Introduction
In adults, sudden cardiac arrest (SCA) is one of the main signs of heart disease, with symptomatic or asymptomatic ischemic heart disease are considered to be the cause of most cases1-3. SCA occurs when the heart suddenly and unexpectedly stops pumping blood; the victim loses the state of alertness, has no signs of circulation and only gasps; without treatment, this abnormality leads to sudden death (SD). Some individuals with SD may have previous symptoms, such as chest pain, dyspnea, syncope, pre-syncope, or seizures, but often they go unnoticed4. SD is also suspected in people who had been seen alive within a period not longer than 24 h and then were found lifeless in the absence of an obvious cause of death, such as those cases identified at dawn without an observer5,6. It is a public health problem worldwide7; SD is estimated to account for 30% of cardiac-origin mortality, and for 20% of deaths in adults8-10. The true incidence of SCA and SD is unknown, and there are variations according to the studied population; in China, Europe, and USA, 41, 86, and 155 cases have been reported per 100,000 population/year, respectively11-13. In the population younger than 35 years, an incidence of 1-3 cases/100,000 population/year is considered14, and at 75 years of age, 800 cases/100,000 population/year13,15. In 2015, 17.7 million of deaths associated with cardiovascular diseases were reported in the world16; 30% of these are likely to be due to SCA and SD, which can represent up to 5.31 million cases/year (Table 1).
Table 1 SD in adults worldwide, calculated causes, and survival
| Cardiovascular deaths worldwide/year (2015) | 17.7 million |
| SCA and SD/year (30% of cardiovascular mortality) | 5.31 million |
| Causes | |
| Ischemic heart disease | 60-80% |
| Cardiomyopathies (hypertrophic, dilated, valvular, etc.) | 20-40% |
| Primary arrhythmic disease | 1-2% |
| Detected arrhythmias | |
| Asystole | 40-50% |
| PEA | 30% |
| VF/PVT | 20% |
| Out-of-hospital cases | |
| At home | 70-80% |
| In public areas | 20% |
| Without observer | 50-60% |
| Overall survival | < 10% |
PEA: pulseless electrical activity; VF: ventricular fibrillation; PVT: pulseless ventricular tachycardia.
Causes according to age groups
The causes vary with regard to age groups; in people older than 25 years, symptomatic or asymptomatic coronary artery disease is the main cause9,10,14. From 20 to 40% of cases can be secondary to cardiomyopathies due to systemic arterial hypertension, obesity, diabetes, alcohol, as well as to idiopathic, valvular, congenital, infiltrative, non-compacted myocardial fibrosis, or heart failure6,8,10,13. Slightly more than 50% of adults with SCA and SD have no previous diagnosis of structural heart disease, only a high prevalence of cardiovascular risk factors, especially systemic arterial hypertension, diabetes mellitus, sedentary lifestyle, smoking, obesity, and dyslipidemia4-6. In few cases, SD is consecutive to primary arrhythmic disease in adults5,6. In those younger than 25 years, the main causes are hypertrophic cardiomyopathy, congenital anomalies of the coronary arteries, arrhythmogenic cardiomyopathy, and primary arrhythmic disease, such as Wolff-Parkinson-White syndrome, long QT syndrome, Brugada syndrome, short QT syndrome, catecholaminergic polymorphic ventricular tachycardia, and idiopathic ventricular fibrillation (VF)14,17. Unfortunately, the exact cause of death is unknown in most cases and only undergo verification by anatomopathological, histological, or toxicological examination; the diagnosis of cardiac-origin SD (CSD) is almost always a clinical approach, which overestimates the causes and the incidence18,19. A recent study of 525 people with CSD, with a mean age of 62.8 years and with 69% of males, identified non-cardiac-origin causes in 40% of cases (34%, drug overdose; 60%, opiates; 14%, neurological causes; 11%, infectious causes; 9% pulmonary embolism; and 7%, gastrointestinal bleeding)18. Another study of 1039 CSD victims with a mean age of 32 years (66% males), identified that 28% of cases were due to non-cardiac-origin causes (40%, pulmonary; 20%, infectious; 18%, cerebrovascular; and 8% other neurological diseases)19. Recently, the American Heart Association (AHA), the American College of Cardiology and the Heart Rhythm Society have recommended the performance necropsy studies in all SCA and SD victims, to confirm the diagnosis and find the exact causes of death20.
Causal arrhythmias
Over the years, the type of arrhythmias causative of a SD episode has changed; previously, VF and pulseless ventricular tachycardia (PVT) were recognized as the main origins, but currently, asystole, and pulseless electrical activity (PEA) are recorded more frequently10,13,20,21. VF and PVT appear to be the most common causes of SCA and SD in cases that occur away from home and in those related to physical activity13. In the general population, asystole has been found in 40-50%, PEA in 30% and VF/PTV in 20% of cases20.
Malignant arrhythmia substrates
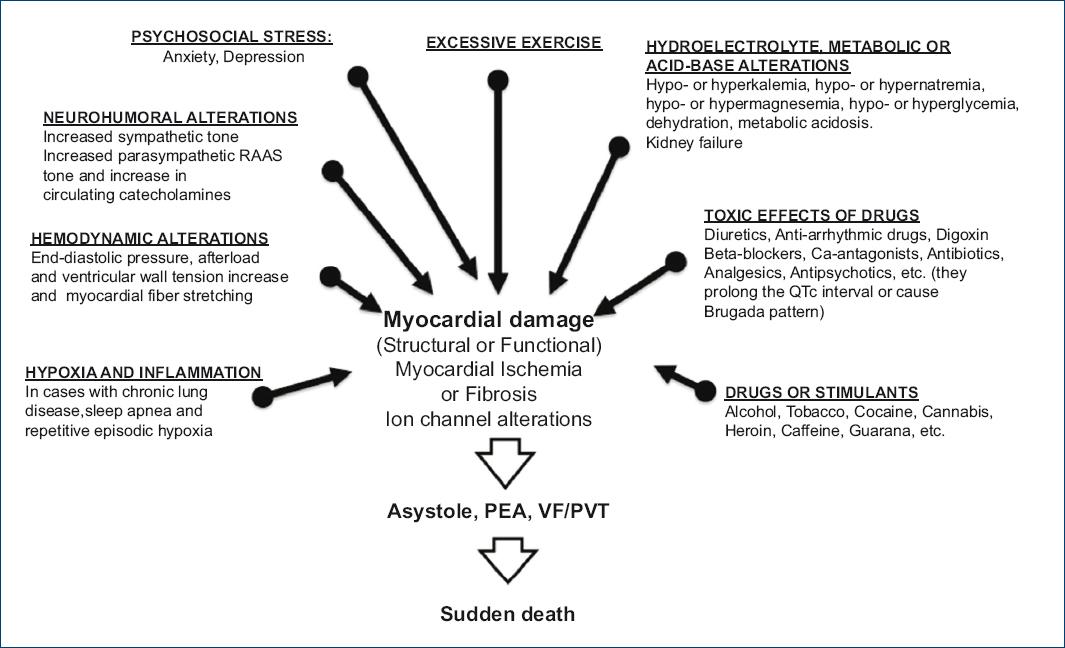
For malignant arrhythmias to occur, the participation of substrates and activators acting on the heart is required. The most important substrates are myocardial ischemia, myocardial fibrosis, and ion channel abnormalities (congenital or acquired)3,13,21. Myocardial ischemia favors the dispersion of refractory periods and the presence of activity in ventricular myocardial cells3,13; myocardial fibrosis gives rise to the development of ventricular reentry circuits22, and ion channel abnormalities, to ventricular depolarization and repolarization alterations23.
Malignant arrhythmia activators
In all SCA and SD victims, the participation of substances, drugs, or metabolic alterations that work as activators and that can be the origin of the episode should be ruled out. Malignant arrhythmia triggering factors that may be involved (Fig. 1) are various: (a) increased activity of the sympathetic and parasympathetic nervous system, of the renin-angiotensin system and increase in the number of circulating catecholamines6; (b) hemodynamic factors such as end-diastolic pressure, afterload, and left ventricle parietal stress elevation7; (c) hydroelectrolytic alterations such as hyponatremia, hypokalemia, hypocalcemia or hypomagnesemia6; (d) metabolic disturbances such as dehydration, acidosis, hyperglycemia, or hypoglycemia2; (e) hypoxia24; (f) iatrogenic factors secondary to the use of drugs such as diuretics, inotropics, vasodilators, anti-arrhythmic agents, or drugs that prolong the QT interval or favor the presence of Brugada pattern, such as some antibiotics, antipsychotics, or analgesics25; (g) drugs and addictive substances such as alcohol, tobacco, cocaine, cannabis, heroin, or LSD26; (h) energy drinks with high content of sugar, caffeine, guarana, and other stimulating substances27; (i) excessive exercise28, and (j) psychosocial stress, specially anxiety, and depression3.
Clinical characteristics and risk group
Based on SCA and SD victims clinical characteristics, the population is classified into three groups, as shown in table 2: group I, population with risk factors for ischemic heart disease, but without a diagnosis of the previous heart disease5,6,9,10; Group II, carriers of some structural heart disease1-3, chronic lung disease29, sleep apnea30 or kidney failure31; and Group III, survivors of a SCA episode or arrhythmic death high-risk carriers32. Symptomatic or asymptomatic myocardial ischemia is the most important risk factor for developing SCA and SD in adults1-3. In patients diagnosed with ischemic heart disease, those of the male gender, who are smokers and have persistent ST-segment elevation with frequent ventricular extra-systoles are at increased risk of SCA and SD33, as it occurs in patients in whom increased myocardial ischemia, myocardial fibrosis, or total occlusion of the coronary artery related to a heart attack have been detected6. Heart failure (HF) patients with left ventricular ejection fraction (LVEF) lower than 30% have a high risk of dying from SCA and SD34. LVEF as the only arrhythmic-origin SD predictor is insufficient; the Seattle classification helps recognize arrhythmic death high-risk carriers who can benefit from an automated implantable cardioverter defibrillator (AICD)35; figure 2 shows the clinical characteristics related to higher risk of SCA and SD and that confer higher possibility of response to the implantation of an AICD in patients with HF of ischemic or non-ischemic origin. Recently, the detection of ventricular myocardial fibrosis by magnetic resonance imaging in patients with HF of ischemic or non-ischemic origin has been shown to be a more efficient predictor to identify patients at high risk of arrhythmic death who may benefit from the use of an AICD36. Patients with chronic obstructive pulmonary disease have 2-3 times higher risk for developing cardiovascular diseases, arrhythmias and death37. The risk of SCA and SD is higher in those with chronic lung disease and frequent exacerbations of hypoxia episodes29. In individuals with obstructive sleep apnea syndrome, the presence of frequent episodes of apnea, hypopnea, and nocturnal hypoxia is associated with a higher incidence of SCA and SD38. Kidney damage increases the risk of SD, with up to 22% of deaths in these patients being due to SCA and SD39. Albuminuria is an early marker of kidney damage and an independent predictor of SCA and SD, which in addition increases its predictive value when linked to a glomerular filtration rate lower than 60 mL/min/1.73 m2,40.
Table 2 SCA and SD victims clinical characteristics.
| Group | Characteristics |
|---|---|
| Group 1 | General population with risk factors for ischemic heart disease such as: Systemic arterial hypertension, diabetes mellitus, smoking, obesity, dyslipidemia, and sedentary lifestyle |
| Group 2 | Structural heart disease Ischemic, hypertrophic, dilated, valvular, congenital, infiltrative heart disease, non-compacted, arrhythmogenic cardiomyopathy, heart failure, abnormalities in the origin or trajectory of coronary arteries, and congenital heart diseases. Kidney failure, chronic pulmonary disease, or sleep apnea Primary arrhythmogenic disease Wolff-Parkinson-White, long QT, and Brugada syndromes, malignant early repolarization, catecholaminergic polymorphic VT (CPVT), and short QT syndrome |
| Group 3 | Subjects recovered from SCA or with a history of VF, VT, or syncope secondary to ventricular arrhythmias Idiopathic VT or VF |
Any patient in these groups is considered to be at higher risk and having a family history of SD should be a reason for more exhaustive examination.

Figure 2 Clinical characteristics according to the scale of Seattle and their relationship with the mode of death and response to an automated implantable cardioverter defibrillator in patients with heart failure of ischemic or non-ischemic origin (modified from Levy et al.33).
Symptoms before an episode of SCA and SD
There is evidence that, in children and adults with SCA, the previous symptoms are common41,42. In children, 26-33% of victims had some type of symptom, and in 45% of cases, symptoms had occurred even 40 days before the episode; the most common symptoms were chest pain, seizures of unknown causes, dyspnea, and syncope41. In adults, up to 50% of victims had previous symptoms and men suffered chest pain more often, while women experienced dyspnea42. Subjects with SCA who experienced symptoms and requested help or sought medical care before the event, significantly improved survival in comparison with those who did not ask for help (32% vs. 6%)42.
SCA treatment in the community
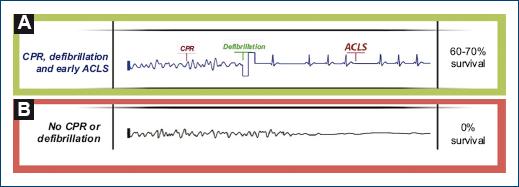
Specific treatment of a SCA victim includes cardiopulmonary resuscitation (CPR) maneuvers and the use of an automated external defibrillator (AED); table 3 shows the steps to follow for the care of SCA in the community. The earlier CPR is applied and AED used, the higher the survival likelihood of those affected by SCA43. In the cases of VF and PVT, which occur more frequently away from home13, early defibrillation highly significantly improves the survival rates (Fig. 3); when CPR is started and defibrillation is carried out within the first 2 min after SCA occurrence, survival rates of up to 71% can be achieved, with good neurological recovery. Within the 1st min, ventricular defibrillation success is higher than 90%, and it drops by 7-10%/min without CPR. The latter prolongs the time window for the possibility to perform successful defibrillation. The AHA CPR guidelines44, as well as studies in the general population, emphasize the importance for both the general public and health personnel to be trained and have the knowledge to perform high quality CPR and use an AED45. Exclusively manual compressions and the use of public access AED have been shown to be highly effective for improving SCA victims survival in the community46. There are important limitations for the treatment of people with SCA occurring at home, where most cases are recorded; the most commonly detected rhythms are asystole and PEA; the possibilities of early detection and treatment are reduced and treatment success is much lower than that achieved in cases with VF and PVT21. In Mexico, some cases of SCA victims survival have been reported, when the survival chain is properly implemented47, and the creation of a comprehensive care system for individuals with SCA is strongly recommended48.
Table 3 Sequence of steps for the care of the SCA victim in the community; manual-only CPR and use of public-access AED
| 1. Recognize the victim in cardiac arrest (suddenly
collapses, does not respond, does not breathe, is pale or livid).
2. Give notice to local emergency number (in Mexico, 911), request an AED, put the call on speaker for assistance. 3. Start compressions at the center of the chest, between the two nipples from 100 to 120 x’, 5 to 6-cm deep in adults and 4 to 5. cm in children, until AED or assistance arrival. 4. Quickly use the AED: – Open the AED and follow the instructions – Place the patches as directed, use pediatric patches in children younger than 8 years, do not touch the victim while the AED analyzes – If applying a discharge is necessary, the AED will indicate so – Warn: “Clear, nobody touch the victim”, before applying the discharge – Apply the discharge on the button that blinks 5. Restart compressions until the patient recovers, assistance arrives, or AED indicates |
Conclusions
SCA and SD are a global public health problem. Unfortunately, almost all cases occur in the general population, in out-of-hospital settings, at home and in people who were unaware of being heart disease bearers. True incidence and prevalence are unknown. Carrying out anatomopathological, histological and toxicological studies in all people with SD is advisable to find the exact cause of death, which will help the provision of better prevention measures. At present, the most commonly identified arrhythmias are asystole and PEA. Symptoms before a SCA occur in up to 33% of children and 50% of adults; when victims seek medical attention before experiencing the episode, survival is significantly improved. High-quality CPR and AED use are SCA initial treatment; in the cases of VF and PVT, AED early use substantially improves survival; health personnel and the general population should know and apply these measures. Favoring manual-only CPR and AED use programs in the community to reduce SCA mortality is advisable. Further research and prevention measures applied to the general population are needed to reduce the incidence of SCA and SD.











 nueva página del texto (beta)
nueva página del texto (beta)