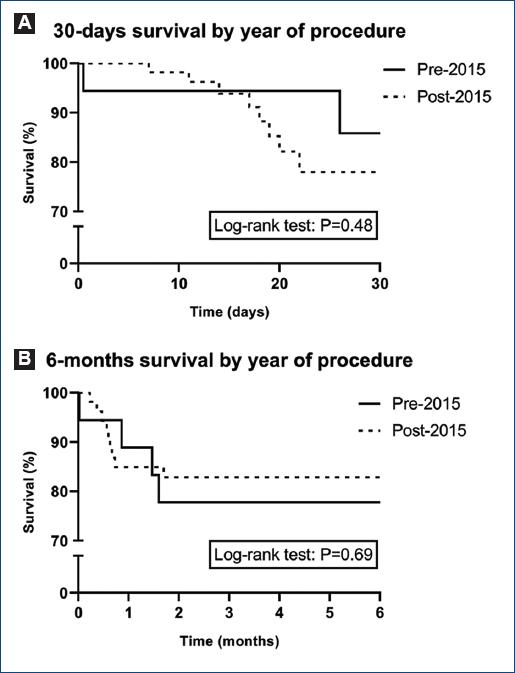
Figure 3 Survival curve of stratified patients before and after 2015. A: 30-day survival. B: 6-month survival. The difference between curves was evaluated by the log-rank test.
To establish the risk factors for mortality in our population, a multivariate logistic regression analysis of COX was performed. Demographic, clinical, surgical, and echocardiographic hemodynamic parameters were included (Table 2 supplementary appendix). The factors found associated with mortality were the diastolic diameter of the right ventricle measured postoperatively (hazard ratio [HR] 10.88 95% confidence interval [CI] 1.97-62, p = 0.007), time of invasive mechanical ventilation (HR 1.06 95% CI 1.02-1.09, p = 0.004), and the presence of complications during the surgical procedure (HR 5.62 95% CI 1.94-16.22, p = 0.001). None of the other variables included in the model presented a significant association. An exploratory analysis of survival was performed using the Kaplan–Meier method at both 30 days and 6 months for PVR and surgical times. No differences were found according to PVR, nevertheless, it clear that visually, there seems to be a trend toward better survival in patients with PVR <1000 dyn.s.cm−-5 (Figure 1 of the supplementary appendix) and neither according to the surgical times (Figures 2, 3, and 4 of the supplementary appendix).
Discussion
Although the exact prevalence of chronic thromboembolic pulmonary hypertension is unknown, it is believed that 4-5% of patients who present with an episode of pulmonary embolism develop it. Pulmonary thromboendarterectomy remains the management strategy of choice in patients with pulmonary hypertension associated with chronic thromboembolic disease due to the results, it has shown in recent years (low mortality rate, complications, and high possibility of cure)13.
This study presents the clinical and hemodynamic results associated with the surgical management of thromboembolic pulmonary hypertension over a period of 18 years; previous reports in Colombia have included a small number of patients14.
Regarding the baseline characteristics of the population, these accord with those of the group of patients published by two of the largest registries in the United States15 and Europe8. The history of thrombophilia is in a medium range in relation to the different series, coinciding with the antiphospholipid syndrome being the main alteration16,17. Most of the patients (79%) presented severe and limiting symptoms measured in their baseline functional class (III and IV) something that is also similar to those documented in large centers8,15. An important and higher proportion than that reported presented chest pain in our population8,18. The time from the onset of symptoms to diagnosis is similar to that reported (12 months), not being the case for the times from diagnosis to surgery (78 days vs. 12 months) and from the onset of symptoms to the surgical procedure (24 months vs. 17 months)8,15,16, surely something related to the Colombian health-care system. The stay in the intensive care unit was shorter than that reported (6 vs. 14) with similar days of mechanical ventilation (2 on average)8,15. Among the complications after the procedure, a higher frequency of reperfusion edema was found compared to other studies8,16 (43% vs. 9.6-20%), something that did not increase the need for ventilatory support or stay in the unit intensive care, nor was it a risk factor for mortality in the population.
Regarding the technical aspects of the procedure, the median time of perfusion as for aortic clamp was like the data of large series8,15, not being the case for the time of circulatory arrest, since in our series is double that reported (35 min for the California University in San Diego and the European vs. record 64 min in our cohort). Although this parameter has been related to transient neurological dysfunction, memory alterations, and focal motor deficits in some studies19,20, these abnormalities were not found in the population studied. Complications occurred during surgery in eight patients, most of them arterial injuries, but none died as a cause of these; this parameter was one of the risk factors for death found, something that can be explained by an indirect relationship since these patients required a longer time of ventilatory support and stay in the intensive care unit, which increases the possibility of nosocomial or care-related infections, the main cause of death in the present study.
The hemodynamic and follow-up data found were similar to those reported worldwide with a remarkable improvement immediately after surgery, which in the long term translates into an improvement in dyspnea parameterized by functional class as well as an increase in the 6 min walk distance8,10,15,21,22 and the echocardiographic parameters (right ventricular diameter, significant tricuspid regurgitation), reinforcing the benefit of surgical management. The rate of residual pulmonary hypertension (21%) was similar to that reported by the San Diego group (16%).
The reported in-hospital mortality varies worldwide from 4.4 to 16%8,10,15 and is related to aspects such as the experience of the surgical group. In the California University in San Diego, mortality for the first 200 procedures was 17%, which decreased to 8.8% in the next 500 patients in 4 years, reaching the current reported rate of 2.2%15. Global mortality was 19.17% and in-hospital at 20 days 12.32%, what agrees with the aforementioned. In the analyzes carried out for the 2 time periods, in the first 18 procedures, mortality was 30% (2001-2014), decreasing to 14.54% in the following 55 interventions (2015-2019), something that reinforces the observations of improvement in mortality with the increase in the number of patients, procedures, and the experience of the surgical group. The main cause of death was infectious complications, which again denotes the safety of the intervention.
The risk factors for mortality in our population were the diameter of the right ventricle after surgery, the time of mechanical ventilation, and the presence of complications; these last findings are surely related to the fact that the main cause of death was septic shock, due to ventilator-associated pneumonia. No relationship or association was found with parameters related to higher mortality previously described, such as PVR before the procedure, the 6 min walk distance, and the functional class of the patients8,15,23.
The present study has several limitations: the first is that the retrospective nature allows that biases cannot be completely ruled out during the study process. They are data from a single center. Patient follow-up by the medical group was low, with few data from studies such as echocardiography, 6 min walk distance, paraclinical tests such as natriuretic peptides, and right catheterization at 12 months. However, due to the health insurance model in Colombia, it is something that researchers cannot control.
Conclusions
Pulmonary thromboendarterectomy is the medical management of choice in patients with pulmonary hypertension in Group 4, due to the clinical and hemodynamic results and its safety.
In our population, the results obtained in a center with high volume and cardiovascular complexity was similar to those reported worldwide, with mortality that is decreasing as the number of cases increased. This should be considered the first treatment option in candidate patients in our setting.
Supplementary Data
Supplementary data are available at Archivos de Cardiología de México online (https://www.archivoscardiologia.com). These data are provided by the corresponding author and published online for the benefit of the reader. The contents of supplementary data are the sole responsibility of the authors.











 nueva página del texto (beta)
nueva página del texto (beta)