Introduction
Overweight and obesity (O/O) are defined as excessive accumulation of fat that can lead to hormonal, inflammatory, and metabolic interactions that adversely affect all organs and systems. In the heart, the accumulation of free and intermediate fatty acids causes cardiac lipotoxicity, a phenomenon that implies an increase of β-oxidation and excessive reactive oxygen species production. The excess of adipocytes in the body and inside the myocardium generate an inflammatory environment due to exposure to inflammatory cytokines that in the heart is translated by the precipitation of apoptosis and fibrosis of the cardiomyocytes. When this toxic environment is perpetuated it leads to irreversible structural and functional damage of the cardiac fiber1,2. Large epidemiological studies have associated obesity with an increase in the incidence of heart failure, even doubling its risk3,4; additionally, O/O and abdominal obesity increases the incidence of aortic valve stenosis5 and is also associated with the progression6. In addition, both O/O and aortic valve stenosis coexist, and combined they cause greater damage to the cardiac fiber, since, on the one hand, there is an increase in systolic stress that inevitably leads to hypertrophy and myocardial fibrosis and, on the other hand, cardiac fiber is also exposed to a toxic and inflammatory environment that also leads to apoptosis and fibrosis7,8. In a previous study, our group evaluated the characteristics of ventricular remodeling in myocardial biopsies, in patients whit O/O and severe aortic stenosis (SAS); we observed that this association caused greater fibrosis and fat infiltration compared with the group of patients with SAS without O/O9. This increased presence of fibrosis in patients with SAS and O/O suggests that aortic valve replacement (AVR) surgery may be more at risk and one of the main complications that increase morbidity and mortality in the post-surgical period is the low cardiac output syndrome (LCOS)10. In cardiac surgery, several risk factors have been associated with LCOS11-17. On the other hand, the large study by Mariscalco et al.18 concluded that in cardiac surgery O/O are even associated as a protective factor, except for obesity Grade 3; we think that given the double aggression in the myocardium produced by SAS and O/O, post-operative behavior could be different and confer greater risk in the development of LCOS, in comparison with the rest of cardiac surgeries; therefore, the objective of this study was to investigate whether O/O is an associated risk factor for developing LCOS in patients with isolated SAS undergoing AVR.
Methods
A retrospective observational study of the analytic cohort was performed, which consecutively included all the patients with SAS who underwent surgery scheduled for AVR in a period from 2015 to 2016; the selection diagram is shown in figure 1. Demographic data of the patients, their comorbidities, as well as their intra and post-operative evolution during the first 30 days or until hospital discharge were collected. Patients with previous cardiac surgery, associated moderate or severe valvular lesions, functional class III/IV of the NYHA, emergency surgery, left ventricular ejection fraction <50%, need of revascularization, malnutrition (body mass index [BMI] < 18.5 kg/m2), pre-operative plasmatic hemoglobin concentration < 12 and < 14 g/dL in women and men, respectively19, lymphocytes < 2000 cells/mL, serum creatinine > 1.4 mg/dL were excluded from the study. Patients in whom a cardioplegia was different from Custodiol® or those with surgical accidents and prosthetic mismatch (effective orifice area with continuous Doppler ≤ 0.85 cm2/m2)20 were also excluded from the study. None of our patients had right ventricular failure in this study. Finally, all the patients had cardiopulmonary bypass use.
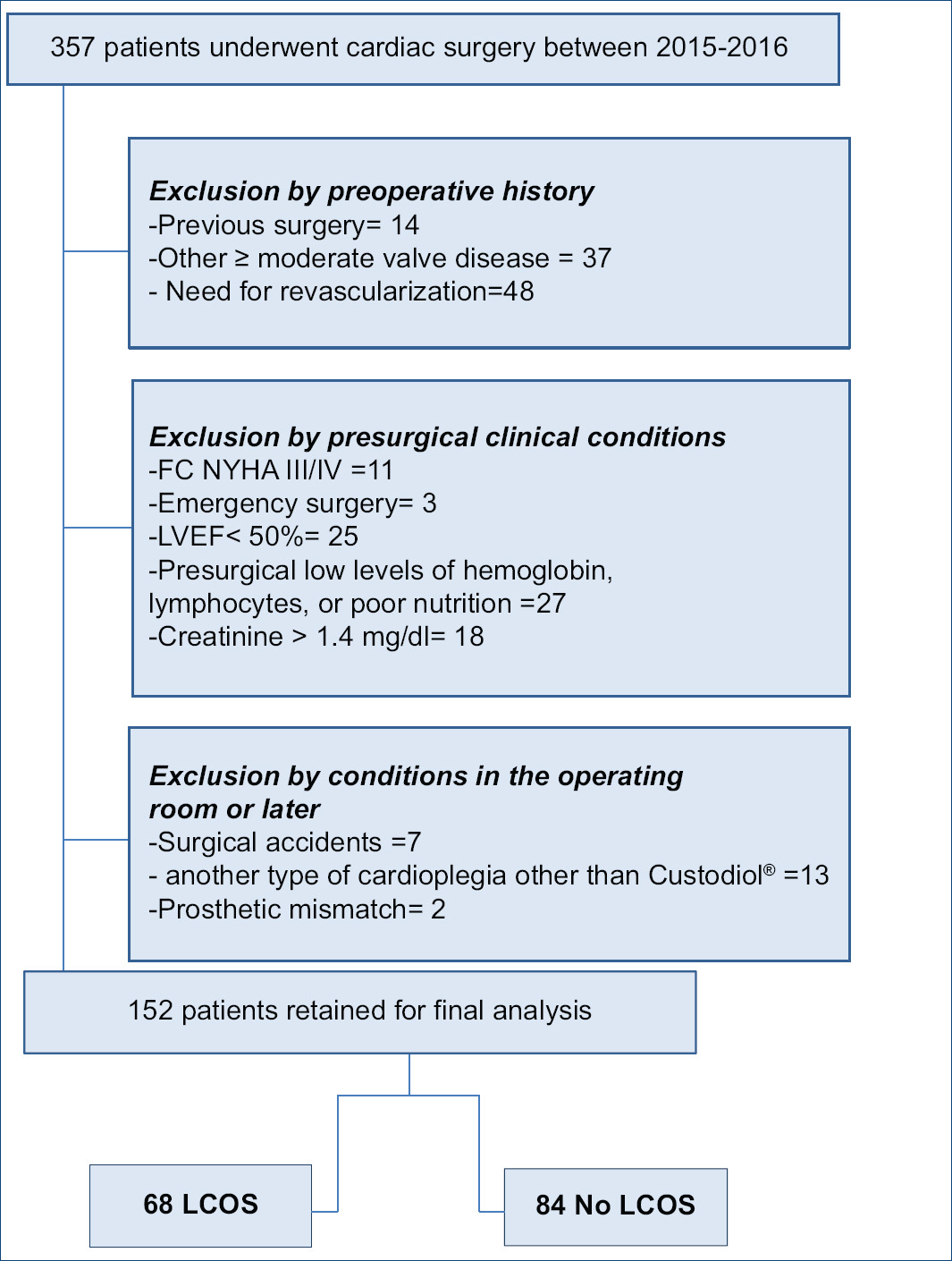
Figure 1 Patient selection. SAS: Severe aortic stenosis; FC NYHA: Functional Class of New York Hear Association; LVEF: left ventricular ejection fraction.
LCOS was diagnosed if in intensive care unit, after correction of all abnormalities of electrolytes and blood gases and after adjusting the preload to its optimal value the patient required inotropic medication (dopamine, dobutamine, or epinephrine) to maintain systolic blood pressure by at least 90 mmHg and cardiac output by 2.2 l/min/m2 for 30 min or more21.
According to the BMI kg/m2 (BMI), the patients were divided into three groups: normal weight (NW) group (NW, BMI between 18.5 and < 25 kg/m2), overweight with BMI 25 and < 30 kg/m2, and obese group with BMI of 30 kg/m2 or more.
Evaluation of echocardiograms
The reports of two-dimensional transthoracic echocardiography performed on patients before AVR surgery were reviewed (all were performed at least 6 months before the surgical event). SAS was considered when an aortic transvalvular velocity ≥ 4 m/s and mean gradient ≥ 40 mmHg were detected by continuous Doppler. We also collected: left ventricular mass and ejection fraction, left atrium volume, systolic pulmonary pressure, diastolic function and gradients, velocities, and valve area. If in addition to SAS, there was regurgitation greater or equal to moderate, with vena contracta method of 4 mm, and descending aortic reverse velocity > 15 cm/s, it was defined as mixed aortic valve disease. After surgery, prosthetic valve function was evaluated by transthoracic echocardiography in those cases with LCOS.
Statistical analysis
The categorical variables were summarized in frequency and proportions. The numerical variables are summarized as mean and standard deviation or median and 25th and 75th percentiles, according to their distribution. We performed a bivariate analysis with Students T or ANOVA for the quantitative variables with normal distribution; MannWhitney U- or Kruskal-Wallis test was used for quantitative variables with non-parametric distribution, and Pearsons Chi-square test or linear trend for categorical variables. Univariate and multivariate analyses were performed with logistic regression to determine the predictors of LCOS. A value of two-tailed p < 0.05 was considered as significant. All the analysis was performed with the statistical package SPSS version 21.
Results
152 patients were included in the study, 45 (29.6%) had NW, 60 were overweight (39.5%), and 47 obese (30.9%); demographic and echocardiography findings are shown in Table 1. There were no differences in sex, age, history of type 2 diabetes mellitus, smoking, maximum and medium gradients, aortic valve area, left ventricular ejection fraction, or diastolic dysfunction. The prevalence of hypertension (HT) was higher in the O/O groups compared to the NW group: 66.7%, 83%, and 55.6%, respectively p < 0.0001. On the other hand, left ventricular mass, left atrium volume, and systolic pulmonary pressure were higher in the O/O compared to NW group, in all p < 0.001.
Table 1 Demographic and echocardiography findings divided by groups
| Total, group n = 152 | Normal weight (29.6%) n = 45 | Overweight (39.5%) n = 60 | Obesity (30.9%) n = 47 | p | |
|---|---|---|---|---|---|
| Age (years) | 67 ± 10 | 67 ± 13 | 67 ± 10 | 66 ± 8 | 0.747* |
| Male sex (%) | 82 (53.9) | 25 (55.6) | 37 (61.7) | 20 (42.6) | 0.205^ |
| Weight (kg) | 71 ± 11 | 62. ± 9 | 71 ± 9 | 80 ± 9 | < 0.0001* |
| Height (mts) | 1.60 (1.52-1.68) | 1.64 (1.53-1.68) | 1.62 (1.53-1.68) | 1.56 (1.50-1.64) | 0.056+ |
| BMI (kg/m2) | 27.7 ± 3.7 | 23.5 ± 1.2 | 27.7 ± 1.0 | 32.3 ± 2.1 | < 0.0001* |
| HT (%) | 104 (68.4) | 25 (55.6) | 40 (66.7) | 39 (83) | < 0.0001^ |
| HT (Years of diagnosis) | 5.5 (1-15) | 5 (2-10) | 4.5 (2-9) | 7 (4-14) | 0.07+ |
| Treatment for SAH | 0.91* | ||||
| ACE-I or ARA2 (%) | 59 (57) | 15 (60) | 23 (58) | 21 (54) | |
| BB (%) | 8 (7.6) | 0 | 4 (10) | 4 (10.2) | |
| CC (%) | 5 (4.8) | 1 (4) | 1 (2.5) | 3 (7.6) | |
| Diuretic (%) | 1 (0.9) | 0 | 1 (2.5) | 0 | |
| ACE-I ARA2+diuretic (%) | 12 (12) | 2 (8) | 4 (10) | 6 (15) | |
| ACE-I o ARA2 + BB (%) | 8 (7.6) | 2 (8) | 3 (5.0) | 3 (7.6) | |
| Triple therapy (%) | 5 (4.8) | 3 (12) | 1 (2.5) | 1 (2.5) | |
| Without treatment (%) | 6 (5.7) | 2 (8) | 3 (7.5) | 1 (2.5) | |
| T2DM (%) | 28 (18) | 9 (20) | 12 (20) | 7 (15) | 0.525^ |
| Smoking (%) | 52 (33) | 14 (50) | 12 (38) | 10 (42) | 0.524^ |
| Aortic valve diagnosis: | 0.057^ | ||||
| ISAS (%) | 100 (66) | 26 (58) | 38 (64) | 36 (77) | |
| MAVD (%) | 52 (34) | 19 (42) | 22 (37) | 11 (23) | |
| Maximum gradient (mmHg) | 92 ± 21 | 91 ± 21 | 92 ± 18 | 94 ± 24 | 0.903* |
| Mean gradient (mmHg) | 57 (45-71) | 58 (44- 65) | 55 (47- 70) | 57 (41-74) | 0.953+ |
| Aortic area (cm2) | 0.6 (0.5-0.7) | 0.6 (0.5-0.7) | 0.6 (0.5-0.8) | 0.6 (0.5-07) | 0.742+ |
| LVEF (%) | 61 (60-65) | 64 (60-70) | 61 (60-65) | 60 (58-65) | 0.170+ |
| Diastolic dysfunction E/A (%) | 0.098^ | ||||
| Grade 1 | 116 (75) | 38 (84) | 40 (68) | 38 (81) | |
| Grade 2 | 31 (20) | 5 (11) | 17 (28) | 9 (19) | |
| Grade 3 | 5 (3.2) | 2 (4.4) | 3 (5.0) | 0 | |
| Left ventricular mass (gr/m2) | 126 ± 17 | 117.9 ± 20 | 128.7 ± 15 | 130.2 ± 15 | < 0.001* |
| Left atrial volume (ml/m2) | 32.8 ± 5 | 29 ± 4 | 32.5 ± 5 | 36.6 ± 5 | < 0.001* |
| SPP (mmHg) | 27 ± 8 | 26 ± 8 | 30 ± 8 | 31 ± 8 | < 0.001* |
HT: systemic hypertension; BMI: body mass index; ACEI: angiotensin-converting enzyme inhibitor; ARA 2: angiotensin 2 receptor antagonist blocker; BB: beta-blocker; CC: calcium receptor antagonist; T2DM: type 2 diabetes mellitus; ISAS: isolated severe aortic stenosis; MAVD: mixed aortic valve disease (stenosis and regurgitation); LVEF: left ventricular ejection fraction; SPP: systolic pulmonary pressure. Comparison with one-way ANOVA test (*), Kruskal-Wallis test (+) and Lineal trend Chi-square (^).
Operative and post-surgical characteristics of the patients are shown in table 2; there were no differences in extracorporeal circulation time, aortic clamping time, or prosthetic valve size. Central venous pressure and pulmonary capillary pressure were higher in the O/O groups compared to NW patients, with p < 0.019 and < 0.0001, respectively. Global incidence of LCOS was 44.7%, being more frequent in the O/O groups compared to NW group: 43.3%, 68.1%, and 22.2%, respectively, p < 0.05 in overweight and p < 0.0001 in obesity.
Table 2 Surgical and post-surgical variables
| Total group n = 152 | Normal weight (29.6%) n = 45 | Overweight (39.5%) n = 60 | Obesity (30.9%) n = 47 | p | |
|---|---|---|---|---|---|
| ECT (min) | 93 (75-124) | 94 (78-105) | 92 (73-110) | 94 (80-117) | 0.929+ |
| ACT (min) | 68 (52-87) | 69 (55-84) | 67 (55-79) | 68 (55-80) | 0.805+ |
| Prostheses size, (Diameter in mm) | 21.5 ± 1.6 | 21.4 ± 1.5 | 21.5 ± 1.7 | 21.4 ± 1.7 | 0.944* |
| BSA (m2) | 1.77 (1.67-1.88) | 1.77 (1.65-1.91) | 1.79 (1.70-1.87) | 1.78 (1.67-1.85) | 0.872+ |
| Valve type (%) | < 0.001^ | ||||
| Mechanical | 67 (44.1) | 17 (37.8) | 28 (62.2) | 22 (46.8) | |
| Bio-prostheses | 85 (55.9) | 28 (46.7) | 32 (53.3) | 25 (53.2) | |
| Annular enlargement (%) | 8 (5.2) | 4 (8.8) | 2 (3.4) | 2 (4.2) | 0.453^ |
| CVP (cmH20) | 11 (9-14) | 10 (9-12) | 11 (9-14) | 12 (11-15) | 0.019+ |
| PCP (mmHg) | 13 ± 4 | 10 ± 5 | 14.5 ± 7 | 16 ± 5 | < 0.0001* |
| Low cardiac output syndrome (%) | 68 (44.7) | 10 (22.2) | 26 (43.3) | 32 (68.1) | < 0.0001^ |
ECT: extracorporeal circulation time; ACT: aortic clamping time; BSA: body surface area; CVP: central venous pressure; PCP: pulmonary capillary pressure. Comparison with One-Way ANOVA test (*), Kruskal-Wallis test (+) and Lineal trend Chi-square (^).
We also assessed the effect of BMI and the presence or absence of LCOS with the former analyzed as continuous numerical variable; in this setting, we found that the female sex, HT, BMI Kg/m2, left ventricular mass, and the labeled valve size were associated with LCOS, p < 0.02, p < 0.02, p < 0.001, p < 0.032, and p < 0.045, respectively. Mortality was higher in patients who developed LCOS, p < 0.02 (Table 3). The identified causes of death were cardiogenic shock (six patients, 46.1%); septic shock (six patients, 46.1%), and one patient had mixed shock (septic and cardiogenic, 7.69%). About 84.6% of the deaths occurred in patients with O/O, and 15.3% were in NW.
Table 3 Factors associated with LCOS
| No LCOS n = 84 | LCOS n = 68 | p | |
|---|---|---|---|
| Labeled valve size | 21.7 ± 1.5 | 21.1 ± 1.7 | < 0.045 |
| Age (years) | 65.8 ± 10.4 | 67.5 ± 9.9 | 0.290 |
| BMI (kg/m2) | 26.5 ± 3.2 | 29.2 ± 3.8 | < 0.001 |
| Left atrial volume (ml/m2) | 32.2 ± 5.4 | 33.7 ± 5.4 | 0.087 |
| Left ventricular mass(grs/m2) | 123 ± 18 | 129 ± 16 | < 0.032 |
| SPP (mmHg) | 29 ± 9 | 30 ± 8 | 0.673 |
| Maximum gradient (mmHg) | 93.1 ± 20 | 91.4 ± 22 | 0.712 |
| Mean gradient (mmHg) | 59 ± 18 | 53 ± 21 | 0.205 |
| Aortic valve area cm2 | 0.64 ± 0.1 | 0.63 ± 0.1 | 0.700 |
| LVEF (%) | 63 ± 7 | 62 ± 5 | 0.281 |
| ECT (min) | 68 ± 17 | 72 ± 25 | 0.518 |
| ACT (min) | 93 ± 25 | 102 ± 34 | 0.124 |
| Women (%) | 30 (36) | 40 (59) | < 0.02 |
| HT (%) | 49 (58) | 55 (81) | < 0.02 |
| T2DM (%) | 14 (17) | 14 (21) | 0.137 |
| Smoking (%) | 34 (41) | 18 (26) | 0.056 |
| Diastolic dysfunction | 0.097 | ||
| Grade 1 (%) | 62 (74) | 54 (79) | |
| Grade 2 (%) | 19 (23) | 12 (18) | |
| Grade 3 (%) | 3 (4) | 2 (3) | |
| Aortic valve diagnosis | 0.102 | ||
| ISAS (%) | 53 (63.1) | 47 (69.1) | |
| MAVD (%) | 31 (36.9) | 21 (30.9) | |
| Mortality % | 2 (2.4) | 11 (16.2) | < 0.02 |
BMI: body mass index; SPP: systolic pulmonary pressure; LVEF: left ventricular ejection fraction; ECT: extracorporeal circulation time; ACT: aortic clamping time; HT: systemic hypertension; T2DM: type 2 diabetes mellitus; ISAS: isolated severe aortic stenosis; MAVD: mixed aortic valve disease (stenosis and regurgitation). Comparison with t-test and Chi-square test.
Bivariate analysis by logistic regression showed that female sex (odds ratio [OR] 2.57 [95% confidence interval (CI) 1.33-4.96], p < 0.005), HT (OR 3.02 [95% CI 1.43-6.35], p < 0.004), BMI (OR 1.23 [95% CI 1.12-1.36], p < 0.001), left ventricular mass (OR: 1.02 [95% CI 1.00-1.04], p < 0.03), and the labeled valve size of the prosthesis (OR 0.81 [95% CI 0.66-0.99], p < 0.04) were factors associated with LCOS (Table 4). The multivariate model showed that only BMI was an independent risk factor to develop LCOS (OR 1.21 [95% CI 1.08-1.35], p < 0.001) (Table 4).
Table 4 Bivariate and multivariate analysis to evaluate the association with LCOS
| Variable | Bivariate OR (CI95%) | p | Multivariate OR (CI95%) | p |
|---|---|---|---|---|
| Female sex | 2.57 (1.33-4.96) | 0.005 | 2.07 (0.96-4.45) | 0.06 |
| HT | 3.02 (1.43-6.35) | 0.004 | 2.08 (0.93-4.66) | 0.07 |
| BMI (Kg/m2) | 1.23 (1.12-1.36) | < 0.001 | 1.21 (1.08-1.35) | < 0.001 |
| Left ventricular mass (grs/m2) | 1.02 (1.00-1.04) | 0.03 | 1.01 (0.99-1.03) | 0.31 |
| Labeled valve size | 0.81 (0.66-0.99) | 0.04 | 0.84 (0.66-1.07) | 0.16 |
OR: odds ratio; CI: confidence interval; HT: systemic hypertension; BMI: body mass index.
Discussion
This study shows that in patients with SAS, a high BMI, are a risk factor associated with LCOS in the post-operative period of AVR, increasing the risk by 21% for each BMI unit above 25 kg/m2. LCOS is a serious complication following cardiac surgery22. In our study, LCOS was associated with a 16.2% death rate, compared to 2.4% in patients who did not develop this syndrome, p < 0.02. Several predictive factors for LCOS have been studied10,23,24 but little attention has been given to O/O as predictors. To answer this question, we eliminated from the analysis patients with confounding variables (those already recognized as risk factor for LCOS), except for diabetes and HT, the latter, due to its frequent association with aortic stenosis. In the present study, all the patients had normal baseline left ventricular ejection fraction; however, with this apparently favorable scenario, the overall incidence of LCOS was 44.7%. We then analyzed the pre-existing and the intermediate variables that could correlate with this high incidence, such as aortic clamping time, extracorporeal circulation time or left ventricular mass (due to the probability of differences for myocardial preservation during the time of ischemia), and without identifying statistic differences. In a previous report in which our group studied similar groups of patients with SAS; we found an incidence LCOS of 41%25. In the literature, there are reports of other investigations that show a wide range of incidence of LCOS being between 3 and 45%10-26; we think that this wide incidence is consequence of different criteria used to diagnose it.
Regarding HT, Lund et al.27 reported that the prevalence in patients with aortic stenosis increased with increasing BMI, being of 63% in their obesity group. We found a global prevalence of 68.4%, and 83% in the obesity group. The difference with Lunds study is that they only included patients with mild-to-moderate aortic stenosis, while in our study all the patients had SAS. However, our study agrees with the Lunds study27 in associating BMI with a higher prevalence of HT in the context of aortic stenosis.
Myocardial hypertrophy is a known risk factor for LCOS28, as HT and SAS have been causes associated with greater hypertrophy, this could predispose to inadequate myocardial preservation. We analyzed whether left ventricular hypertrophy alone was associated with LCOS; however, the multivariate model did not show statistical significance. In another similar study, the authors also did not find that HT was associated with the syndrome10.
Regarding the size of the implanted prosthesis, the mean in this study was 21.5 ± 1.6 mm, without statistical difference between groups (p = 0.94). A method to calculate the prosthesis to be placed, is to use the body surface area m2 (BSA m2)29, with this value, investigators30 showed that their group of SAS, had BSA higher than that observed in our population (2.06 vs. 1.77 m2, respectively), which can explain the smaller valve size in our population. Finally, we also analyzed the relationship between prosthetic valve size, BMI, and the presence of LCOS using multivariate analysis, and we did not find that valve size was an independent risk factor associated with LCOS. Maganti et al.10 found that a small size of the prosthesis emerges as a predictor of mortality with OR 1.3; however, it is not a predictor of LCOS as such.
We observed that the patients who developed LCOS had higher mortality at 30-days, which was 16.2% versus 2.4% in the group that did not develop LCOS (p < 0.02). The previous studies have associated LCOS with morbidity and mortality10. Interestingly the Mariscalcos study18 found that obesity is associated with a low risk of mortality after cardiac surgery. Although this is a large study, which included 13 countries, it has several differences that make it not comparable with our population: first of all, that study includes patients one decade younger: 59 (18-67) years versus 67 ± 10 (60-74) years, respectively, second, 27% were women, while in our group women comprised 47.1% of the population; in third place, Mariscalcos study included all cardiac surgeries, the vast majority of which were coronary artery bypass surgery, but even lower risk procedures were included, such as right mini-thoracotomy for the mitral valve and trans-AVR, in their logistic regression analysis only Grade 3 obesity was associated as an independent risk factor for mortality following isolated valvular surgery, [OR 1.26 (CI 95% 1.01-1.58) p < 0.041], but not only were patients with SAS and AVR as in our group, in fact, valve surgery in general formed a low percentage of the total of their patients. For all the above, the result of supporting the paradox of obesity should be taken with reserve, this may apply to certain groups and ages, as our study which focused on patients with SAS and AVR, the results were different.
Clinical implications
LCOS is a dreaded complication of cardiac surgery, which increases morbidity and mortality. Other factors have been associated to its presentation, but the O/O has been little studied, in fact, there has been controversy between whether or not it is a risk factor. In our SAS group, it turned out to be a predictor for the development of LCOS and we consider that it is of vital importance to recognize them, as a risk factor to be able to use strategies that decrease their incidence, prospective studies will be necessary to confirm these observations.











 nueva página del texto (beta)
nueva página del texto (beta)


