Heart surgery post-operated (POP) patients are a population of medical-surgical care with characteristics of their own according to the type of procedure they undergo since during the surgery they are assisted with a cardiopulmonary bypass pump, they require blood transfusions and are likely to experience inherent acute cardiopulmonary complications in the trans-operative period1. Furthermore, they need invasive and non-invasive hemodynamic surveillance, and their hemodynamic profile generally has to be determined under sedation and mechanical ventilation in the early post-operative period1,2.
Their evolution in the early POP period in a post-operative cardiovascular intensive care unit (PCICU) can be uneventful or with acute complications, such as low cardiac output syndrome2, pulmonary congestion (pulmonary edema, extravascular lung water [EVLW]), or cardiogenic shock of diverse origins requiring further intervention, such as administration of drugs with inotropic activity, counterpulsation balloon, or even extracorporeal membrane oxygenation (ECMO), which implies further impairment of their hemodynamic behavior1-5.
In the PCICU, hemodynamic profile is determined by the thermodilution method with a flotation catheter in the pulmonary artery (Swan-Ganz) and the presence of EVLW through chest X-ray and thermodilution5-7. Cardiopulmonary evaluation can be complemented with lung ultrasound (L-US), which is also a tool that can calculate the presence of EVLW and support its evolution with specific treatment8. In patients undergoing a heart surgery procedure, the number of B-lines has been associated with the amount of EVLW9.
However, the hemodynamic profiles that can occur after heart surgery can be diverse, although not all of them occur in a single patient; for this reason, L-US imaging could be different depending on the category of the hemodynamic profile obtained at admission or within the 1st 12-24 h of PCICU stay. For this reason, an exploratory examination of the possible images that would result according to the hemodynamic profile in the early post-operative period of heart surgery is carried out.
Figure 1. Lung ultrasound and chest X-ray correlation according to the hemodynamic profile in heart surgery post-operated patients. In 1A, anteroposterior X-ray with portable equipment is shown, without evident radiographic alterations, which is indicative of a patient without lung compromise. In 1B, lung ultrasound reveals the bat sign, the pleural line, and A-lines indicative of normal lung; hemodynamic pattern without alterations by cardiac index (CI) and normalized left ventricle filling pressures (pulmonary capillary pressure, PCP). In 2A, anteroposterior X-ray shows an increase in bronchovascular bilateral weave, flow cephalization, left costodiaphragmatic effacement, with a hemodynamic pattern, increased PCP, and pulmonary congestion. In 2B, lung ultrasound identifies the bat sign, the pleural line, and B-lines suggestive of alveolar-interstitial syndrome due to pulmonary congestion, in addition to a hemodynamic pattern with normal CI and increased PCP and acute pulmonary edema. In 3A, anteroposterior X-ray shows no apparent lung involvement. In 3B, anteroposterior lung ultrasound reveals the presence of bat sign, pleural line, and A-lines consistent with normal or dry lung, in addition to hemodynamic pattern with normal CI and low PCP due to hypovolemic shock. In 4A, anteroposterior X-ray indicates bilateral bronchovascular weave increase, interstitial occupation, and effacement of both costodiaphragmatic angles. In 4B, pulmonary ultrasound recognizes the bat sign, the pleural line, and B-lines indicative of alveolar-interstitial syndrome due to pulmonary congestion, together with hemodynamic patterns with low cardiac index and filling pressures (PCP) elevation due to cardiogenic shock.
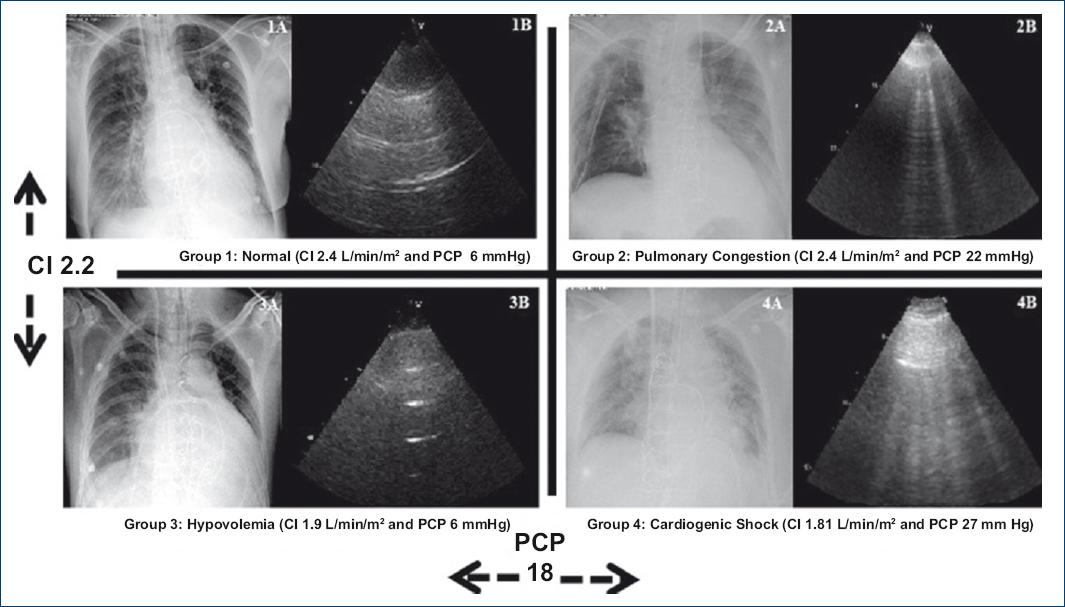
Figure 1 Lung ultrasound and chest X-ray correlation according to the hemodynamic profile in heart surgery post-operated patients. In 1A, anteroposterior X-ray with portable equipment is shown, without evident radiographic alterations, which is indicative of a patient without lung compromise. In 1B, lung ultrasound reveals the bat sign, the pleural line, and A-lines indicative of normal lung; hemodynamic pattern without alterations by cardiac index (CI) and normalized left ventricle filling pressures (pulmonary capillary pressure, PCP). In 2A, anteroposterior X-ray shows an increase in bronchovascular bilateral weave, flow cephalization, left costodiaphragmatic effacement, with hemodynamic pattern, increased PCP and pulmonary congestion. In 2B, lung ultrasound identifies the bat sign, the pleural line, and B-lines suggestive of alveolar-interstitial syndrome due to pulmonary congestion, in addition to a hemodynamic pattern with normal CI and increased PCP and acute pulmonary edema. In 3A, anteroposterior X-ray shows no apparent lung involvement. In 3B, anteroposterior lung ultrasound reveals the presence of bat sign, pleural line, and A-lines consistent with normal or dry lung, in addition to hemodynamic pattern with normal CI and low PCP due to hypovolemic shock. In 4A, anteroposterior X-ray indicates bilateral bronchovascular weave increase, interstitial occupation and effacement of both costodiaphragmatic angles. In 4B, pulmonary ultrasound recognizes the bat sign, the pleural line and B-lines indicative of alveolar-interstitial syndrome due to pulmonary congestion, together with hemodynamic pattern with low cardiac index and filling pressures (PCP) elevation due to cardiogenic shock.
Herein, the behavior of the different hemodynamic profiles according to Forrester-Diamond-Swan classification (which correlates the magnitude of cardiac index and pulmonary capillary pressure with four possible profiles) in cardiac surgery post-operated patients is described; figure 1 shows the correlation of L-US and chest X-ray obtained with a portable device for these same categories:
– Class 1: Normal profile (cardiac index [CI] > 2.2 L/min/m2; pulmonary capillary pressure [PCP] <18 mmHg). Seventy-one-year-old female patient, post-operated of mitral valve exchange with biological prosthesis plus tricuspid valve plasty; hemodynamic profile at PCICU admission: CI of 2.4 L/min/m2; and PCP of 14 mmHg, stable evolution and extubation at 48 h (Fig. 1A and B).
– Class 2: Profile consistent with pulmonary congestion (CI >2.2 L/min/m2; PCP > 18 mmHg). Eighty-four-year-old male patient, post-operated of aortic valve replacement by biological prosthesis plus mitral plasty with a rigid ring; complicated with vasoplegic syndrome requiring intensive fluid resuscitation and use of high-dose vasopressors (at the moment of the images, water balance was positive: 9,600 cm3); hemodynamic profile at PCICU admission: IC of 2.4 L/min/m2 and PCP of 22 mmHg; left ventricle (LV) ejection fraction was normal (Fig. 2A and B).
– Class 3: Profile consistent with hypovolemia (CI < 2.2 L/min/m2 and PCP < 18 mmHg). Forty-six-year-old male patient, post-operated of mitral valve plasty with a rigid ring who had more than usual bleeding (1000 cm3 in 2 h). Hemodynamic profile at PCICU admission: CI of 1.9 L/min/m2 and 9-mmHg PCP; LV ejection fraction of 45% (Fig. 3A and B).
– Class 4: Profile consistent with cardiogenic shock (CI < 2.2 L/min/2 and PCP > 18 mmHg). Sixty-five-year-old female patient, post-operated of a coronary artery bypass graft procedure with left mammary artery to anterior descending artery and left radial artery to first right ventricular branch, who experienced peri-procedural infarction, with new LV hypokinesia on anterior aspect and apex; hemodynamic profile at PCICU admission: CI of 1.81 L/min/m2 and PCP of 27 mmHg; LV ejection fraction of 25%. Double inotropic regimen and intra-aortic balloon pump counterpulsation were required (Fig. 4A and B).
As it can be observed in the hemodynamic profiles, chest X-ray, and L-US, PCP increase-related pulmonary congestion1,3,10 is a regular event and, actually. it reflects the conditions LV end-diastolic pressure is even in cardiac procedure post-operated patients.
A 3rd day of heart surgery, L-US has been shown to detect complications such as pulmonary congestion (p = 0.043), atelectasis (p <0.001), pneumothorax, pleural effusion (p = 0.013), and consolidation11 earlier and in larger quantities.
Furthermore, in other clinical scenarios, the presence of EVLW (pulmonary edema, pulmonary congestion) has been linked to decompensation and mortality in acute heart failure8.
It should be pointed out that, despite these and other evidences, when PCP has been tried to be correlated with L-US-defined EVLW, it has been low4 in the studied population.
It should be noted that L-US does not differentiate by itself between cardiogenic and of non-cardiogenic origin acute edema (EVLW, pulmonary congestion)12, and for this reason, both have received the name of the alveolar-interstitial syndrome, with its sonographic translation being B-lines.
B-lines are formed due to different acoustic impedance produced by the pulmonary water-air interface and cause reverberation that on the screen can be seen in the form of vertical lines referred to as comet tail pattern. As the balance between interstitial water increases and alveolar air decreases, the interlobular septum thickens. The alveoli are filled with fluid and this results in the appearance of multiple diffuse B-lines5-7. With L-US, sensitivity and specificity have been reported to be 93.4% and 93%9, respectively.
It is important mentioning that EVLW (pulmonary edema or pulmonary congestion), of cardiogenic or hydrostatic origin, is associated with an imbalance of the Starling mechanisms that favor the increase of water in the interstitial space. Those in charge of moving excess EVLW are the lymphatics, which are identified on chest X-ray as Kerley B-lines when they are engorged. When this mechanism is insufficient, alveolar fluid appears7,8,10,12.
Cardiac surgery POP patient is subjected to cardiogenic and non-cardiogenic mechanisms that are complicated by EVLW2; in this context, the sequence of episodes can be different for the presence of EVLW, which might explain the possible lack of correlation between PCP and EVPW in other studies4.
In the absence of other cardiopulmonary complications and PCP elevation, at least at stages 1 and 3, the lung is free of EVLW; not so for Forrester-Diamond-Swan stages 2 and 4, where it is shown by chest L-US and X-ray with portable equipment; the obtained images are highly indicative of EVLW.











 nueva página del texto (beta)
nueva página del texto (beta)


