Introduction
Cardiovascular diseases (CVDs) are the main cause of morbidity and mortality in the adult population, both in developed and developing countries1,2, since they represent about 30% of all deaths3,4 and about 50% of deaths associated with non-communicable diseases4. In addition, there are certain current trends that contribute to its increase, such as population growth or longer average life expectancy, and increased risk factors attributable to the characteristic lifestyles of industrialized cities5,6. Such is the case of Mexico, where a notable displacement of the population from rural to urban areas has occurred in the past decades, which, in turn, has led to changes in diet (promoting an atherogenic diet) and to sedentariness3,5.
CVDs integrate a group of conditions which find their origin in cardiac and blood vessel disorders and that entail a poor tissue blood supply due to a diseased vascular source. Among these, ischemic cardiomyopathy (IC) and cerebrovascular accidents (CVA) stand out, followed by systemic arterial hypertension (SAH) (also considered as an independent risk factor for other CVDs) and peripheral vascular disease (PVD)4,7. About 80% of the mortality associated with this group of non-communicable diseases is attributed to these entities4.
Regarding its etiology, it is considered multifactorial and complex, insomuch as factors inherent to the individual (e.g., physiological, biochemical, genetics, lifestyles and habits) and its environment (e.g., the urbanization and the community, in which its socioeconomic and cultural context develops) intervene synergistically in its genesis8,9. The underlying situation is atherosclerosis, which develops progressively over the years in a silent manner, so the onset of symptoms generally occurs at middle age, when the atherosclerotic process is already at an advanced stage10,11.
Nevertheless, evidence shows the appearance of early atherosclerotic detrimental changes11-13, as a result of the joint action of cardiovascular risk factors (CVRFs) which are present from early childhood, and therefore, there is a longer time of exposure to them (since the effects of unhealthy diets, sedentary lifestyle, childhood obesity, high blood pressure and elevated levels of LDL cholesterol on the arterial system are cumulative), which, in turn, leads to an increased risk of cardiovascular morbimortality in adult life11,14.
In addition, there is an association of individual and sociocultural aspects, such as exposure to tobacco smoke (passive smoking) and the tendency for CVRFs to continue until adulthood, inasmuch as some risk factors are determined by the behaviors or habits learned since childhood or adolescence15,16, while others are acquired during the initial years of adult life, as consequence of greater independence12,15,17.
CVRFs correspond to those biological signs, acquired habits and characteristics of the individual that are most frequently associated with the statistical risk to predispose the development of a CVD in the coming years18,19. CVDs are preventable if measures on these factors are taken, some of which are fortunately modifiable4,20; the World Health Organization (WHO) considers as CVRFs: systemic arterial hypertension, overweight, obesity, inadequate diet (atherogenic), dyslipidemia (hypercholesterolemia, hypertriglyceridemia, increased LDL cholesterol, and decreased HDL cholesterol), smoking, alcohol consumption, physical inactivity or sedentariness, male sex, age (men > 55 years, women > 65 years), family background and genetics, stress, diabetes mellitus, and the presence of another CVD5,8,21.
Although each CVRF represents an independent impact on health, the association of two or more risk factors in an individual is not uncommon, especially now as sedentary lifestyles predominate over the population22,23. The more risk factors are present in an individual, the likelihood of presenting CVD increases12,24, insomuch as they act in a synergistic way in its physiopathology20.
The seventh report of the Joint National Committee for the prevention, detection, evaluation, and treatment of arterial hypertension (JNC 7), as well as other guidelines, refers to CVRFs as major or independent and minor; likewise, modifiable and non-modifiable factors are recognized25,26 (Table 1).
Table 1 Major and minor risk factors for cardiovascular disease
| Major risk factors | Minor risk factors |
|---|---|
| Modifiable | Modifiable |
| - Systemic arterial hypertension | - Overweight and obesity |
| - Smoking | - Sedentariness |
| - Dyslipidemia | - Atherogenic diet |
| - Diabetes mellitus or other CVD | - Alcohol consumption |
| Microalbuminuria or GFR < 60 mL/min | - Stress |
| Non-modifiable | Non-modifiable |
| Age (men > 55 years, women > 65 years) | Late CVD family background (men > 55 years, women > 65 years) |
| - Male sex | |
| Premature CVD family background (men < 55 years, women < 65 years) |
CVD: cardiovascular disease; GFR: glomerular filtration rate26,27.
Behavioral risk factors, such as smoking, unhealthy diets and physical inactivity, depict by themselves about 80% of the causes that lead to a cardiovascular complication,4,27 so that the efficiency in the prevention of CVDs depends on the adequate knowledge about CVRFs5.
Most studies on CVRFs (as well as the strategies on prevention, detection, and treatment of CVDs) have focused their attention on children, adolescents, the elderly28 and mainly on adults of mature age (particularly those aged over 40 years)11,28; on the contrary, those which analyze specifically the individuals who are at the beginning of adulthood (18-25 years) are scarce so far15.
Some research carried out in different countries (Mexico, Argentina, Chile, Spain and Venezuela)18, consistently reveals an increase in the incidence of CVRFs in young populations; these studies are striking since they argue that the cardiovascular risk profile in young people may be different to the one found in adults, as they might develop a CVD in the absence of classic CVRFs5,9,18.
By demonstrating that CVDs can manifest from these ages, a field of research on CVRFs affecting these age groups is exposed, inasmuch as it is important to study the relationship between the pathogenesis of CVDs and the lifestyle of young adults (who are not exempt)2,18. Prospective studies have shown that the presence of abnormal blood pressure levels in young patients has a direct association with the development of CVD in future29.
When considering the results obtained from the National Health and Nutrition Survey conducted in Mexico in 2016 (Encuesta Nacional de Salud y Nutrición, ENSANUT 2016), it was observed that 5.4% of young adults aged from 20 to 29 years suffered from systemic arterial hypertension30. On the other hand, in the last census of the National Institute of Statistics and Geography (Instituto Nacional de Estadística y Geografía, INEGI), carried out in 2015, it was reported that 16.6% of its Mexican inhabitants corresponded to the population aged between 20 and 29 years31. Correlating this data with the results provided by ENSANUT 2016, it could be estimated that about 1.07 million young adults in Mexico suffered from systemic arterial hypertension and among these, only around 53.78% knew it31.
Thus, the identification of CVRFs within a population of young adults enables to determine their susceptibility and to route the development of preventive measures, as they are subjects in which the modification of harmful behaviors and habits is attainable, with the aim of promoting healthy lifestyles to reduce the risk (or to delay the development) of cardiovascular origin conditions1,18,32.
Materials and Methods
A cross-sectional, descriptive and observational study was conducted in a population
integrated by 1066 university students from the Faculty of Chemistry of the
Autonomous University of the State of Mexico (Facultad de Química de la
Universidad Autónoma del Estado de México, UAEM), within the range from
18 to 25 years old, during the period from October 2018 to June 2019, from which a
representative, simple and random sample was selected, using the following formula
for finite populations  . As a result, a sample of 283
university adults was integrated, to which an additional 10% was added, considering
the possible losses, and a total of 311 apparently healthy participants (without the
presence of pre-existing cardiovascular or metabolic disease) with Mexican
nationality were obtained, all of whom granted their informed consent. A
questionnaire structured in five sections evaluating: (1) characteristics of the
diet, (2) characteristics of physical activity, (3) consumption of tobacco and
alcohol, (4) level of stress, and (5) familiar background of CVDs, was applied to
this sample.
. As a result, a sample of 283
university adults was integrated, to which an additional 10% was added, considering
the possible losses, and a total of 311 apparently healthy participants (without the
presence of pre-existing cardiovascular or metabolic disease) with Mexican
nationality were obtained, all of whom granted their informed consent. A
questionnaire structured in five sections evaluating: (1) characteristics of the
diet, (2) characteristics of physical activity, (3) consumption of tobacco and
alcohol, (4) level of stress, and (5) familiar background of CVDs, was applied to
this sample.
This questionnaire was based on the validated instruments corresponding to ENSANUT 2016 from the Mexican National Institute of Public Health (Instituto Nacional de Salud Pública, INSP)33, the International Physical Activity Questionnaire IPAQ34, the Global Adult Tobacco Survey,35 and the Alcohol Use Disorders Identification Test36, both from the WHO, as well as the Work Stress Test of the Mexican Institute of Social Security (Instituto Mexicano del Seguro Social, IMSS)37. Subsequently, each of the participants was scheduled an individual appointment to determine their levels of blood pressure, weight, height, body mass index (BMI), abdominal and hip circumference, and waist-to-hip ratio (WHR).
The obtained results were collected in frequency tables for further statistical analysis, which, in turn, was represented as tables and bar graphs, showing the absolute and relative frequencies of each of the variables. For this purpose, the Microsoft Office Excel Professional Plus 2016 and Microsoft Office Power Point Professional Plus 2016 software were used.
Results
The questionnaire was applied to a sample of 311 young Mexican university-level adults, who were subsequently scheduled an individual appointment for the measurement of anthropometric and blood pressure values. To this appointment, only 198 university students attended (67 men = 33.8% and 131 women = 66.2%), due to the fact that some of them were either working on final projects or studying for exams and were not able to show up (even after one phone call reminder and granting a second opportunity to attend an open appointment), so the final sample was reduced to that number. The established age range was from 18 to 25 years old, with an average of 19.7 years.
In 46% of the subjects, an atherogenic diet was identified, being more predominant among males (49.2%) than females (44.3%). Although 47% of the sample consumes fruits from 5 to 7 days/week, 73.2% consume only one or two out of the five recommended servings per day. Regarding the consumption of fast food, 68.2% reported doing it from 1 to 2 days a week and 16.7% does so from 3 to 4 times a week. Meanwhile, 48.5% consume soda from 1 to 2 days/week and 13.6% up to 4 days/week.
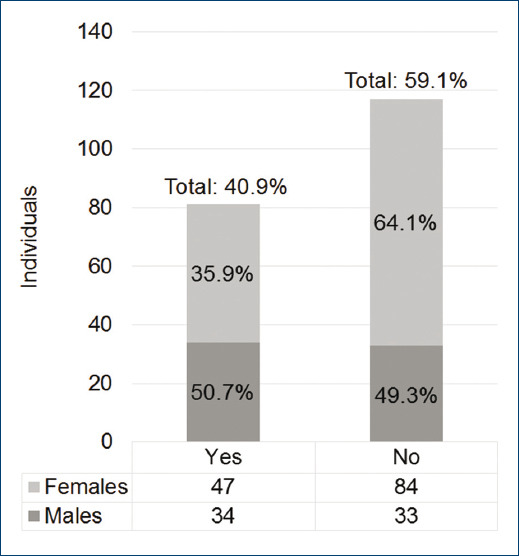
As for the level of physical activity, 40.9% of the sample reported they carried out moderate or intense physical activity in the past 6 months, while 59.1% of the subjects would be classified as sedentary (Fig. 1), being higher the level of physical inactivity among women (64.1%) than men (49.3%). The main reasons why individuals affirmed not performing physical activity were the lack of time (43.9%), lack of interest (5.6%), in adequate urban spaces and insecurity (4.5%), as well as the lack of knowledge about what activities they could perform (5.6%). Concerning the time they usually spend in front of a screen (television, computer, videogames, cell phone, or electronic tablet), 41.9% allocate from 3 to 4 hrs a day.
On the subject of tobacco consumption, the results showed that 78.3% of individuals have never smoked, while 9% have quit smoking and 12.6% are currently smokers, who mostly consume about one or two cigarettes with a frequency of 1 or 2 times/week, with tobacco consumption being a little higher among women (13%) compared to men (11.9%). The age at which a greater frequency was observed about the beginning of tobacco consumption was at 17 years old.
With regard to alcohol consumption, 64.1% asserted that they usually consume alcoholic beverages, with higher consumption among men (76.2%) than between women (58%); however, most of them refer doing it only 1 or 2 times/month, consuming from 1 up to 4 drinks per occasion (Table 2).
Table 2 Tobacco and alcohol consumption according to sex
| Variables | Males | Females | Total | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 67 | 33.8 | 131 | 66.2 | 198 | 100 | |
| Tobacco consumption | ||||||
| Smoker | 8 | 11.9 | 17 | 13 | 25 | 12.6 |
| Non-smoker | 51 | 76.2 | 104 | 79.4 | 155 | 78.3 |
| Ex-smoker | 8 | 11.9 | 10 | 7.7 | 18 | 9 |
| Alcohol consumption | ||||||
| Yes | 51 | 76.2 | 76 | 58 | 127 | 64.1 |
| No | 16 | 23.8 | 55 | 42 | 71 | 35.9 |
Regarding the stress level, it was found that in 32.8% of individuals, it can be classified as medium, highlighting that frequently (or relatively frequently) they manifest inability or difficulty to get to sleep, headaches, indigestion and gastrointestinal discomfort, increased tendency to eat, drink or smoke more than usual, muscle tremors or nervous tics, as well as a constant sensation of fatigue or exhaustion.
With regard to genetic factors and family history, 91.4% of the subjects have a family background of CVD (and other associated conditions), the most frequent being diabetes mellitus (71.2%), systemic arterial hypertension (64.6%), and overweight or obesity (56.6%). In turn, 44.4% of the individuals reported having from 3 to 4 antecedents of CVD in their family history, 36.4% referred from 1 to 2, and 11.1% mentioned more than 5. Moreover, 5.5% and 1.6% of the sample had a premature and late family history of acute myocardial infarction, respectively.
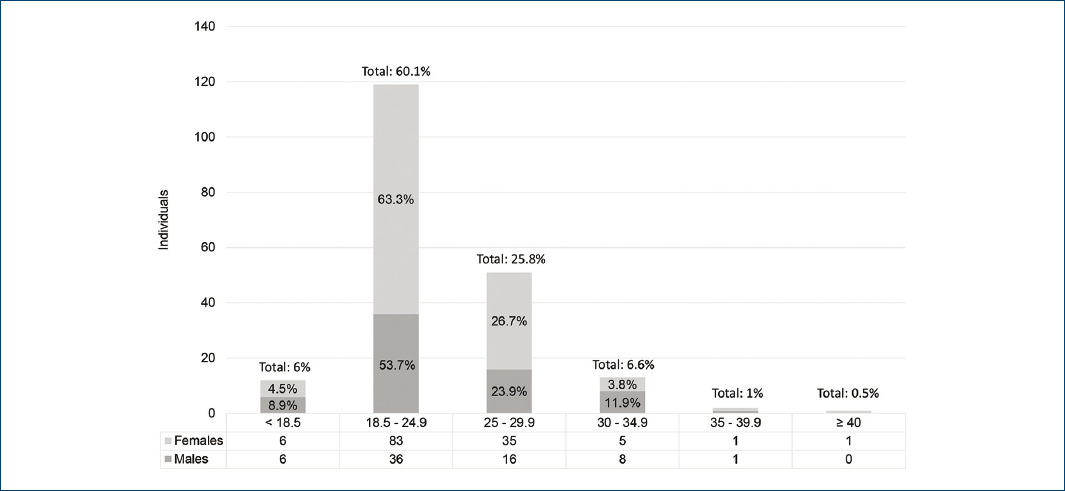
After obtaining the BMI of each of the participants, it was determined that 60.1% of them presented normal weight, 25.8% suffered from overweight (slightly more frequent among women than among men), and 8% from obesity (mostly observed in males) (Fig. 2). Besides, high values of abdominal circumference were found in 57.6% of the individuals, being higher among women (65.6%) than among men (47.8%). As for WHR, high values were recorded in 49% of young adults, with a clear predominance among women (64.1%) over men (19.4%).
The systolic blood pressure levels were normal (≤ 120 mmHg) in 71.2% of the individuals, while 15.2% presented high values (121-129 mmHg) and 13.6% reflected a number above 130 mmHg. As for the diastolic blood pressure, 81.8% of the subjects had levels ≤ 80 mmHg, 10.1% had levels between 80 to 89 mmHg, and only levels > 90 mmHg were observed in 3%. The mean arterial blood pressure was normal (≤ 93 mmHg) in 82.3% of the subjects, whereas in 17.7%, it was found to be high (> 93 mmHg). It is worth mentioning that it was men in whom a greater proportion of alterations in blood pressure levels was noticed.
Hence, the main CVRFs found correspond to family history of CVD, sedentariness, atherogenic diet, stress, and overweight. On the other hand, the risk factors which presented a lower rate were alcohol consumption, smoking, high blood pressure and obesity (Table 3).
Table 3 Main cardiovascular risk factors findings according to sex
| Cardiovascular risk factors | Males | Females | Total | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| 67 | 33.8 | 131 | 66.2 | 198 | 100 | ||
| Major | Modifiable | ||||||
| Systemic arterial hypertension | 11 | 16.4 | 6 | 4.6 | 17 | 8.6 | |
| Smoking | 8 | 11.9 | 17 | 13 | 25 | 12.6 | |
| Non-modifiable | |||||||
| Premature CVD family background* | 6 | 8.9 | 5 | 3.8 | 11 | 5.5 | |
| Minor | Modifiable | ||||||
| Overweight | 16 | 23.9 | 35 | 26.7 | 51 | 25.8 | |
| Obesity | 9 | 13.4 | 7 | 5.3 | 16 | 8 | |
| Sedentariness | 33 | 49.2 | 84 | 64.1 | 117 | 59.1 | |
| Atherogenic diet | 33 | 49.2 | 58 | 44.3 | 91 | 46 | |
| Alcohol consumption | 51 | 76.1 | 76 | 58 | 127 | 64.14 | |
| Stress | 22 | 43 | 32.8 | 32.8 | 65 | 32.8 | |
| Non-modifiable | |||||||
| Late CVD family background** | 17 | 25.4 | 14 | 10.7 | 31 | 1.6 | |
| Genetic factors and other family background of CVD***. | 59 | 88 | 122 | 93.1 | 181 | 91.4 | |
CVD: cardiovascular disease
*Premature CVD family background: male relatives < 55 years and female relatives < 65 years.
**Late CVD family background: male relatives > 55 years and female relatives > 65 years.
***Systemic arterial hypertension, cerebrovascular accident, diabetes mellitus, overweight or obesity, atherosclerosis, peripheral vascular disease, familial hypercholesterolemia.
Discussion
Among the main findings of this study on CVRFs, carried out in a population of young Mexican university-level adults, a high family background burden was found, reinforced in turn by an insufficient physical activity, an atherogenic diet, a high level of stress, and a significant frequency of overweight. Even though some differences were perceived (both subtle and notable) in the incidence of certain factors between both sexes, the general risk outlook between women and men was similar.
Genetic factors and family background stood out since they were present in 91.4% of individuals, in whom diabetes mellitus, systemic arterial hypertension, and overweight or obesity emerged as the most frequent antecedents for CVD. Likewise, it was observed that most of the subjects presented from 2 up to more than 5 associated antecedents, which could mean an increase in the risk of suffering these or other CVD, inasmuch as there was also a strong relationship between the number of antecedents presented by each individual, with the alteration of their anthropometric parameters and blood pressure levels. This suggests a strong family correlation, either due to the implication of intrinsic genetic factors, or to the instructed customs and reinforced habits in the household, or a confluence of both situations.
Regarding the level of physical activity, more than half of the sample (59.1%) was classified as sedentary, because the amount of physical activity they perform is insufficient to maintain an optimal energy balance, indicating as the main reason the lack of time (43.9%), which could be attributed to the intense workload university students must meet. However, one factor that should be considered would be the amount of hours they spent in front of a screen (television, computer, videogames, cell phone, or electronic tablet) since at least 41.9% allocates from 3 to 4 hrs daily. When taking sex into account, it was women (64.1%) in whom a higher level of physical inactivity was observed, which is a common finding with other studies conducted in Chile16,32 and in Spain1,17.
This situation is aggravated when considering that 46% of the subjects (mainly males) follow an inadequate diet, which propitiates the atherogenic process, forasmuch as the consumption of food that provides an adequate nutritional intake is insufficient in comparison with the high consumption of refined sugars and saturated fats from another group of food for which individuals tend to opt more frequently, perhaps due to the university lifestyle and family customs.
Furthermore, 32.8% of this population of young adults reported being subjected to a medium level of stress, with the perception of stress being equivalent between women (32.8%) and men (32.8%). It is worth mentioning that the studied individuals noticed an increase in other cardiovascular risk behaviors associated with stress, such as the tendency to overeat, smoking, and alcohol consumption, in an attempt to reduce the sensation of stress in the organism. Despite the mechanisms through which stress is implicated as a CVRF are not fully understood, it is known that in a stressful situation, the adrenergic system is constantly stimulated, which is enough to increase blood pressure and produce endothelial harm9,20.
When contemplating that a large majority of the subjects have a significant family history of diseases (present exclusively or in association), as well as the sedentariness categorized in more than half of the sample, and the important percentage of individuals who follow an atherogenic diet, a relationship between these factors with the alterations found in the samples anthropometric values could be established. These results are comparable with other studies carried out in Spain1 and in Peru19, in which it is also indicated that sedentary lifestyle affects women most of the time, with direct effects on their abdominal circumference and BMI. Nonetheless, men were not exempt from anthropometric abnormalities, given that 8% of the people in whom obesity was identified, a subtle majority was integrated by males, in whom alterations in abdominal circumference (47.8%) and in the WHR (19.4%) were also found, although in a smaller proportion.
In those subjects in whom blood pressure levels above the normality parameters were detected (9% and 14.4% of individuals with values corresponding to prehypertension and hypertension, respectively) and who were mostly males (16.4% with the first condition and 31.34% with the second one), it was observed a relationship with the referred record of antecedents of CVD in the family background and with alterations in the values of BMI, abdominal circumference, and WHR, which altogether could increase the rate of CVDs.
Despite the fact that drug addiction constitutes a relevant CVRF, smoking was not considered as a transcendent finding in this sample. On the contrary, alcohol consumption had a higher incidence (64.1% of the subjects, with a higher proportion of males and with similar results in another study carried out in Chile)32, with a consumption of one up to four drinks with a frequency from 1 to 2 times/month.
In this sample, it was appreciated that habits and lifestyles can be established and even reaffirmed during youth. Therefore, if there is no emphasis on the modification of these patterns, that is, if behaviors such as sedentariness or consumption of alcohol and tobacco prevail, coupled with a poor diet quality and a strong genetic and family component, those individuals with normal weight could get into to the group of subjects with overweight and obesity, and those in whom any of these conditions were detected during the study, could aggravate their situation, and suffer a CVD with greater target organ damage from earlier stages. If this path continues, the impact will not be limited to the individuals health, but could eventually affect the economic activity of the country since the young population will be ill in their productive years18.
The main limitation of this study consisted of the impossibility to analyze biochemical variables, with the aim of assessing serum parameters such as HDL and LDL cholesterol, triglycerides, and glucose, which would have enriched the results by being useful in the measurement of vascular age with the QRISK algorithm, stratifying cardiovascular risk with the Framingham score and establishing criteria for the diagnosis of metabolic syndrome or diabetes mellitus. Nonetheless, in other similar studies carried out in Brazil22, Cuba38, India2, and Mexico15, in which biochemical variables were taken into account, alterations such as dyslipidemia (characterized by high levels of LDL cholesterol and low HDL cholesterol and hypertriglyceridemia) and abnormal serum levels of glucose were identified in young individuals in whom, in turn, the confluence with other CVRFs (such as sedentary lifestyle, overweight, and obesity) was observed. This information suggests that alterations in these biochemical variables could also be found in the individuals who took part in the sample of this study.
Conclusions
The main CVRFs identified in this sample of young Mexican adults correspond to a high hereditary and family background of CVD burden, aggravated in turn by an insufficient level of physical activity (with higher incidence among women), an atherogenic diet (more frequent among males), a high level of stress, and a significant frequency of overweight (mostly women). The cases in which high blood pressure was detected were mostly males, showing a relationship with the referred record of antecedents of CVD in the family background and with alterations in their anthropometric values. Smoking was not considered a transcendent finding in this sample; on the contrary, alcohol consumption had a higher incidence, especially among males.
According to the categorization of CVRFs, the most frequently identified findings correspond to the group of modifiable minor risk factors, which could allow the development of preventive measures, inasmuch as they are subjects in which the modification of harmful behaviors and habits is achievable since they find themselves at a timely moment in which they own sufficient autonomy to take responsibility for their self-care.
Thus, further development of analytical research articles about CVRFs and CVDs in these age range (for which this study could serve as baseline) should be considered.











 nova página do texto(beta)
nova página do texto(beta)