Introduction
Heart failure with preserved ejection fraction (HFpEF) is increasingly prevalent due to population aging and the growth of risk factors such as obesity. It is a challenging diagnosis and has been based on the findings of the resting echocardiogram1,2. The problem is that a significant number of patients only have symptoms during physical activity; thus, only analyzing diastolic function at rest may not be sufficient to identify this group of patients3-5. Many studies have suggested the usefulness of diastolic stress test for showing diastolic function alterations with exercise6-8.
At the same time, a clinical score has been developed to identify patients with HFpEF: the H2FPEF9. This score confirms HFpEF with high scores or rules it out with low scores. However, intermediate scores require additional studies to confirm or rule out the diagnosis.
The objective of this study is to determine the association between diastolic dysfunction after exercise, clinical variables, and H2FPEF score in a population of patients referred for exercise stress test at a Colombian reference center.
Methods
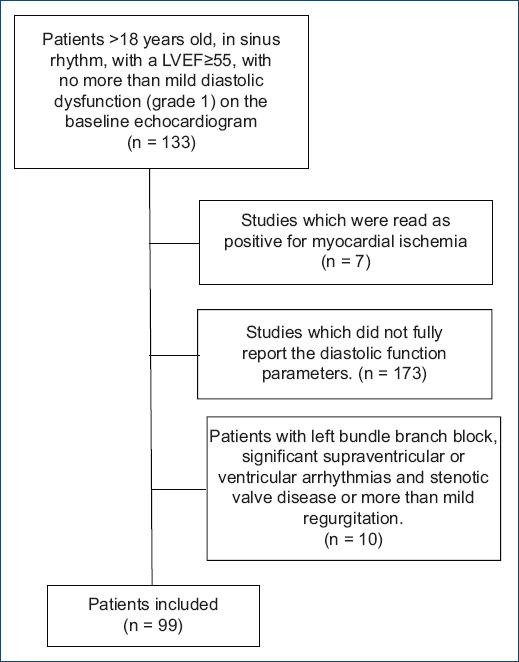
The researchers retrospectively analyzed exercise stress test performed between January 2018 and December 2019 which had been ordered due to dyspnea or fatigue, from which images were extracted to evaluate diastolic function as well as contractility parameters.
A convenience sample was taken and patients who met the eligibility criteria were included in the study.
Inclusion criteria
Patients over the age of 18, in sinus rhythm, with a left ventricular ejection fraction (LVEF) equal to or > 55%, with no more than mild diastolic dysfunction (grade 1) on the baseline echocardiogram, according to guidelines of the American Society of Echocardiography and the European Association of Cardiovascular Imaging10, were included in the study.
Exclusion criteria
Studies which were read as positive for myocardial ischemia were discarded, as well as those which did not fully report the diastolic function parameters. Patients with atrial fibrillation, significant mitral valve disease; at least moderate mitral annular calcification, any mitral stenosis or mitral regurgitation of more than moderate severity, mitral valve repair or prosthetic mitral valve, LV assist devices, left bundle branch block, and ventricular paced rhythms10, were excluded from the study.
Resting echocardiogram
A conventional resting echocardiogram was performed according to the American Society of Echocardiography’s recommendations11. The LVEF was evaluated using the modified Simpson’s method measured from the apical four-chamber view; the left ventricular filling pressure was calculated by the ratio of early mitral inflow velocity to early diastolic mitral annular tissue velocity (E/e´); and pulmonary artery systolic pressure (PASP) was evaluated by the peak velocity of the tricuspid regurgitant jet, using Bernoulli´s equation, plus the estimated right atrial pressure.
Post-exercise echocardiography stress protocol
Patients were evaluated using the Bruce protocol immediately after exercising on a treadmill, measuring the tricuspid regurgitant velocity before the 1st min and the E/e´ ratio once mitral wave separation was observed. A septal E/e´ ratio equal to or > 15 was used to establish the presence of post-exercise diastolic dysfunction, accord of the most recent guideline of stress echocardiography12-14. The H2FPEF score was calculated for all patients and an association was sought with the diastolic stress test results.
Statistical analysis
Categorical variables were summarized in absolute and relative frequencies. The normal distribution of continuous variables was evaluated with the Kolmogorov–Smirnov test. They were normally distributed and therefore were expressed as mean ± standard deviation (SD). For the bivariate analysis, the dependent variable was the result of the diastolic test (positive/negative); Pearson’s Chi-square test was used to measure the association with the categorical independent variables and Student’s t-test was performed for quantitative independent variables. Chi-square was used to determine the association between the H2FPEF score and the diastolic test results. Demographic and clinical data processing was performed using the SPSS® version 21.0 statistical package.
The study was conducted according to the rules of the Declaration of Helsinki and was approved by relevant ethical committees and/or regulatory bodies in participating hospitals. All patients gave written informed consent to participate, in accordance with national and local regulations.
Results
A total of 99 patients who met the eligibility criteria were included for data analysis (Fig. 1), the average age of the population was 62.2 years (SD 12.3), 49.5% were women. Altogether, 58.6% had a history of arterial hypertension, 12.1% had diabetes mellitus, and 20.2% had a prior diagnosis of coronary disease (Table 1).
Table 1 Clinical and echocardiographic characteristics of the study population, by diastolic stress test results
| Negative DST (n (%) = 36) | Positive DST (n (%) = 63) | p-value | |
|---|---|---|---|
| Males | 34 (54.0%) | 16 (44.4%) | 0,4* |
| Age (year, DS) | 58.5 (± 11.74) | 68.1 (± 10.5) | < 0.01+ |
| BMI (DS) | 25.7(± 3.1) | 26.2 (± 3.6) | 0.55+ |
| BMI > 30 | 7 (11.1%) | 6 (16.7%) | 0.54* |
| Hypertension | 30 (47.6%) | 28 (77.8%) | 0.01* |
| Paroxysmal AF | 5 (7.9%) | 1 (2.8%) | 0.41* |
| DM | 5 (7.9%) | 7(19.4%) | 0.11* |
| Coronary disease | 8 (12.7%) | 12 (33.3%) | 0.19* |
| Dyslipidemia | 20 (31.7%) | 20 (55.6%) | 0.33* |
| LVEF% (DS) | 59.9 (± 2.1) | 58.8 (± 4.4) | 0.57+ |
| Baseline TRV mt/s (DS) | 2.3 (± 0.18) | 2.5 (± 0.2) | < 0.01+ |
| PASP mmHg (DS) | 30.5 (± 3.5) | 34.3 (± 4.1) | < 0.01+ |
| Baseline E/e (DS) | 9.3 (± 1.7) | 10.3 (± 1.4) | < 0.01+ |
| Post-exercise TRV mt/seg (DS) | 2.6 (± 0.2) | 3.2 (± 0.3) | < 0.01+ |
| Post-exercise E/e’ cm/seg (DS) | 9.6 (± 2.2) | 17.8 (± 2.6) | < 0.01+ |
| Mets reached | 9.8 (± 1.8) | 8.4 (± 2.4) | < 0.01+ |
*Pearson’s Chi-square.
+Student’s t.
DET: diastolic stress test; SD: standard deviation BMI: body mass index; AF: atrial fibrillation; DM: diabetes mellitus; LVEF: left ventricular ejection fraction; TRV: tricuspid regurgitation velocity; PASP: pulmonary artery systolic pressure; Mets: metabolic equivalent of task.
The following echocardiographic parameters were obtained: LVEF 59.7% (SD 3.1); resting septal e´ 7.5 cm/s (SD 1.1) and post-exercise septal e´ 7.3 cm/s (SD 1.8); resting tricuspid regurgitant velocity 2, 4 mt/s (SD 21.0) with 2.8 mt/s (SD 37.0) post-exercise; and resting E/e´ 9.7 cm/s (SD 1.6) with 12.6 cm/s (SD 4.6) after exercise.
Regarding to the terms included in the H2FPEF score, 13.1% of patients had a body mass index > 30, 58.6% of patients with hypertension were treated with 2 or more medications, 6.1% had a history of paroxysmal atrial fibrillation, 27.3% had pulmonary hypertension, 56.5% were older than 65 years, and 63.6% had an E/e´> 9 (Table 2).
Table 2 Positivity of the H2FPEF items by diastolic stress test results
| Clinical variable | Definition | Patients with a positive parameter | ||
|---|---|---|---|---|
| Negative DST n = 6) | Positive DST(n = 36) | |||
| H | Heavy | BMI > 30 kg/mt2 | 14 (22%) | 13 (36%) |
| Hypertension | Treatment with ≥ 2 antihypertensives | 20 (32%) | 13 (36%) | |
| F | Atrial fibrillation | Paroxysmal or persistent | 5 (8%) | 1 (3%) |
| P | Pulmonary hypertension | PSAP > 35 mmHg | 9 (14%) | 17 (47%) |
| E | Elderly | > 60 years | 27 (42.8%) | 28 (77%) |
| F | Elevated filling pressures | E/e´> 9 | 39 (62%) | 23 (64%) |
| H2FPEF score | 1.8 (sd 1.3) | 3.2 (sd 1.3) | ||
DST: diastolic stress test.
The average H2FPEF score was 2.3 (SD 1.4): 27.2% of the patients had a low H2FPEF score (0-1), 71.7% an intermediate score (2-5), and 1% a high score (≥ 6). About 12.5% of the patients with a low H2FPEF score had a positive stress test for diastolic dysfunction, in the intermediate range, the positivity was 45%.
The stress test was positive for diastolic dysfunction in 36.4% of the patients.
A statistically significant association was found between the H2FPEF score and the diastolic stress test (p = 0.02) (Table 3).
Table 3 Association of the total H2FPEF score and the diastolic stress test result
| H2FPEF score (n = 99) | H2FPEF score | Positive DST (n = 36) | Negative DST (n = 63) | Association |
|---|---|---|---|---|
| Low 0-1 (n = 27) | 0 | 1 (2.8%) | 13 (20.6%) | p = 0.02* |
| 1 | 2 (5.6%) | 11 (17.5%) | ||
| Intermediate 2-5 (n = 71) | 2 | 12 (33.3%) | 21 (33.3%) | |
| 3 | 9 (25.0%) | 9 (14.3%) | ||
| 4 | 7 (19.4%) | 8 (12.7%) | ||
| 5 | 4 (11.1%) | 1 (1.6%) | ||
| High ≥ 6 (n = 1) | 6 | 1 (2.8%) | 0 |
*Pearson’s Chi-square test. DST: diastolic stress test.
The use of the post-exercise tricuspid regurgitant velocity more than 3,4 mt/s as a parameter for the diagnosis of diastolic dysfunction was present in only one patient without E/e´ > 15 and in 10 patients with E/e > 15, all of these patients were classified as intermediate probability of having the disease according to the H2FPEF score.
Discussion
This study found a high frequency of diastolic dysfunction diagnosed by stress test in a population of symptomatic patients with a medium to high probability of having the disease according to the H2FPEF score. These data are congruent with the prevalence reports of the disease, which have increased over the past decades; HFpEF constitutes up to 56% of all heart failure cases15. Despite the high prevalence of the disease, the ideal strategy for diagnosing it is still unclear, and thus, it is important to use other tools such as the exercise stress test and scores like H2FPEF. Some of the diagnostic difficulties have been the existence of multiple predisposing phenotypes such as diabetes, obesity, or kidney disease16,17, along with the fact that, unlike patients with heart failure with reduced ejection fraction, in these patients, biomarkers such as natriuretic peptides may be within normal limits or only slightly elevated18.
This study found a high prevalence of a history of coronary disease with post-exercise diastolic dysfunction, it may have resulted from a selection bias in the referral for the exercise test. It has been reported relatively recently that the development of diastolic dysfunction during stress studies could, theoretically, be an early marker of myocardial ischemia and allow an earlier diagnosis of coronary disease19,20. Furthermore, Gimelli study, using nuclear medicine, suggests that post-stress diastolic function testing could help identify patients with non-obstructive coronary disease21.
Evaluation of the variables used for the H2FPEF score showed that, in general, they were more frequently positive in the population with a positive diastolic dysfunction stress test, except for age and atrial fibrillation. However, approximately 70% of the patients had intermediate scores which require further testing to be able to determine the presence or absence of HFpEF. Furthermore, there were patients with low scores and a positive test. The clinical characteristics of patients with HFpEF vary among population groups and the discrimination capacity of the clinical scores may also vary according to the population to which they are applied. It would be important to validate these scores in our population.
Although atrial fibrillation has been documented as a marker of diastolic dysfunction22,23, in this study, this disease was more frequently found in the group of patients with normal diastolic function in response to exercise (1% vs. 5%). This could be due to the sample size and to the fact that the stress test was not performed on patients who had fibrillation at the time of the study, which constitutes a selection bias. Diastolic dysfunction increases with age; however, the lack of age-adjusted and standardized references may lead to overestimating its importance in the development of HFpEF24.
Elevated baseline filling pressures, defined as E/e´> 9, were found in a high percentage of patients in both groups, although they were more prevalent in those with a positive diastolic dysfunction test. The E/e´ ratio increases with age, from 7.8 at 35 years to 10.9 in individuals at or above the age of 7525. Antonello study found that 48% of healthy individuals between the ages of 55 and 64 had an E/e´ ratio > 10, and in patients between 65 and 74 years old, this percentage increased to 63% of asymptomatic patients, suggesting that the cutoff points for this population should be modified26. In our study, we found a total of 55 patients over the age of 60, 67% of whom had an E/e´ ratio ≥ 10; the average E/e´ ratio was 10.1, with no significant differences between those with post-exercise diastolic dysfunction and those without (10.2 and 10.0, respectively).
The tricuspid regurgitation velocity is usually used in the assessment of diastolic function, although its normal values at rest are well standardized, the same does not happen with the values during exercise, the European guide suggests values for the diagnosis of diastolic dysfunction > 3.4 mt/s14, while some authors such as Belyavsiy suggest a cutoff point of > 2.8 mt/s27. In our work, with the cutoff point of > 3.4 mt/s, only one patient was found who did not meet the criteria of presenting an E/e´ > 15, and this had a low pre-test probability. In addition, this parameter is the one with the lowest reproducibility with an intraoperative correlation of 65%, for which we decided not to use it in our work as a diagnostic criterion for diastolic dysfunction28.
Limitations
This study’s limitation includes its retrospective nature, the small sample size, and the NT pro-BNP or BNP levels which were not available. The elevated filling pressure findings were not validated by invasive measurements, which are the gold standard. This study’s finding should be validated through prospective studies with a larger sample.











 nueva página del texto (beta)
nueva página del texto (beta)