Sixty-nine-year-old male, with a history of mitral-aortic mechanical valve replacement and ascending aorta repair with a tubular prosthesis two years prior, who was admitted with biventricular heart failure (predominantly right). In the echocardiogram, highlighted the existence of a severely dilated and dysfunctional right ventricle (RV), a prostheses with high gradients and a severe pulmonary hypertension; the transesophageal echocardiography (TEE) ruled out prosthetic thrombosis. By means of computed tomography, the existence of a 92 x 95 mm diameter pseudoaneurysm of the ascending aorta (AAP) was detected; this AAP was surrounding the aortic graft and compressed the right atrium (RA) (Fig. 1 [*]). A second TEE also demonstrated the existence of a fistula connecting the AAP to the RA. The patient underwent surgery: the fistula was closed (Fig. 2 [arrow]), and the aortic valve prosthesis together with the aortic tubular graft (which was not epithelialized and had ruptures in its proximal and distal anastomoses as origins of the PAA), were replaced by a valved tubular aortic prosthesis.
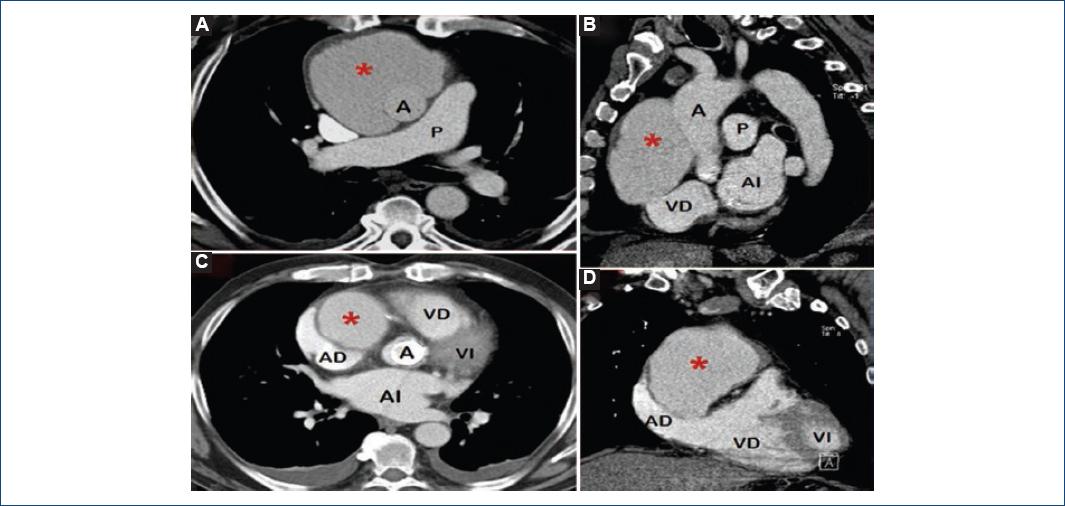
Figure 1 Computed tomography images. A and B: axial sections where the large pseudoaneurysm (*) is observed to be formed around the aortic tubular prosthesis, as well as the severe compression it exerts on the RA. C and D: same alterations but observed in sagittal sections made at the same levels.A: aorta; AD: right atrium; AI: left atrium; VD: right ventricle; VI: left ventricle; P: pulmonary artery.
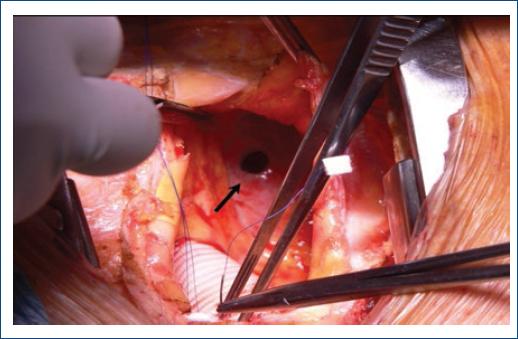
Figure 2 Image of the surgery: opening of the aortic pseudoaneurysm. After drainage of the pseudoaneurysm, the aortic tubular prosthesis, not epithelized, and at the bottom, on its wall, the orifice (arrow) of the fistula into the right atrium are observed.
AAP is a very rare pathology; its incidence, after an aortic intervention, is < 1% and it is favored by perioperative infections1. Usually, its origin is in aortotomy or anastomosis stitches or suture lines (of aortocoronary bypass prostheses or grafts), or at puncture, aortic cannulation or clamping points. Clinical presentation varies according to its localization, size and compression on adjacent structures; however, its presentation as right heart dysfunction (superior vena cava syndrome, RV inflow tract obstruction, or fistula into pulmonary artery, RA or RV) is exceptional2,3.











 text new page (beta)
text new page (beta)


