Introduction
Infective endocarditis (IE) has an annual incidence of 3-9 cases/100,000. Multiple studies suggest auxiliary diagnoses tests for early and timely diagnosis to decrease morbidity1-3. Despite medical progress in surgical procedures and medical treatments, IE is a disease that has a high mortality (30-80%)4-7. Surgical procedures may reduce significantly composite morbidity and mortality in hospital complications8,9.
According to the American College of Cardiology and European Society of Cardiology guidelines, the criteria for a surgical procedure on endocarditis of the left heart valve are: cardiac events (heart failure, moderate or severe regurgitation, abscess, and dehiscence or perforation), embolization prevention (vegetation greater than 10 mm with embolization to the central nervous system and/or great mobility, and vegetation greater than 15 mm) and uncontrolled infection (persistent fever or positive blood cultures after 5 days with medical treatment, infection due to fungi or multi-resistant bacteria)1-3,10-13. Indications for right heart valve vegetation include: microorganisms (fungi or failure to eradicate them), vegetation greater than 20 mm with recurrent pulmonary embolism, or right heart failure due to tricuspid regurgitation with a poor response to medical treatment14. Surgery is suggested in the first 4-week period, but patients with these criteria having unstable hemodynamic state or hemorrhagic vascular event a 4-week delay of the surgical procedure is recommended15. We compared the risk factors associated to mortality of patients with or without surgery. Our primary outcome was mortality within 6 months of follow-up after the diagnosis.
Materials and methods
We conducted a retrospective cohort study in patients diagnosed with IE at our Institution, from January 2001 to September 2016. Patients were evaluated if they were treated with either a surgery or medical treatment. The study protocol was accepted by the Institutional Ethics Committee. We designed the study according to the principles of the Helsinki Declaration.
Patient selection
Patients older than 15 years with a definitive diagnosis of IE according to the Duke’s Criteria were included; (1) all included patients had echocardiographic evidence of vegetation in any of the cardiac valves.
Data collection
Medical records were reviewed for patient demographics, comorbidities, initial laboratory findings, predisposing cardiac conditions, echocardiographic findings, cardiac surgery, as well as concomitant complications. Acute Physiology and Chronic Health Evaluation (APACHE) IV and Glasgow Coma Scale (GCS) were calculated based on the variables within the first 24 h of admission to the hospital.
Statistical analysis
Descriptive statistics are shown as a mean ± standard deviation or median and interquartile range (IQR) according their distribution; categorical variables as percentages. In the comparison of surgical versus medical treatment group, categorical variables were compared with c2 or Fisher’s exact test; continuous variables were compared using student’s T or Mann–Whitney’s U-tests analysis. Because of the difference of follow-up, a survival analysis was performed to determine factors associated with mortality. Categorical variables were compared with the log-rank test; multivariate analysis was performed with Cox proportional-hazards models which included the variables that had a p-value lower than 0.1. We describe the hazard ratios with a 95% confidence interval that was derived from the Cox proportional-hazards model for bivariate and multivariate analysis. Statistical analysis was performed with Rcmdr program (version 3.5.0).
Results
Participants
From January 2001 to September 2016, we included 105 patients who met the inclusion criteria at our Institution. The incidence rate observed was 7.32 cases/10,000 admissions/year. The global mortality rate for IE was of 36%.
Baseline characteristics are shown in table 1. The median of age of our cohort was of 46 years, 51 (48.6%) of patients were men. Four patients (3.8%) were intravenous drug user; thirty patients (28.6%) had diabetes mellitus; and 33 patients (31.4%) had chronic kidney disease (CKD). The distributions of affected valves were: left-sided valve (mitral and aortic valves) in 65 patients (61.9%) and right-sided valve (tricuspid and pulmonary valves) in 40 patients (38%). Prosthetic valves were involved in three patients (2.9%). Heart failure (48 cases, 45.71% of patients) was the most common complication.
Table 1 Baseline characteristics
| All (n = 105) | MTG (n = 69) | STG (n = 36) | p-value | |
|---|---|---|---|---|
| Male (%) | 51 (48.6) | 34 (49.3) | 17 (47.2) | 0.842 |
| Age (median [IQR])* | 46 [30, 59] | 46 [30, 60] | 45.5 [31, 51.3] | 0.38 |
| Age > 60 (%) | 27 (25.7) | 19 (27.5) | 8 (22.2) | 0.554 |
| DM2 (%) | 30 (28.6) | 21 (30.4) | 9 (25.0) | 0.558 |
| CKD (%) | 30 (28.5) | 27 (39.0) | 3 (8.3) | 0.001 |
| Arterial Systemic Hypertension (%) | 44 (41.9) | 27 (39.13) | 17 (47.22) | 0.29 |
| Previous IE (%) | 3 (2.9) | 2 (2.9) | 1 (2.8) | 1 |
| Charlson > 2 (%) | 46 (43.8) | 35 (50.7) | 11 (30.6) | 0.048 |
| Seizures (%) | 98 (93.3) | 63 (91.3) | 35 (97.2) | 0.418 |
| GCS (median [IQR])* | 15 [14, 15] | 15 [14, 15] | 15 [15, 15] | 0.482 |
| Creatinine mg/dl (median [IQR])* | 1.2 [0.8, 6.0] | 2.0 [0.9, 7.8] | 1.0 [0.7, 1.9] | 0.003 |
| Creatinine > 2 (%) | 41 (39.0) | 34 (49.3) | 7 (19.4) | 0.003 |
| APACHE (median [IQR])* | 16 [13, 21] | 17 [13, 21] | 15 [12, 20] | 0.515 |
| HDAccess (%) | 29 (27.6) | 27 (39.1) | 2 (5.6) | < 0.001 |
| HF (%) | 48 (45.7) | 29 (42.0) | 19 (52.8) | 0.294 |
| LVEF (median [IQR])* | 60 [49, 65] | 60 [49, 65] | 64 [49.5, 67.3] | 0.188 |
| PAP (median [IQR])* | 40 [35, 47.5] | 40 [34.3, 47.5] | 40.5 [35, 45.8] | 0.885 |
| Aneurysm (%) | 2 (1.9) | 1 (1.4) | 1 (2.8) | 1 |
| Valve Perforation (%) | 24 (22.9) | 9 (13) | 15 (41.7) | 0.001 |
| Valve Rupture (%) | 19 (18.1) | 10 (14.5) | 9 (25) | 0.184 |
| Valve Dehiscence (%) | 1 (1.0) | 1 (1.4) | 0 (0.0) | 1 |
| PHV (%) | 3 (2.9) | 2 (2.9) | 1 (2.8) | 1 |
| Valve Abscess (%) | 2 (1.9) | 1 (1.4) | 1 (2.8) | 1 |
| Regurgitation (%) | 90 (85.7) | 56 (81.2) | 34 (94.4) | 0.065 |
| Vegetation > 15 mm (%) | 46 (43.8) | 27 (39.1) | 19 (52.8) | 0.181 |
| Vegetation > 20 mm (%) | 51 (48.6) | 24 (34.8) | 27 (75.0) | < 0.001 |
| Multi-valve (%) | 50 (47.6) | 24 (34.8) | 26 (72.2) | < 0.001 |
| Left valve (%) | 65 (61.9) | 43 (62.3) | 22 (61.1) | 0.904 |
| Fw months (median [IQR])* | 44 [20, 147] | 43.00 [17, 210] | 44 [30.3, 92.8] | 0.72 |
*Median [range IQ1-IQ3] l.
CKD: Chronic Kidney Disease; DM2: diabetes mellitus type 2; Fw: follow-up; GCS: Glasgow Coma Scale; HDAcces: Hemodialysis Access; HF: heart failure;
IE: infective endocarditis; LVEF: left ventricle ejection fraction; PAP: pulmonary artery pressure; PHV: prosthetic heart valve.
In addition, the bivariate analysis between MTG and STG is shown, observing a higher prevalence of CKD in the MTG and greater valvular complications in the STG.
Comparative analysis of both groups
In the bivariate analysis (Table 2), surgical treatment was associated to a lower mortality; however, patients in the medical treatment had a higher frequency of comorbidities (Charlson score), and a higher frequency of chronic kidney disease (creatinine levels and substitutive renal therapy).
Table 2 Bivariate analysis based on mortality
| n = 105 | |||
|---|---|---|---|
| Dead (n = 41, 39%) | Alive (n = 64, 61%) | p value (HR, CI) | |
| Gender | 0.44 | ||
| Male (n = 51, 48.57%) | 21 (20) | 30 (28.57) | |
| Female (n = 54, 51.43%) | 20 (19) | 34 (32.3) | |
| Age* | 45.09 | 46.11 | 0.78 |
| Diabetes Mellitus | 12 (11.42) | 18 (17.14) | 0.45 |
| Chronic Renal Disease | 13 (12.38) | 17 (16.19) | 0.36 |
| Heart Failure | 16 (15.23) | 32 (30.47) | 0.29 |
| Creatinine > 2 mg/dl | 21 (20) | 20 (19.04) | 0.03 |
| Charlson > 2 | 20 (19.04) | 26 (24.76) | 0.53 |
| Pulmonary artery pressure** | 40 | 40 | 0.62 |
| Treatment/procedure | 0.049 (HR 0.37, CI 0.12-0.99) | ||
| Medical treatment | 33 (31.42) | 36 (34.28) | |
| Surgical procedure | 8 (7.6) | 28 (26.66) | |
| Vegetation higher than 15 mm | 21 (20) | 25 (23.8) | 0.05 |
| Left-sided valve | 24 (0.95) | 38 (38) | 0.52 |
| Prosthetic heart valve | 1 (1) | 2 (1.9) | 0.49 |
| Left ventricle ejection fraction** | 60 | 61 | 0.07 |
| Abscess | 1 (0.95) | 1 (0.95) | 1 |
| Perforation | 5 (4.7) | 19 (18.09) | 0.152 |
| Dehiscence | 0 (0) | 1 (0.95) | 0.54 |
| Multi-valve | 19 (18.09) | 31 (29.52) | 0.93 |
| Rupture | 7 (6.66) | 12 (11.42) | 0.83 |
| Glasgow coma scale** | 14 | 15 | 0.005 |
| APACHE* | 18.86±7.5 | 14.35±6.7 | 0.005 |
*Mean ± Standard Deviation.
**Median [range IQ1-IQ3].
HR: hazard ratio; CI: 95% confidence interval.
Survival analysis
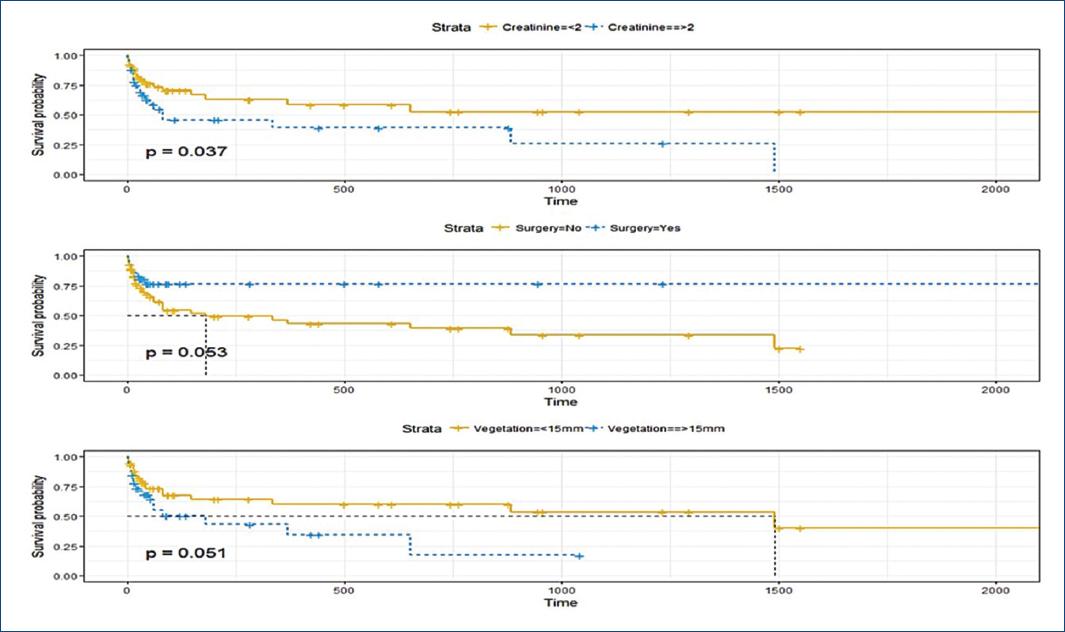
Because of the differences in comorbidities between the medical and surgical groups, we performed a survival analysis to evaluate factors associated with mortality; moreover, we performed a multivariate Cox-regression analysis to evaluate if the surgical treatment is an independent factor associated with improvement in survival. In the bivariate survival analysis, we found that patients who died had: higher creatinine levels, higher APACHE II score, vegetation of more than 15 mm and had lower frequency of surgery (Table 2, Fig. 1).
For the multivariate survival analysis, we include as variables in the model creatinine, vegetation > 15 mm, surgery, and APACHE II. Adjusted for APACHE II, size of vegetation and creatinine, surgery was an independent protective factor to death (Fig. 2). Adjusted for APACHE II surgery, creatinine levels and the size of vegetation, the surgery group had lower mortality than patients on medical treatment group (HR 0.36, p = 0.047) (Table 3).
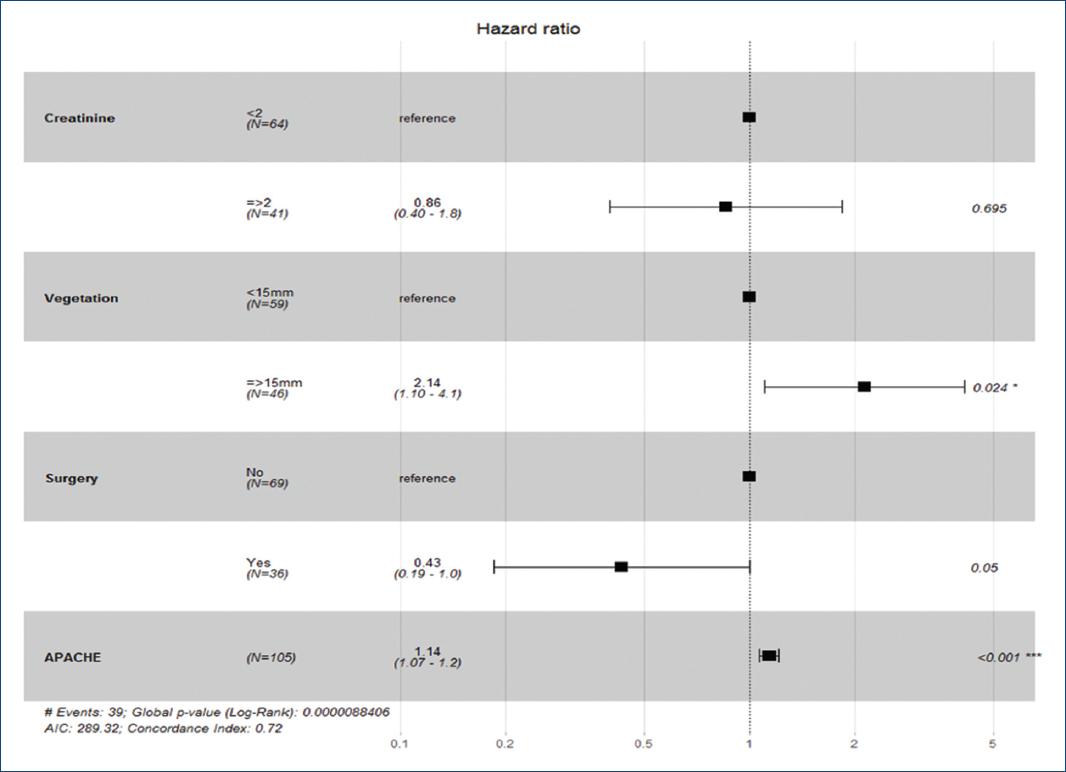
Figure 2 Subgroup analyses of mortality for the variables with statistical difference in bivariate survival analysis.
Table 3 Multivariable logistic regression model for mortality, including variables that were determined a priori to be clinically significant in affecting outcome in EI
| HR, (CI) | p value | |
|---|---|---|
| Surgical Procedure | 0.43, (0.19-0.95) | 0.047 |
| APACHE | 1.14, (1.07-1.2) | 0.001 |
| Left Ventricle Ejection fraction | 0.97 (0.93-1.01) | 0.16 |
| Glasgow Coma Scale | 0.88 (0.74-1.05) | 0.16 |
HR: hazard ratio; CI: 95% confidence interval.
Discussion
Even though the criteria for surgery are well-described, a surgical procedure can be limited for other comorbidities and severity of the disease. In our cohort, not all patients who accomplish criteria of surgery were operated due to clinical instability according to clinical guidelines management. Our first analysis shows that patients who underwent a surgery had lower comorbidities and lower frequency of renal failure. The survival analysis showed that even to adjust for severity (APACHE score) and other factors, mortality surgical procedure showed a reduction in mortality compared with medical treatment. Studies have shown that surgical procedure reduces embolization at central nervous system, without reducing mortality. In our study, we found a relationship between a surgical procedure and the reduction of this; our results agree with the described by Cabell et al.16. In addition, our study describes a global mortality of 39% similar to that reported in medical literature1-3,10,11.
We adjusted the impact in mortality of surgery in the multivariate analysis for variables which had an impact in the bivariate analysis. The variables that showed statistically significant differences were: APACHE scale and surgical procedure, mentioning that patients with a multiple organic failure measured by parameters of the APACHE scale have a higher mortality. The surgical procedure was seen to have an independent influence improving the mortality similar to the described in the literature17.
The limitations of our study are inherent to its retrospective design and being single-center study. It is convenient to conduct a prospective study to validate our findings and, thus, demonstrate the superiority of surgical procedure.
Despite advances in the diagnosis and treatment of IE, its mortality is high. EI has many significant predictors of mortality such as cardiac events (heart failure, moderate or severe regurgitation, etc.), embolization to the central nervous system, and uncontrolled infection, so the use of strategies such as the surgical treatment is essential to improve mortality.











 nueva página del texto (beta)
nueva página del texto (beta)