Introduction
Cardiovascular disease in pregnant patients has an approximate prevalence of 1-4% and causes 10-15% of maternal mortality1,2. Gestation represents a pressure for the cardiovascular system, not only because of the 50% increase in blood volume and cardiac output but also due to cardiac structural changes, as well as vascular and metabolic modifications3. This explains the risk for decompensation and death in women with heart disease during pregnancy. In Colombia, 39% of maternal deaths are the result of indirect causes, i.e., those resulting from a condition established before pregnancy or that evolves during its course and that is not related to obstetric causes; of the total number of these indirect causes, 3.7% corresponds to heart disease4.
Given the specific epidemiological and sociocultural characteristics of the country5, the pattern of heart disease occurrence and its effect on maternal-fetal morbidity and mortality, assessing associated factors becomes essential to timely detect them.
Methodology
This was a observational, analytical, and retrospective cohort study with a non-probabilistic convenience sample. The sample consisted of 104 pregnant patients who were admitted to the obstetrics department of a high-complexity institution between January 1, 2010, and December 31, 2015, including patients with congenital or acquired heart disease, corrected or not, and with arrhythmias requiring urgent hospital treatment. Medical histories from both the mother and the newborn were reviewed using a case report form for the collection of information using the Microsoft Excel software, and the data were subsequently analyzed with STATA 13. A cardiologist, a neonatologist, and an obstetrician-gynecologist corroborated the cardiovascular, neonatal, and obstetric outcomes, respectively. Individuals with mild or moderate valve insufficiency, those with mild valve stenosis according to the 2017 European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines6 criteria and subjects who lacked an echocardiographic study or delivery information were excluded.
Variables taken from patient history included demographic data such as age, parity status, gestational age at first evaluation by the cardiology department and at delivery, habits (smoking and alcohol consumption), comorbidities according to current guidelines definitions (hypertension, diabetes mellitus, dyslipidemia, and other conditions that implied adopting chronic treatment), cardiovascular history (surgical or percutaneous cardiovascular interventions before pregnancy, heart disease, or complication before pregnancy), oxygen saturation at admission, presence of cyanosis, chronically consumed drugs, and with an emphasis on anticoagulants (indication, type, and follow-up). Regarding echocardiographic findings, left ventricle ejection fraction, presence or not of right ventricular dilatation, and type of detected heart disease were reviewed. The route of delivery was verified and, in case of cesarean delivery, whether the indication was obstetric or cardiac was reviewed.
Maternal-fetal and obstetric hospital outcomes were classified as follows:
Primary cardiac events: pulmonary edema, sustained symptomatic arrhythmia requiring treatment (tachyarrhythmia or bradyarrhythmia), stroke, cardiac arrest, or cardiac death.
Secondary cardiac events: deterioration of two or more New York Heart Association (NYHA) classes in comparison with baseline, need for urgent invasive cardiac procedure during pregnancy or in-hospital postpartum period.
Neonatal episodes: premature delivery (< 37 weeks of gestation), low weight for gestational age (lower than 10th percentile), respiratory distress syndrome, intraventricular hemorrhage, stillbirth (≥ 20 weeks of gestation), or neonatal death (up to postpartum day 28). In addition to neonatal episodes, the presence of abortion was investigated (< 20 weeks of gestation).
Obstetric episodes: non-cardiac maternal death, hypertensive disorder of pregnancy (HDP), and postpartum hemorrhage (> 500 mL in vaginal delivery or > 1000 mL in cesarean section).
Statistical analysis
Categorical variables are summarized in absolute and relative values, and for continuous variables, normality assumption was carried out with the ShapiroWilk test. Variables with normal distribution are summarized with averages and standard deviation, and variables that did not meet the normality assumption, with medians, and interquartile range. The outcome measure was a composite of cardiac, obstetric, and neonatal episodes. Univariate analysis was performed for the proposed risk variables using the Chi-square test, Fishers exact test, or the t-test for single samples and MannWhitneys U-test for continuous data. A wide spectrum of variables was considered (Table 1) to identify determinants of the proposed outcome; univariate analysis predictors (p < 0.25) were included in a multivariate analysis with a logistic regression model, and its discrimination capacity was determined with the area under the curve; after the logistic regression, a generalized linear model with logit function was constructed to compare the results of the two alternative methods and generate the same outcome prediction. The modified World Health Organization (mWHO) risk classification and its differentiation capacity were independently analyzed.
Table 1 Patient general characteristics
| Variable | n = 104 |
|---|---|
| Age in years, median (range) | 22 (15 40) |
| Number of previous pregnancies, median (range) | 2 (0 7) |
| Gestational age at delivery in weeks, median (range) | 34 (6 40) |
| Gestational age at first evaluation by the cardiology department in weeks, median (range) | 32 (5 postpartum) |
| Oxygen saturation % at admission (range) | 94.7 (50 100) |
| Smoking history: number of patients (%) | |
| Never | 99 (95.1) |
| Former smoker | 4 (3.85) |
| Active consumption | 1 (0.96) |
| Alcohol consumption during pregnancy: number of patients (%) | |
| No | 102 (98.08) |
| Yes | 2 (1.92) |
| Functional status classified at admission: number of patients (%) | |
| NYHA I | 77 (74.04) |
| NYHA II | 17 (16.35) |
| NYHA III | 7 (6,73) |
| NYHA IV | 3 (2.88) |
| Modified WHO risk: number of patients (%) | |
| I | 12 (11.54) |
| II | 59 (56.73) |
| III | 16 (15.38) |
| IV | 17 (16.35) |
| Echocardiographic findings | |
| Ejection fraction % (range) | 61 (20 85) |
| Right ventricular dilatation: number of patients (%) | |
| No | 80 (76.92) |
| Yes | 24 (23.08) |
| Comorbidities: number of patients (%) | |
| Hypertension | 12 (11.5) |
| Hypothyroidism | 4 (3.8) |
| Hyperthyroidism | 1 (0.96) |
| Type 2 diabetes mellitus | 2 (1.92) |
| Cerebrovascular disease | 2 (1.92) |
| Ischemic stroke | |
| Pulmonary embolism | 1 (0.96) |
| Systemic lupus erythematosus | 2 (1.92) |
| Takayasus arteritis | 1 (0.96) |
| Mixed connective tissue disease | 1 (0.96) |
| Antiphospholipid syndrome | 1 (0.96) |
| Immune thrombocytopenic purpura | 1 (0.96) |
| Epilepsy | 1 (0.96) |
| HIV infection | 1 (0.96) |
| Chronically used medications: number of patients (%) | |
| None | 75 (72.12%) |
| Calcium antagonists | 5 (4.8) |
| Methyldopa α | 5 (4.8) |
| Furosemide | 5 (4.8) |
| ACEI | 5 (4.8) |
| ASA | 5 (4.8) |
| α-blocker | 4 (3.85) |
| Levothyroxine | 4 (3.85) |
| Enoxaparin | 4 (3.85) |
| Steroids | 3 (2.88) |
| Warfarin | 3 (2.88) |
| ARA-II | 1 (0.96) |
| Spironolactone | 1 (0.96) |
| Chloroquine | 1 (0.96) |
| Azathioprine | 1 (0.96) |
| Sildenafil | 1 (0.96) |
| Hydrochlorothiazide | 1 (0.96) |
| Metformin | 1 (0.96) |
| Clonidine | 1 (0.96) |
| Digoxin | 1 (0.96) |
| Anticoagulation indication: number of patients (%) | |
| None | 98 (94.23) |
| Mechanical heart valve | 4 (3.85) |
| Venous thromboembolism | 1 (0.96) |
| Thrombophilia | 1 (0.96) |
| Anticoagulation type: number of patients (%) | |
| None | 98 (94.23) |
| Warfarin | 2 (1.92) |
| Enoxaparin without measuring anti-Xa values | 3 (2.88) |
| Warfarin followed by enoxaparin without measuring anti-Xa values | 1 (0.96 |
ARA-II: angiotensin II receptor antagonists; ASA: acetylsalicylic acid;
ACEI: angiotensin-converting enzyme inhibitors, NYHA: New York Heart Association.
Results
A total of 104 patients with an average age of 25 ± 6.5 years and an average gestational age of 32 ± 8 weeks at cardiologic evaluation were included in the study, out of whom 74% were in NYHA functional Class I (Table 1).
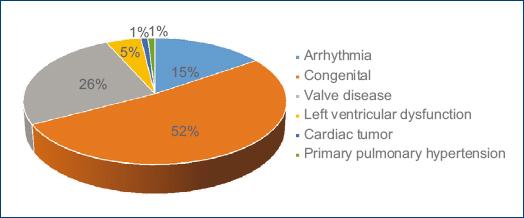
Congenital heart disease was the most common primary diagnosis in the assessed pregnant women with 51.92%, followed by valvular heart disease with 25.95%, arrhythmias with 15.38%, and left ventricular dysfunction with 4.81%. Other less frequent heart alterations were idiopathic pulmonary arterial hypertension and cardiac tumors with 0.96% each (Fig. 1). Specific heart condition diagnoses and their frequency of occurrence are described in table 2.
Table 2 Specific cardiac diagnoses and frequency of occurrence
| Variables | n = 104 |
|---|---|
| Mitral valve regurgitation, n (%) | 11 (10.6) |
| Patent ductus arteriosus, n (%) | 10 (9.62) |
| Ventricular septal defect, n (%) | 10 (9.62) |
| Ventricular septal defect with Eisenmenger syndrome, n (%) | 2 (1.92) |
| Ventricular septal defect + atrial septal defect, n (%) | 4 (3.85) |
| Ventricular septal defect with Eisenmenger syndrome + persistent truncus arteriosus, n (%) | 1 (0.96) |
| Atrial septal defect, n (%) | 8 (7.69) |
| Atrial septal defect + abnormal venous drainage, n (%) | 1 (0.96) |
| Supraventricular tachycardia due to re-entry phenomenon, n (%) | 8 (7.69) |
| Bivalve aorta without stenosis or severe insufficiency, n (%) | 6 (5.77) |
| Left ventricular dysfunction, n (%) | 5 (4.81) |
| Double mitral lesion, n (%) | 5 (4.81) |
| Mechanical valve, n (%) | 3 (2.88) |
| Ebstein anomaly, (%) | 3 (2.88) |
| Increased ventricular automaticity, n (%) | 3 (2.88) |
| Corrected aortic coarctation, n (%) | 3 (2.88) |
| Advanced AV block without previous pacemaker, n (%) | 2 (1.92) |
| Mitral stenosis, n (%) | 2 (1.92) |
| Congenital pulmonary stenosis, n (%) | 2 (1.92) |
| Aortic stenosis, n (%) | 2 (1.92) |
| Mitral valve regurgitation + aortic valve regurgitation, n (%) | 1 (0.96) |
| Congenitally corrected transposition of the great arteries + mechanical valve + pacemaker, n (%) | 1 (0.96) |
| Infective endocarditis, n (%) | 1 (0.96) |
| Biological prosthetic valve, n (%) | 1 (0.96) |
| Presence of pacemaker due to complete AV block, n (%) | 1 (0.96) |
| Aortic valve regurgitation, n (%) | 1 (0.96) |
| Corrected tetralogy of Fallot, n (%) | 1 (0.96) |
| Primary pulmonary arterial hypertension | 1 (0.96) |
| Atrial tachycardia, n (%) | 1 (0.96) |
| Uncorrected tetralogy of Fallot, n (%) | 1 (0.96) |
| Atrial fibrillation, n (%) | 1 (0.96) |
| Corrected AV canal, n (%) | 1 (0.96) |
| Fibroelastoma, n (%) | 1 (0.96) |
Primary cardiac episodes occurred in 13.5% of cases and the most common was pulmonary edema in 8.65% of patients. Obstetric events were observed in 14.42% and neonatal events in 28.85% of cases. The delivery route was cesarean section in 50% of patients; however, the majority had obstetric indications (39%), and only 11% was due to heart disease.
In the univariate analysis, the outcome was found to be related to the following factors: NYHA functional class, HDP, cesarean delivery, gestational age of < 27 weeks, hypoxemia, and mWHO risk classification (Table 3). Gestational age was associated with adverse outcomes; however, this was limited to neonatal episodes, as it was expected.
Table 3 Risk factors and adverse outcomes in heart disease and pregnancy (univariate analysis)
| Variable | − Outcome | + Outcome | Total | χ2 | p |
|---|---|---|---|---|---|
| NYHA | 59 | 45 | 104 | 9.98 | 0.019 |
| Pregnancy > 2 | 17 | 19 | 36 | 2.02 | 0.154 |
| Hypertension during pregnancy | 0 | 10 | 10 | 14.5 | 0.000 |
| Ejection fraction < 40% | 1 | 2 | 3 | 0.74 | 0.38 |
| RV dilatation | 11 | 13 | 24 | 1.5 | 0.21 |
| Pulmonary arterial hypertension | 27 | 28 | 55 | 3.06 | 0.08 |
| Cesarean delivery route | 24 | 28 | 52 | 19.6 | 0.000 |
| Gestational age < 27 weeks | 0 | 10 | 10 | 14.5 | 0.0001* |
| Hypoxemia | 0 | 5 | 5 | 6.88 | 0.009 |
| WHO classification | 59 | 45 | 104 | 28.21 | 0.000 |
*Neonatal episodes; χ2 of 93.2; p = 0.000; obstetric episodes, χ2 of 0.27, p = 0.59; primary cardiac episodes, χ2 of 0.06, p = 0.8.
In the multivariate analysis, only two factors maintain an association with the outcome: delivery route by cesarean section (odds ratio [OR], 2.68; 95% CI, 1.05-6.86) and gestational age at delivery (OR, 0.39; 95% CI, 0.22-0.67). When included in the model, the NYHA functional class, multiparity, right ventricular dilatation, pulmonary blood pressure, delivery route, gestational age at delivery, and oxygen saturation variables showed a Chi-square of 60 (p = 0.000), pseudo-R2 of 0.58 and area under the curve of 0.93.
mWHO risk classification (mWHO)
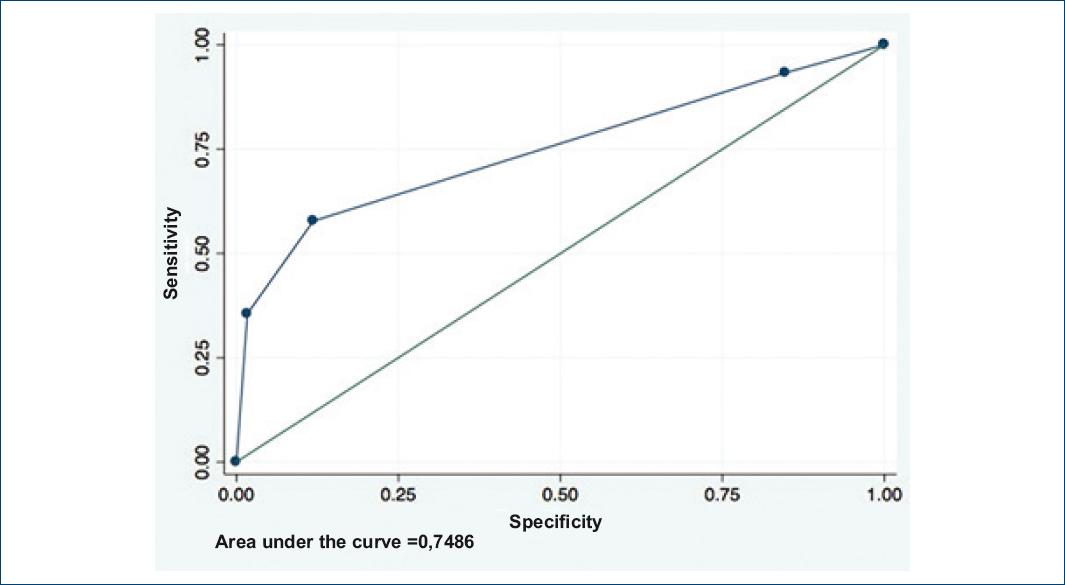
The mWHO risk classification showed the following results: mWHO I with positive outcome, 3/12 (25%); mWHO II, 16/59 (27%); mWHO III, 10/16 (62.5%); and mWHO IV, 16/17 (94%) (tendency Chi-square, 23.21; p = 0.000001). When the mWHO I risk classification (lower-risk heart disease) was taken as reference and compared with mWHO II classification, MantelHaenszel (MH) OR is 1.11 (95% CI, 0.26-4.65); with mWHO III, MH OR is 5 (0.95-26.1), and with mWHO IV, MH OR is 48 (4.32-532). The area under the curve for differentiation (receiver operating characteristic [ROC] curve) is 0.75, with adequate calibration (hearing level > 0.05) (Fig. 2).
Discussion
Patients with heart disease during pregnancy are at high risk of both cardiac and obstetric and neonatal episodes, as explained not only by the stress imposed by gestational changes but also by the socioeconomic profile, which in the setting of the authors includes late evaluation at a high complexity center and lack of preconception assessment. NYHA functional class, HDPs, cesarean section as delivery route, gestational age of < 27 weeks, hypoxemia, and mWHO risk classification behave as predictors of adverse events in the univariate analysis, although only the delivery route and gestational age retain their predictive capacity in the multivariate analysis. These variables have a good discriminating capability (ROC, 0.93) in the logistic regression model; nevertheless, given the low number of outcomes, they should be considered only exploratory.
The mWHO risk classification for heart disease and pregnancy has an acceptable discriminating capacity (ROC, 0.75), and it is therefore confirmed that it should be the risk scale to be used in this scenario; in addition, it allows monitoring to be planned and early interventions to be defined; this shows that each one of the groups has a different risk when compared with the first one (mWHO I; tendency Chi-square), although the confidence interval (CI) crosses 1 in the mWHO II and III risk groups, which is explained by the sample size, which generates imprecise CIs. This is consistent with recent data from the European Registry of Pregnancy and Cardiac, where the main causes of adverse primary outcomes (maternal death and heart failure) occurred in patients with mWHO IV conditions, such as pulmonary hypertension and cardiomyopathy7.
In most cases, the route of choice for delivery is vaginal, since cesarean section is reserved for obstetric indications8 and for complex or decompensated heart disease, since it attenuates changes observed with labor, which could aggravate disorders such as aortic dissection and aortic root dilatation of more than 45 mm, severe valve stenosis of the left side, highly severe cases of pulmonary hypertension, or established heart failure; in these conditions, cesarean section would allow better invasive and non-invasive monitoring1,9; however, it is associated with higher risk of postpartum hemorrhage, infection, surgical accidents, and thromboembolic episodes, which are further increased when urgently performed. These are possibly the reasons why it persists as a predictor in the multivariate analysis in the described cohort. Pregnancy termination, either vaginally or by cesarean section, should be planned and, protocols for care should be previously established by a multidisciplinary and experienced group to improve the outcomes.
Gestational age is related to adverse events, particularly neonatal, as it would be expected due to vulnerability of the fetus when it is far from term, as described in other cohorts9,10. The elevated rate of adverse effects in patients with heart disease during pregnancy forces to develop multidisciplinary programs for the care of this vulnerable population, which overcome socioeconomic barriers, especially in relation to late care, which on average occurred at 32 weeks of gestation in this cohort, which has produced a marker of adverse outcomes in a recent study (when the first assessment has place after 20 weeks of gestational age)11. The current cohort, developed as a prelude to organizing a cardio-obstetric group in a high-complexity center, supports this need. This studys limitations include its retrospective nature; however, the follow-up of a current prospective cohort, with earlier intervention, will allow to change the horizon and determine with higher accuracy the predictive factors of adverse episodes and develop specific scales adjusted to local reality. On the other hand, the retrospective nature of the trial itself prevented the development of scales that enabled echocardiographic studies inter-observer and intra-observer variability to be determined. Nevertheless, the echocardiography department has strict adherence to the American Society of Echocardiography recommendations for obtaining diagnostic images.
Conclusions
Pregnant women with heart disease in this cohort had a late evaluation, which in part could have led to the high rate of adverse effects. Gestational age of < 27 weeks and delivery by cesarean section behaved as predictors of maternal-fetal adverse results in the multivariate analysis. On the other hand, mWHO risk classification independent evaluation was acceptably predictive of adverse outcomes and is suitable for assessment and planning of patient follow-up. The search for risk factors that help predict adverse outcomes in pregnant patients with heart disease is essential to achieving a quality multidisciplinary care that allows improving the results.











 nueva página del texto (beta)
nueva página del texto (beta)