Introduction
Cardiovascular disease (CVD) was responsible for 31.8% of all deaths in Venezuela in 2017 and has increased by 10.8% in the past decade1 prompting an urgent call for action to implement population-based preventive strategies. Regional adaptation of diagnostic criteria and tools is a mandatory step to implement tailored interventions to reduce CVD burden. For example, using all available data from Asian countries, the World Health Organization recommends lowering body mass index (BMI) cut-points to 23-27.5 kg/m2 as overweight and BMI ≥27.5 kg/m2 as obese, to promote early public health action for Asians2. Complications related to Adiposity-Based Chronic Disease (ABCD)3 are the major modifiable risk factors that underlie CVD, increasing the risk for hypertension, insulin resistance (or Stage 1 dysglycemia-based chronic disease [DBCD]4, and dyslipidemia, which can be viewed as a cluster known as metabolic syndrome (MetS)5. MetS also involves various residual risk factors, such as inflammation, atherogenesis, and platelet hyper-reactivity (prothrombotic state), which independently or together increase the risk for coronary artery disease6, stroke, type 2 diabetes (T2D)7, and cancer5,8.
To estimate the prevalence of MetS and abdominal obesity, the International Diabetes Federation (IDF) recommends adapting waist circumference (WC) cutoffs in different ethnic groups. For Latin American, the IDF recommends applying the values of South Asian countries (90 cm for men and 80 cm for women) until more data are available9. Due to a paucity of cohort studies in Latin America to potentially adapt WC cutoff values associated with the development of CVD events, a variety of strategies have been enlisted. One of the most frequently used strategy is to determine the correlations of different WC cutoffs with individual cardiometabolic components. For example, in 14,893 adults between 35 and 74 years from six cities in Brazil, the optimal WC cutoffs correlating with ≥2 MetS components were 92.0 cm in men and 86.6 cm in women10. In 318 adults older than 18 years from Cuenca city, Ecuador, the optimal WC cutoffs correlating with ≥ 2 MetS components were 95.5 cm in men and 91.5 cm in women11. In 1902 adults with a mean of age 38.7 from Maracaibo city, Venezuela, the optimal WC cutoff correlating with ≥2 MetS components were 95.1 cm in men and 90.2 cm in women12. Finally, in 362 adults from San Cristobal, Venezuela, the optimal WC cutoff correlating with ≥ 2 MetS components was 95.2 cm in men and 88.7 cm in women13. Alternatively, The Latin American Group for the Study of MetS (GLESMO), analyzing data from México, El Salvador, Venezuela, Colombia, and Paraguay, used a different methodology based on the best value to detect 100 cm3 of intraabdominal fat at the 4th and 5th lumbar vertebrae using computer tomography images and recommended a cutoff value of 94 cm in men and 90 cm in women14.
Despite the efforts of these studies, they do not have a national representativity, limiting extrapolation to an entire population. In addition, defining abdominal obesity using only a surrogate of the amount of fat can fail to detect the specific level of adiposity associated with the presence of cardiometabolic risk factors. This is particularly relevant in Latin American populations, where cardiometabolic risk factors remain demonstrable with low amounts of adipose tissue15. Based on these knowledge gaps, the Venezuelan Study of Cardiometabolic Health (EVESCAM, for its acronym in Spanish) database, which includes a national representative evaluation of adults of the eight regions of the country, was interrogated. The aims of this paper were (1) to determine the optimal WC cutoff value associated with ≥2 cardiometabolic alterations; (2) Incorporating this new WC cutoff as part of the diagnostic criteria to determine the prevalence of abdominal obesity and cardiometabolic risk factors related in Venezuela
Methods
Study design
The study design, sampling protocol, and implementation strategies were described previously16,17. In brief, the EVESCAM was a population-based, observational, cross-sectional, and cluster sampling study designed to evaluate cardiometabolic risk factors among subjects aged ≥20 years in Venezuela from July 2014 to January 2017.
Population
A multi-stage stratified sampling method was used to select a representative sample of the general population of Venezuela. Four thousand four hundred fifty-four women and men, aged 20 years and older, were recruited from randomly selected samples in the eight regions of Venezuela. Initially, 23 cities from the eight regions - one to four cities per region - were chosen. Each selected city was stratified by municipalities. Two municipalities in each city, then two parishes in each municipality, and finally, two locations in each parish were randomly selected. Further mapping and census-taking for each location identified the streets or blocks and selected the households that were eventually visited. Inclusion criteria were subjects, 20 years or older, living in the house selected for more than 6 months. Exclusion criteria were current pregnancy, inability to stand or communicate, or refusal to participate in the study by not signing the informed consent.
The target sample size was calculated based on a previous report on diabetes (prevalence 7.7%, standard deviation 1.55%, and confidence level 95%)18 and found to be 2940. Therefore, considering a minimal expected response rate of 70%, the final target sample size was 4200, representing the proportions of the country in terms of age, sex, and proportion of regions. For this study, 4454 subjects were recruited (86.3% urban and 13.7% rural areas), among which 3,420 were evaluated, corresponding to a net response rate of 77.3%.
The study protocol complied with the Helsinki declaration and approved by the National Bioethics Committee (CENABI). Consent from all participants was obtained and filed. The present report is presented according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)19.
Clinical and biochemical measures
A customized questionnaire was used to collect information on demographics, family and personal history, T2D and cardiovascular risk, and socioeconomic status (SES). Questionnaires, anthropometrics, and other physical measurements were obtained by trained and certified health personnel. Blood pressure was measured twice, with 5 min intervals, in the right arm, supported at heart level, in a sitting position, after 5 min of rest, with a validated oscillometric sphygmomanometer (Omron HEM-705C Pint® Omron Healthcare CO., Kyoto/Japan)20. Weight was measured with the lightest possible clothes, without shoes, using a calibrated scale (Tanita UM-081®, Japan). Height was measured using a portable stadiometer (Seca 206® Seca GmbH & Co., Hamburg, Germany). BMI= kg/m2 was calculated for all subjects. WC was measured twice with a metric tape, at the iliac crest, in a horizontal plane with the floor, at the end of expiration, and the average of both was used.
Blood specimens were collected according to a standardized protocol after at least 8-h of fasting. Samples were centrifuged, frozen, and shipped to the central laboratory to be stored at −40° until assay. Blood tests included fasting blood glucose and lipid profile.
Definition of variables
To detect the cardiometabolic components associated with abdominal obesity was used the MetS criteria of the Joint Interim Statement: high triglycerides ≥150 mg/dL; low high-density lipoprotein cholesterol (HDL-c) <40 mg/dL in men or <50 mg/dL in women; high blood pressure ≥130/85 mmHg or use of antihypertensive treatment; and high blood glucose ≥100 mg/dL or self-report of diabetes.21
Abdominal obesity was determined as the WC value associated with ≥2 MetS components described above.
The nutritional state was categorized according to the BMI as underweight <18.5 kg/m2, normal weight 18.5-24.9 kg/m2, overweight 25-29.9 kg/m2, and obesity ≥30 kg/m2. A questionnaire, validated in the Venezuelan population and based on four variables (source of income, profession of householder, educational level, and housing conditions), was used to determine SES. Thus, the population was categorized by 5 strata: SES I - II high-middle-high; SES III - middle; SES IV - poor; and SES V - extreme poverty or extremely poor22.
Data analysis
All calculations were performed using SPSS 20 software (IBM corp. Released 2011; Armonk, NY, USA). Data were weighted to address any imbalance in the distribution of sociodemographic factors in the sample, compared with the whole Venezuelan population. Sampling weights were created using standardized population weights for gender in combination with a second set of weights based on the region/age distribution in Venezuela. Population distributions were obtained from the Venezuelan 2011 census. All continuous variables were initially tested for normality (Q-Q plot and Kolmogorov-Smirnov test) and presented as mean ± standard deviation (SD). Differences between means were assessed by the Student's t-test. Qualitative variables were presented as prevalence and 95% confidence intervals (95% CI) and compared using the Chi-square test. To assess performance of WC for identifying cardiovascular risk, receiver operating characteristics curves, area under the curve (AUC), sensitivity, specificity, and positive likelihood ratios were calculated. The highest sum sensitivity plus specificity favoring sensitivity (when each value was >50%) was used to determine the optimal cutoff value to detect abnormalities. Logistic regressions were made adjusting by age and gender to assess the risk and social factors related to the MetS and its components. p < 0.05 was considered statistically significant.
Results
Subject characteristics
Out of 3454 subjects who completed all stages of data collection, 34 did not complete the evaluation, and 33 had missing data on one or more variables needed. The final sample comprised 3387 participants (Fig. 1). Mean age was 41.2 ± 15.8 years, higher in men than women (p = 0.008) (Table 1). Men showed a worse cardiometabolic profile than women, with higher values of blood pressure, WC, triglycerides, blood glucose, and lower value of HDL-c than women (p < 0.01), despite having a similar BMI. A 39.1% of the population had a university degree and this was higher in women than men (p = 0.002). Almost half of the population was poor and extremely poor SES and 80% were from urban areas.
Table 1 Characteristics of the subjects
| Variable | Men | Women | Total | p |
|---|---|---|---|---|
| n (%) | 1617 (47.7) | 1770 (52.3) | 3387 | |
| Age (years) | 41.9 ± 16.5 | 40.5 ± 15.1 | 41.2 ± 15.8 | 0.008 |
| Systolic BP (mmHg) | 130.5 ± 19.3 | 123.1 ± 19.3 | 126.6 ± 20.7 | <0.001 |
| Diastolic BP (mmHg) | 75.7 ±11.6 | 74.7 ± 11.4 | 75.2 ± 11.5 | 0.008 |
| BMI | 26.7 ± 5.4 | 27.0 ± 6.3 | 26.8 ± 5.9 | 0.114 |
| Waist circumference (cm) | 92.9 ± 14.0 | 90.4 ± 14.0 | 91.6 ± 14.1 | <0.001 |
| Triglycerides (mg/dL) | 116.7 ± 72.7 | 100.6 ± 54.3 | 108.3 ± 64.3 | <0.001 |
| HDL-c (mg/dL) | 34.9 ± 10.4 | 38.7 ± 11.2 | 36.9 ± 11.0 | <0.001 |
| Blood glucose (mg/dL) | 105.2 ± 33.5 | 99.3 ± 26.2 | 102.1 ± 30.1 | <0.001 |
| Academic degree (%) | 0.001 | |||
| Primary | 19.0 (15.2-18.8) | 18.1 (15.0-18.4) | 18.5 (15.3-17.8) | |
| Secondary | 45.2 (42.8-47.6) | 39.8 (37.5-42.1) | 42.4 (40.7-44.1) | |
| University | 35.8 (33.5-38.1) | 42.2 (39.9-44.5) | 39.1 (37.5-40.7) | |
| Social economic stratus (%) | ||||
| V - Extremely poor | 6.3 (5.1-7.3) | 5.1 (4.1-6.1) | 5.7 (5.0-6.5) | 0.152 |
| IV - Poor | 40.7 (38.3-43.1) | 43.3 (41.0-45.6) | 42.0 (40.3-43.7) | |
| III - Middle | 30.8 (28.6-33.1) | 31.4 (29.2-33.6) | 31.1 (29.5-32.7) | |
| I-II - High/Middle-High | 22.3 (20.2-24.3) | 20.2 (18.3-22.0) | 21.2 (19.8-22.5) | |
| Location (%) | ||||
| Urban | 82.3 (80.4-84.2) | 79.3 (77.4-81.2) | 80.8 (79.5-82.1) | 0.029 |
| Rural | 17.7 (15.8-19.6) | 20.7 (18.8-22.6) | 19.2 (17.9-20.5) |
Data are presented as mean ± SD. Proportions are presented as percent and 95% CI. BP: blood pressure; HDL-c: high-density lipoprotein cholesterol
Optimal WC
To determine the WC associated with ≥2 cardiometabolic alterations, the AUC was 0.75 (95% CI; 0.73-0.78) in men and 0.73 (95% CI; 0.71-0.76) in women (Fig. 2), corresponding to a probability around 74% to detect subjects with ≥2 alterations. Using the best tradeoff between sensitivity and specificity, a cutoff value of 90 cm in men (sensitivity = 72.4% and specificity = 66.1%) and 86 cm in women (sensitivity= 76.2% and specificity = 61.4%) were optimal for aggregation of ≥ 2 alternations in Venezuelan adults (Table 2).

Figure 2 Receiver operating characteristic curves constructed to determine waist circumference cutoff points for the detection of multiple risk factor aggregations in the general population by gender.
Table 2 Sensitivity, specificity, sum, and likelihood ratio of abdominal circumference cutoff point
| Men | Women | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cut point | Sensitivity | Specificity | Sum | +LR | Cut point | Sensitivity | Specificity | Sum | +LR |
| 86 | 81.5 | 52.4 | 1.339 | 1.71 | 82 | 85.9 | 44.7 | 1.306 | 1.55 |
| 87 | 78.8 | 54.3 | 1.331 | 1.72 | 83 | 84.5 | 48.3 | 1.328 | 1.63 |
| 88 | 76.2 | 56.7 | 1.329 | 1.76 | 84 | 81.0 | 51.8 | 1.329 | 1.68 |
| 89 | 73.8 | 60.1 | 1.339 | 1.84 | 85 | 79.4 | 56.9 | 1.363 | 1.84 |
| 90 | 72.4 | 66.1 | 1.385 | 2.13 | 86 | 76.2 | 61.4 | 1.376 | 1.97 |
| 91 | 69.5 | 68.5 | 1.380 | 2.20 | 87 | 72.4 | 63.1 | 1.354 | 1.95 |
| 92 | 67.3 | 73.0 | 1.403 | 2.49 | 88 | 70.4 | 65.6 | 1.360 | 2.04 |
| 93 | 65.0 | 75.2 | 1.402 | 2.62 | 89 | 66.9 | 68.5 | 1.355 | 2.12 |
| 94 | 62.0 | 78.3 | 1.403 | 2.85 | 90 | 63.7 | 70.4 | 1.342 | 2.15 |
+LR: likelihood ratios.
Prevalence of abdominal obesity and cardiometabolic risk factors
With these cutoff values, the prevalence of abdominal obesity in Venezuela was 59.6% (95% CI; 57.5-61.7), similar between genders. Incorporating this new WC cutoff as part of the diagnostic criteria, the prevalence of MetS was 47.6% (95 CI; 45.2-50.0), higher in men (50.0% [95 CI; 47.7-52.3) than in women (45.4% [95 CI; 42.9-47.8) (p= 0.007) (Table 3). Low HDL-c was the most prevalent alteration (78%), followed by abdominal obesity (59.6%), high blood glucose (43.6%), and high blood pressure (39.6%). Men presented a higher prevalence of high blood pressure, blood glucose, and triglycerides, but a lower prevalence of low HDL-c than women (p < 0.01). All cardiometabolic risk factors, except low HDL, increased with age (p < 0.001). In the group with 70 years or older, the prevalence of MetS was 72.3%, driven by a very high prevalence of high blood pressure in this age group (79.6%).
Table 3 Prevalence of cardiometabolic risk factors
| Variables | MetS | High blood pressure | High triglycerides | Abdominal obesity | Low HDL-c | High blood glucose |
|---|---|---|---|---|---|---|
| Total | 47.6 (45.2-50.0) | 39.6 (37.0-42.2) | 22.7 1(19.7-25.7) | 59.6 (57.5-61.7) | 78.0 (76.4-79.6) | 43.6 (41.1-46.1) |
| Men | 50.0 (47.7-52.3) | 44.5 (41.8-47.2) | 24.7 (21.7-27.8) | 59.1 (56.7-61.5) | 71.2 (69.5-72.9) | 49.4 (46.9-52.0) |
| Women | 45.4 (43.0-47.8) | 35.0 (32.5-37.6) | 20.9 (18.0-23.8) | 60.0 (57.7-62.3) | 84.3 (82.9-85.7) | 38.3 (35.8-40.8) |
| p | 0.007 | <0.001 | 0.008 | 0.612 | <0.001 | <0.001 |
| Age | ||||||
| 20-44 | 35.7 (33.4-38.0) | 24.3 (22.0-26.6) | 15.7 (13.1-18.3) | 51.8 (49.6-54.0) | 80.5 (79.0-82.0) | 34.8 (32.4-37.2) |
| 45-69 | 65.8 (63.5-68.1) | 61.1 (58.5-63.7) | 33.3 (30.0-36.6) | 72.8 (70.9-74.8) | 74.7 (73.0-76.4) | 56.6 (54.0-59.1) |
| ≥9. | 72.3 (70.1-74.5) | 79.6 (77.4-81.8) | 37.4 (34.0-40.9) | 68.0 (66.0-70.0) | 70.9 (69.1-72.6) | 63.1 (60.6-65.6) |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Proportions are presented as percent and 95% CI. Abbreviations: HDL-c: high-density lipoprotein cholesterol; MetS: metabolic syndrome.
Independent of age and gender, the prevalence of MetS and all its components increased with the presence of overweight and obesity. Compared with normal-weight subjects, the OR related to MetS was 7.2 (95% CI; 5.9-8.9) in those with overweight and 20.4 (95% CI; 16.1-26.0) in those with obesity. The MetS components in subjects with overweight ranged from OR = 1.7 (95% CI; 1.4-2.0) for high blood glucose to 19.3 (95% CI; 15.5-24.0) for abdominal obesity; in those with obesity ranged from OR = 2.2 (95% CI; 1.9-2.7) to OR = 382.3 (95% CI; 199.6-731.9), respectively. Subjects in the lowest SES had a lower risk for abdominal obesity than higher SES (Table 4), the rest of cardiometabolic risk factors were not related to academic degree, SES, or location rural/urban.
Table 4 Risk factors related to cardiometabolic components
| Variables | MetS | High blood pressure | High triglycerides | Abdominal obesity | Low HDL-c | High blood glucose |
|---|---|---|---|---|---|---|
| Nutritional status | ||||||
| Normal weight | 1 | 1 | 1 | 1 | 1 | 1 |
| Low weight | 0.2 (0.1-0.4) | 0.6 (0.4-1.1) | 0.2 (0.1-0.5) | 0.0 (0.0-0.2) | 0.6 (0.4-0.9) | 0.7 (0.5-1.0) |
| Overweight | 7.2 (5.9-8.9) | 3.0 (2.4-3.6) | 1.8 (1.5-2.3) | 19.3 (15.5-24.0) | 1.9 (1.5-2.3) | 1.7 (1.4-2.0) |
| Obesity | 20.4 (16.1-26.0) | 4.7 (3.8-5.8) | 3.0 (2.4-3.8) | 382.3 (199.6-731.9) | 3.3 (2.6-4.3) | 2.2 (1.9-2.7) |
| Academic degree | ||||||
| Primary | 1 | 1 | 1 | 1 | 1 | 1 |
| Secondary | 1.2 (0.9-1.5) | 1.1 (0.9-1.4) | 0.9 (0.7-1.2) | 1.4 (1.1-1.7) | 0.7 (0.5-0.9) | 0.9 (0.7-1.2) |
| University | 0.9 (0.7-1.2) | 0.9 (0.7-1.2) | 1.2 (0.9-1.5) | 1.2 (0.9-1.4) | 0.5 (0.3-0.6) | 0.9 (0.8-1.2) |
| Social-economic status | 1 | 1 | 1 | 1 | 1 | 1 |
| V - Extremely poor | 1.3 (0.9-1.8) | 1.4 (1.0-2.0) | 1.0 (0.7-1.5) | 1.8 (1.3-2.4) | 1.1 (0.7-1.6) | 1.2 (0.9-1.7) |
| IV - Poor | 1.2 (0.8-1.6) | 1.4 (1.0-2.0) | 1.1 (0.8-1.7) | 1.9 (1.4-2.7) | 0.9 (0.6-1.3) | 1.4 (1.0-1.9) |
| III - Middle | 1.1 (0.8-1.6) | 1.3 (0.9-1.9) | 1.2 (0.8-1.9) | 1.8 (1.3-2.6) | 0.8 (0.5-1.1) | 1.0 (0.7-1.4) |
| I-II - High/Middle-High | ||||||
| Location | ||||||
| Rural | 1 | 1 | 1 | 1 | 1 | 1 |
| Urban | 1.1 (0.9-1.3) | 1.0 (0.9-1.3) | 1.1 (0.9-1.4) | 1.0 (0.89-1.2) | 0.8 (0.6-1) | 1.0 (0.8-1.2) |
Logistic regression is presented as OR and 95% CI. Abbreviations: HDL-c: high-density lipoprotein cholesterol; MetS: metabolic syndrome.
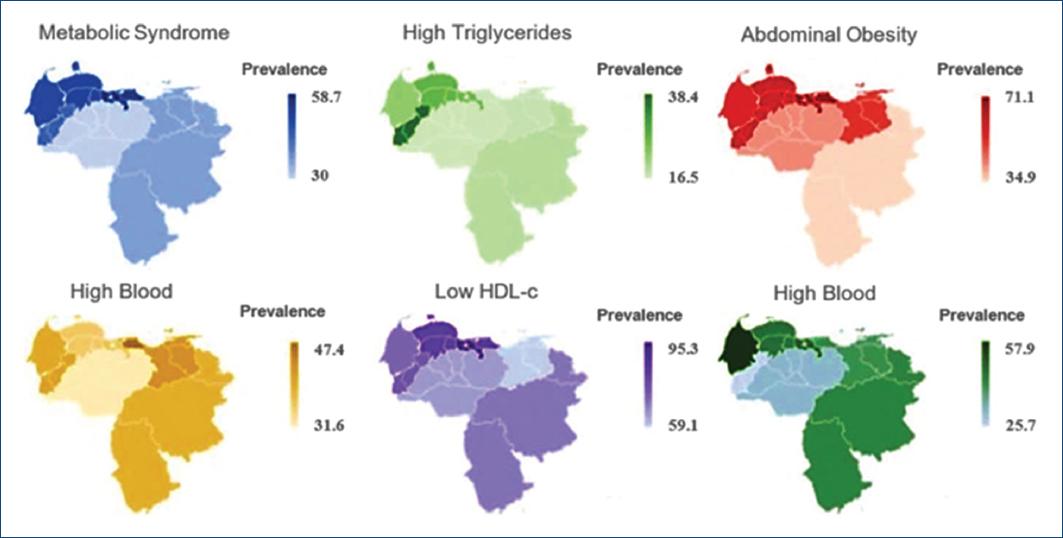
The prevalence of cardiometabolic risk factors was different among diverse regions of the country. The prevalence of MetS was higher in the regions located at northern and western of Venezuela (Fig. 3), driven by high prevalence rates associated with abdominal obesity, low HDL-c, and high blood glucose (p < 0.001). In the central region, the prevalence of low HDL-c was 95.3%, whereas in Los Llanos (Plains), located in the middle on the country, presented the lowest prevalence of MetS, related to the lowest prevalence of high blood pressure and triglycerides, the second-lowest prevalence of low HDL-c, abdominal obesity, and high blood glucose (p < 0.001).
Discussion
Waist circumference cutoff values of 90 cm for men (sensitivity= 72.4% and specificity = 66.1%) and 86 cm for women (sensitivity= 76.2% and specificity = 61.4%) were optimal for the detection of cardiometabolic risk factor aggregation. Using these cutoffs, the prevalence of abdominal obesity was 59.6% (95% CI 57.5-61.7), similar between genders. MetS prevalence was 47.6%, higher in men than women, and increased with age (except low HLD-c) and BMI. The prevalence of cardiometabolic risk factors also varied by regions, being higher in those areas located at the northern and western parts of the country and lower at Los Llanos.
Compared with previous studies, including the Venezuelan population, the WC cutoff values in this study based on the EVESCAM registry are the lowest reported at this date. Specifically, in men, the WC value was 90 cm using EVESCAM data, compared with Maracaibo city of 95.1 cm (12); San Cristobal city of 95.2 cm (13); and GLESMO (Mexico, El Salvador, Venezuela, Colombia, and Paraguay) of 94 cm (14). In women, the figures for EVESCAM are 86 cm, compared with Maracaibo city of 90.2 cm (12); San Cristobal city of 88.7 cm (13); and GLESMO of 92 cm (14). The lower values found in this report are associated with the elevated prevalence of MetS components: low HDL-c (78.0%) and high blood glucose (43.6%), which were 38% and 80% higher than the values observed in Maracaibo city (12). Compared with other locations, in men, this value was also lower than the observed in Ecuador (95.5 cm) (11), Brazil (92 cm) (10), and Portugal (93.5 cm)23, but higher than Japan (85 cm)24 and in eight countries of Sub-Sahara Africa (81 cm)25. In women, this value was also lower than the observed in Ecuador (91.5 cm) (11) and Portugal (89 cm)23, similar than Brazil (10), but higher than Japan (80 cm)24 and in eight countries of Sub-Sahara Africa (81 cm)25.
The prevalence of MetS in this report (47.6%) was higher than that observed in previous studies, including populations from three regions of Venezuela between 2006 and 2010 (35.7%)26, and higher than other reports presented in five countries in Central America at 30.3%27, and the US at 34.7%28. However, the comparison among these studies is very limited because many different definitions of MetS were used, the most frequently used was the Adult Treatment Panel III (ATPIII) criteria29. The limitation of the ATPIII definition is that by relying on impaired fasting glucose, BMI, and waist circumference, alone, the proportion of subjects at risk including Stage 1 DBCD (insulin resistance and other forms of ABCD with normal BMI and WC, but abnormal adiposity distribution or function) and Stage 2 DBCD (prediabetes with impaired glucose tolerance) is underestimated. This limitation is compounded by biometric cutoffs (BMI, waist circumference, blood glucose, etc.) that may differ among the various ethnocultural populations in Latin American adults, which is a population that develops inflammation, insulin resistance, and CVD at lower levels of adiposity30. These variations were observed in a systematic review, including 12 studies in Latin America, where the prevalence of MetS ranged from 18.8% to 43.3%, and the prevalence of each modifiable CVD risk component significantly varied among populations31. In comparison with Cacucasians, studies in Venezuelan population have described the presence of obesity (excess of adiposity) at lower cutoffs for BMI (27.5), insulin resistance at lower HOMA, MetS at lower epicardic fat, and metabolic abnormalities at lower WC12,14,32,33.
Unhealthy eating patterns and physical inactivity are the main drivers of cardiometabolic alterations34. Hence, the high prevalence of cardiometabolic risk factors in Venezuela is not surprising, considering the stressful environment. An adverse lifestyle among inhabitants typically results from chronic social, political, and economic turmoil35. Chronic stress acts in the brain, increasing appetite, locomotor activity, and food-seeking behavior36. High glucocorticoid levels are related to unhealthy behaviors37. Glucocorticoids increase appetite, especially for foods rich in salt, trans fat, and high caloric content and are related to chronic fatigue, which leads to a sedentary lifestyle; additionally, endogenous glucocorticoids promote abdominal obesity, insulin resistance, salt retention, and immunosuppression38,39. Chronic stress also activates the sympathoadrenal and pituitary-adrenal axes increasing cardiac output and peripheral vascular resistance, which elevate blood pressure40. The effects of stress on inflammation, T2D, obesity, and CVD are mediated by direct innervations of lymphatic tissue and complex effects on behaviors that affect dietary patterns and physical activity35. Interestingly, these changes appear despite parallel effects of a stressful environment generated by the widespread humanitarian crisis in Venezuela that reduces the access to calorically dense food (e.g., oils) and increase non-programmed physical activities (primarily due to the lack of public transportation).
The main limitation of this study is the cross-sectional design, impeding to determine causal relation, future prospective studies are mandatory to determine which WC cutoffs predict CVD events, T2D, and mortality. Different fat measurements, especially visceral fat by IMAGEN studies, are better predictors of cardiometabolic risk factors and were not measured in the present study; however, these measurements are complicated to implement and represent an elevated cost in daily practice. The strengths of this report include the national representativeness of EVESCAM, including subjects with 20 years or older from the eight regions of the country, the formal sampling method, and a unique setting influenced by extraordinary stress. Thus, the results of the current study could be generalized to the full adult population of Venezuela.
Conclusion
A WC cutoff value of 90 cm for men and 86 cm for women were related with higher sensitivity and specificity associated with ≥2 cardiometabolic risk factors. Incorporating this new WC cutoff as part of the diagnostic criteria was found a high prevalence of abdominal obesity and MetS in the country. The specific drivers of cardiometabolic alterations in this unique population setting need to be evaluated but social determinants appear to be very important contributing factors.











 nueva página del texto (beta)
nueva página del texto (beta)