Introduction
Hypertrophic cardiomyopathy (HCM) is a heart disease characterized by increased thickness of the left ventricle wall without the presence of blood volume overload or any other heart disease explaining the hypertrophy.1
Throughout history, it has been known with different names, including hereditary ventricular hypertrophy, hereditary hypertrophic cardiomyopathy, familial hypertrophic cardiomyopathy, septal asymmetric hypertrophy and idiopathic subaortic stenosis. (In the Spanish language original version of this work, the term myocardiopathy was used rather than cardiomyopathy for two reasons: a) myocardiopathy defines the entity, a disease of the myocardium, and b) the term cardiomyopathy is an anglicism, a calque of English cardiomyopathy.)
The European Society of Cardiology classifies HCM in two groups: a) primary HCM or of genetic origin caused by mutations in various genes1, and b) secondary HCM consecutive to another disease, such as systemic arterial hypertension, valve disease, or various metabolic syndromes, such as Pompe, Fabry and Danon diseases, which affect the structure of cardiomyocytes. This work focuses on primary HCM.
Primary HCM is considered the most common heart disease of hereditary origin, with a prevalence of 1 in 500 individuals, according to statistical data obtained from the Coronary Artery Risk Development in Young Adults (CARDIA) trial2, and it is the sixth most common cause of sudden death in children and young adults in developed countries, according to a study conducted in Australia and New Zealand3.
Signs and symptoms appear in the third and fourth decades of life, with a wide variation in the onset and severity of clinical manifestations, from asymptomatic individuals to the presence of syncope, tachyarrhythmias or abrupt onset with sudden death. However, the diagnosis of the disease is established based on morphological changes such as ventricular wall thickening ≥ 13 mm (measured by echocardiography), with or without obstruction of the outlet tract of the left ventricle4, and electrocardiographic changes in repolarization, T-wave inversion in the DI and aVL cardiac leads, in addition to QT-intervals prolongation5, among other indicators that reflect damage progression and sudden cardiac death risk, with the latter being higher in the 14- to 35-year age group with HCM-secondary symptoms6.
Mendelian inheritance in HCM
Although this is a disease with a well-identified transmission pattern, HCM shows great clinical variability, with age-dependent penetrance, i.e. clinical evolution has great intrafamily and interfamily heterogeneity due to modifying factors that diversify each patients phenotype. This disease is a good example of nature versus nurture7.
Different genetic and genomic studies have tried to elucidate the causes of this hereditary anomaly and have identified DNA modifications, known as genetic variants and classified as benign, likely benign, of uncertain significance, likely pathogenic and pathogenic, which may cause structural changes in sarcomeric proteins of the heart muscle, which favors ventricular hypertrophy, predominantly of the left ventricle.
In general, primary HCM has a Mendelian inheritance pattern of the autosomal dominant type, i.e., the children of an affected subjects possess a 50% risk for inheriting the mutated allele and therefore will suffer from the disease. However, there are de novo cases who have no family history and, even so, affected individuals show an identified pathogenic variant they will inherit to their offspring with the same probability (50%)8; on the other hand, there are reports of cases that show mutations in the MYL3, MYH7 and MYBPC3 genes that suggest a pattern of autosomal recessive inheritance, which should be considered at the time of taking patient history. For this reason, some investigations have tried to elucidate the functional effect of genetic variants that give rise to cardiac alterations, with the purpose to facilitate diagnosis and offer early treatment, even in asymptomatic patients. For the moment, identification of the causal variants, and their functional effect, helps to understand the mechanism that generates hypertrophy and to predict damage severity.
Thanks to the use of next-generation sequencing (NGS), the number of genes related to HCM has significantly increased in the past few years9-11, with more than 50 published genes and nearly 8,000 variants (Table 1) in the PubMed/MEDLINE database related to this disease, out of which only 25 are consistent with the gene compendium Online Mendelian Inheritance in Man (OMIM; http:www.omim.org), where clinical characteristics, genes with the most common pathogenic identified variants and the pathophysiological consequences of these molecular changes are described.
Table 1 Genes and type of variants related to primary cardiomyopathy
| Gene | HCM type | Frequency | No info | Type of described variant (OMIM)* | ||
|---|---|---|---|---|---|---|
| BEN | PATH | UNC | ||||
| ACTC112-17 | 11a | Rare < 1% | 29 | 8 | 29 | 30 |
| TNNC118 | 13a | Rare < 1% | 17 | 4 | 7 | 8 |
| TNNI313,14,19-24 | 7a | Rara < 5% | 47 | 7 | 73 | 39 |
| TNNT213,14,19,21,22,25-27 | 2a | Rare < 5% | 65 | 11 | 81 | 53 |
| TPM113,14,26,28,29 | 3a | Rare < 5% | 83 | 10 | 29 | 51 |
| MYBPC313,14,17,21,22,26,30,31-55 | 4b | 15-25% | 241 | 42 | 1014 | 302 |
| MYH623,26,56 | 14b | Rare < 1% | 183 | 7 | 3 | 13 |
| MYH713,14,17,21-23,30-32,49-52,55,57-69 | 1b | 15-25% | 300 | 41 | 872 | 317 |
| MYL213,17,29,70-72 | 10b | Rare < 2% | 37 | 18 | 25 | 24 |
| MYL313,14,69,73-75 | 8b | Rare < 1% | 21 | 5 | 30 | 21 |
| ACTN213-15,76,77 | 23c | Rare < 1% | 76 | 30 | 9 | 45 |
| CSRP378,79 | 12c | Rare < 1% | 24 | 9 | 5 | 12 |
| LDB380 | 24c | Rare 1-5% | 151 | 8 | 0 | 5 |
| MYOZ267,81 | 16c | Rare < 1% | 36 | 1 | 8 | 2 |
| MYPN82 | 22c | Rare < 5% | 42 | 39 | 4 | 30 |
| NEXN83 | 20c | Rare < 1% | 35 | 10 | 4 | 45 |
| TCAP84 | 25c | Rare < 1% | 31 | 1 | 0 | 4 |
| TTN15,26,51,72,85 | 9c | Rare < 5% | 3949 | 2 | 12 | 20 |
| VCL86 | 15c | Rare < 1% | 54 | 24 | 3 | 30 |
| CALR37 | 19d | Rare < 5% | 4 | 0 | 0 | 1 |
| JPH288,89 | 17d | Rare < 1% | 6 | 13 | 6 | 15 |
| PLN90 | 18d | Rare < 1% | 7 | 0 | 5 | 5 |
| CAV391 | 1e | Rare < 5% | 54 | 11 | 5 | 8 |
| MYLK292 | 1e | Rare < 5% | 39 | 17 | 3 | 7 |
| PRKAG293-98 | 6e | Rare 1% | 100 | 1 | 31 | 4 |
*Information obtained from PubMed up to April 2018.
OMIM: Online Mendelian Inheritance in Man; No info: no information in medical publications; BEN: benign; PATH: pathogenic; UNC: uncertain; a: thin filament protein; b: thick filament protein; c: Z-disk protein; d: proteins included in the management of Ca+; e: other related proteins.
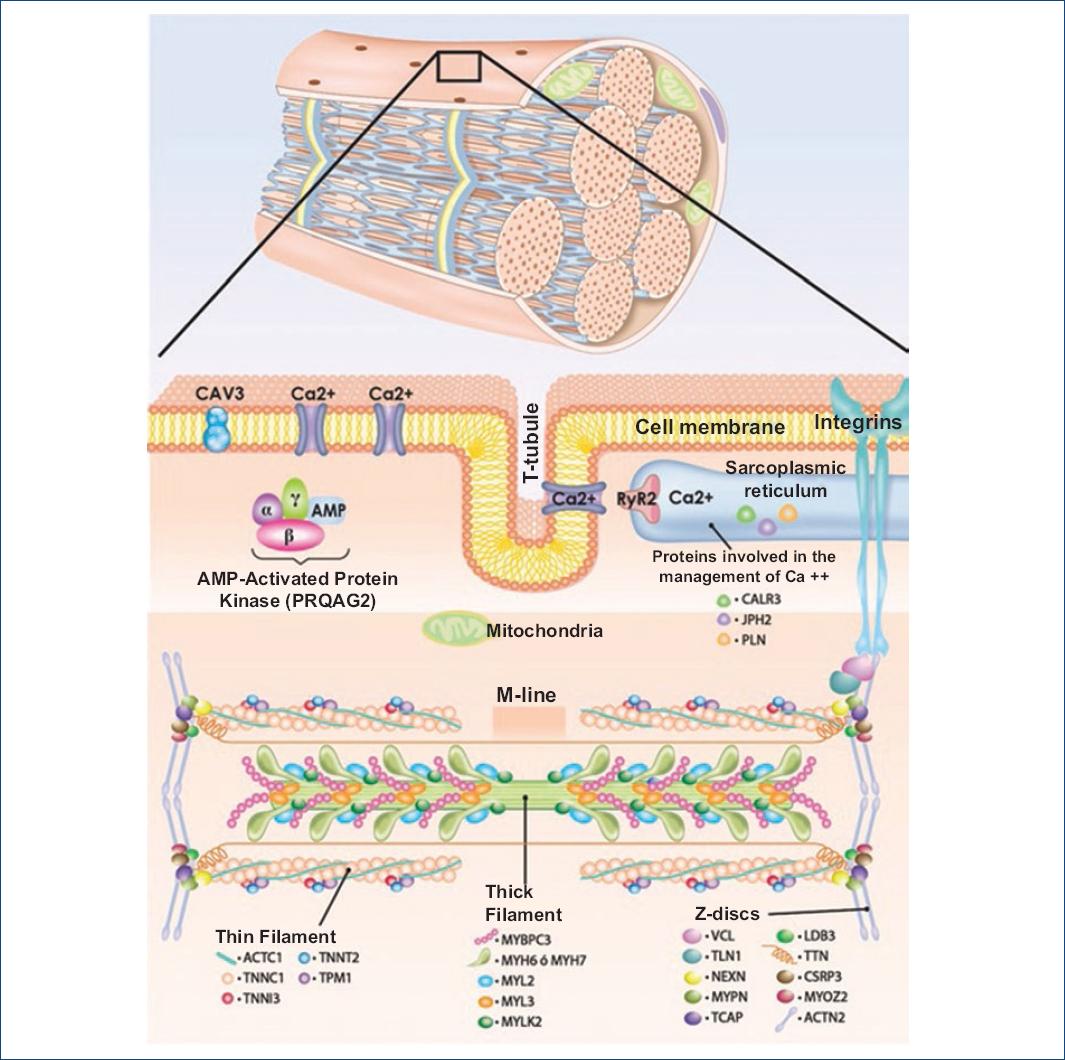
Cardiac cells structure and proteins underlying HCM
Cardiomyocytes are made up of five components: a) tubules and sarcolemma, b) sarcoplasmic reticulum, c) contractile elements, d) mitochondria and e) nucleus. The contractile unit is known as sarcomere, which is formed by thick and thin filaments whose most important proteins are myosin and actin (Fig. 1). Thick filaments are formed by heavy chains of the β-myosin protein. This is a hexameric protein composed of two essential light chains encoded by the MYL2 gene, two regulatory light chains encoded by the MYL3 gene, and two heavy chains encoded by the MYH7 gene, as well as myosin-binding protein C (MYBPC3 gene). The thin filaments are made upof actin (ACTC1 and ACTA1 genes), the troponin complex (TNNC1, TNNI3, TNNT2 genes) and tropomyosin (encoded by the TPM1 gene) (Fig. 1). The alteration of one or several cardiomyocyte components has direct or indirect repercussions on the development of primary HCM7,8.
Alterations in thick and thin myofilaments
Some studies have shown that the pathogenic variants in genes that encode thick and thin filament proteins lead to an energy expenditure increase due to an alteration in ATP use and metabolism9,10. This energy compromise might result in a neuroendocrine system activation in order to develop compensatory cardiac hypertrophy. To study the functional effects of pathogenic variants, Coppini et al.11 conducted a 4.5-year prospective study, where they divided a group of affected individuals according to the altered structure, and thus two groups were formed: one where the patients (n = 80) were carriers of thin filament pathogenic variants and other (n = 150) with pathogenic thick filament variants, and found that patients with thin filament alterations showed higher left ventricular dysfunction and heart failure, in comparison with the group of thick filament alterations, which had more fibrosis, less hypertrophy with atypical distribution, severe diastolic dysfunction, abnormal blood pressure response during exercise and a family history of sudden cardiac death. On the other hand, individuals with pathogenic variants that affect thick filaments suffered higher obstruction of the left ventricular outflow tract due to a pronounced growth of the ventricular wall11. In another study, where nine genes were analyzed in 197 HCM index-cases (including 172 familial cases and 25 apparently sporadic cases), Richard et al.107 found pathogenic variants in 63% of cases; out of these, 42% were found in the MYBPC3 gene sequence and 40% in MYH77. Both genes encode thick filament proteins, and it should be noted that this type of findings are repeated across various investigations108,109 in different ethnic groups. The above turns the MYBPC3 and MYH7 genes into the main subject of study in cases of HCM with a family history of sudden death or non-lethal cardiac arrest (Table 2).
Table 2 Sarcomere genes whose pathogenic or probably pathogenic variants are related to HCM and sudden death
| Gene | Locus | MIM | Protein | Inheritance | FHSD |
|---|---|---|---|---|---|
| Genes that encode thin filament proteins | |||||
| TNNC1 | 3p21.1 | 613243 | Type 1 troponin C | AD | Yes18 |
| TNNI3 | 19q13.42 | 613690 | Type 3 troponin I | AD | Yes19,20 |
| TNNT2 | 1q32.1 | 115195 | Type 2 troponin T | AD | Yes25 |
| TPM1 | 15q22.2 | 115196 | Tropomyosin 1 | AD | Yes28,99 |
| ACTC1 | 15q14 | 612098 | Actin alpha cardiac muscle 1 | AD | Yes12 |
| Genes that encode thick filament proteins | |||||
| MYBPC3 | 11p11.2 | 115197 | Cardiac myosin-binding protein C | AD/AR | Yes23,43,47,49,55,74,100-103 |
| MYH6 | 14q11.2 | 613251 | Alpha-myosin heavy chain | AD | Yes56 |
| MYH7 | 14q11.2 | Beta-myosin heavy chain | AD/AR | Yes46,49,55,57,58,67,100,104,105 | |
| MYL2 | 12q24.11 | 608758 | Ventricular regulatory myosin light chain | AD | Yes70,71 |
| MYL3 | 3p21.31 | 608751 | Myosin 3 light chain | AD/AR | Yes36,73-75,106 |
MIM: corresponding number in the Mendelian Inheritance in Man database; FHSD: family history of sudden death; AD: autosomal dominant; AR: autosomal recessive.
The MYBPC3 gene and its role in HCM
The MYBPC3 gene is located in chromosome 11 short arm, which encodes the cardiac myosin-binding protein C isoform (MYBPC or MyBPC). This protein is expressed only in the cardiac muscle and is localized specifically in the sarcomere transverse A bands, bound to myosin heavy chains in thick filaments; therefore, it is considered a member of the tripartite complex together with actin and myosin, and thus it regulates cardiac contraction through phosphorylation events101,110.
The mechanism by means of which its pathogenic variants lead to the development of HCM is still a matter of discussion, but two hypotheses have been proposed. One of them attributes clinical manifestations of haploinsufficiency, with an increased sensitivity to calcium111, while the second favors the hypothesis of a toxic effect of the altered protein112.
The study of the MYBPC3 gene gained interest due to the increasingly common use of molecular biology technologies for diagnosis, which have found a consistent relationship between pathogenic variants of this gene and the development of HCM113, and thus far, more than 450 pathogenic or probably pathogenic variants have been documented in the Human Gene Mutation Database (HGMD; http://www.hgmd.cf.ac.uk).
The molecular study in cases of sudden death led various researchers to the association with HCM due to the presence of pathogenic variants in proteins that are involved in the functioning of the sarcomere. In this context, Cann et al.49 carried out a study of molecular necropsy in 96 cases of sudden cardiac death and identified 50 cases with cardiomyopathy, out of which 15 had HCM, and out of these, three exhibited pathogenic variants in the MYBPC3 gene and had a history of sudden death of cardiac origin during exercise, immediately after exercise or during sleep49. Late-onset clinical characteristics and a high frequency of a family history of sudden death in those affected do repeat across multiple studies in different populations around the world53,113.
The MYH7 gene and its role in HCM
The MYH7 gene is localized at chromosome 14 long arm and encodes the myosin heavy chain β isoform (MYH or β-MHC), a protein that is expressed in the striated muscle of mammals (predominantly in the ventricles) and that is part of the sarcomere thick filaments114. MYH7 is the first gene whose pathogenic variants were associated with HCM and whose negative dominant effect is well described115,116.
So far, more than 350 pathogenic variants have been documented in the MYH7 gene in HGMD, with highly variable clinical phenotypes, as in the cohort study by García-Castro et al.108 in 120 unrelated patients with HCM. The subjects of this study were underwent history taking and molecular study, with 31 different pathogenic variants being identified in 32 patients, 8% of whom (10 patients) had alterations in the MYH7 gene; mean age at which the diagnosis was established was 35 years, and 3 out of these 10 patients (70%) had a family history of HCM108.
As for the prognosis for MYH7 gene pathogenic variants carriers, Wang et al.117 reported in 2008 that the pathogenic variants of this gene produce more aggressive phenotypes in comparison with those that affect the MYBPC3 gene, with early-onset manifestations (16 years of age) and high risk of sudden death117.
Various investigations have tried to establish the genotype-phenotype correlation in order to facilitate early diagnosis in asymptomatic subjects, but this has been difficult to establish due to the large number of pathogenic variants identified in different genes (locus heterogeneity), to a possible additive effect that modifies the phenotype as in the case of age at presentation and prognosis, to a high clinical variability of this disease and influence of the environment48.
Pathogenic or probably pathogenic variants located in MYBPC3 and MYH7 in relation to sudden death
Currently, there are a dozen pathogenic or probably pathogenic variants related to sudden death in different populations around the world; most of them produce a reading frameshift and, as a consequence, the synthesized protein is truncated due to a premature termination codon. Below, some of them are synthetically described within the context of sudden death.
Variants related to HCM and history of sudden death for the MYBPC3 gene
p.Glu542Gln: This change has been described in seven unrelated index cases. In the molecular plane, the last nucleotide of a consensus splice site is disrupted, and as an effect, a short protein of 486 amino acids is obtained118.
p.Cys719Arg: This change was identified in 2017 in an apparently sporadic case of Chinese ancestry whose cause of death was unknown and, in the death report, sudden death was concluded47.
p.Glu334Lys: It was identified in a 48-year-old man of Korean ancestry, diagnosed by echocardiography as a phenocopy of the Brugada syndrome at admission diagnosis. He was survivor of a non-lethal cardiac arrest100.
p.Pro108Alafs*9: This is an insertion of the GCTGGCCCCTGCC nucleotides at exon 3 position 29. The variant was initially identified in 13 families from southern Spain; therefore, 107 relatives were studied and, out of them, 39 had HCM, with male predominance and with five documented cases of sudden death and enlarged left ventricular mass in carriers of this variant43. In the protein, length is reduced to 115 amino acids, out of which eight are new.
p.Gly1093Cys: 96 necropsies of sudden death cases were analyzed, among which one proband had died immediately after practicing exercise, which is why genetic testing of 12 relatives was requested, eight of which were positive for this change and two cases had cardiac symptoms related to HCM49.
p.Arg668His: The index case apparently died during sleep, which is why 27 relatives were studied, out of which 10 were positive for the variant and four experienced symptoms related to HCM49. This variant had already been previously reported119.
p.Arg502Trp: The index case died while practicing exercise, which is why five relatives underwent genetic testing, out of which three were positive, one of them with symptoms related to HCM49.
IVS5+5G→C: This variant corresponds to a substitution of cytokine by guanine five base pairs downstream of the 5 splice donor site in intron 5 of the MYBPC3 gene. This modification causes a change in the reading frame and incorporates 15 amino acids after position 165, which ultimately causes a truncated protein. Lin et al. report the case of a family with a history of sudden death in the probands brother, who died at 20 years of age. Both the father and the proband are HCM clinical carriers120.
p.F305Pfs*27: This is a deletion of two thymines in exon 11 that causes a termination codon and therefore a truncated protein. Calore et al. studied a series of 97 probands of Italian origin diagnosed with HCM, out of which 19 were carriers of the variant, plus 45 carriers detected by cascade screening. Penetrance in this series of patients was 75%; in eight carriers there was a family history of sudden death, and the prognosis is therefore reserved for those with the variant after the fourth decade of life52.
Lys1209Serfs*28: In combination with p.Gly100Ser, found in PRKAG2 (probable additive effect), Zhao et al. studied 18 patients diagnosed with HCM, among which one proband had two variants and a history of sudden death in the mother and maternal grandmother; the proband phenotype is consistent with severe hypertrophy and HCM early onset23.
Variants related to MCH and history of sudden death for the MYH7 gene
p.Arg453Cys: In this variant, a change of charge is observed due to an amino acid change, and thus, a more aggressive phenotype has been reported in comparison with Val606Met and Phe85Cys121,122. Ko et al. studied a group of 20 individuals originating in one family, all of them older than 16 years; in 11 cases, clinical HCM was suspected, and in seven, the disease was confirmed by echocardiography. This family has a history of three cases of sudden death and two with end-stage heart disease108.
p.Arg1045Leu: In this family, whose proband passed away during sleep, four individuals were studied, out of whom one relative was identified with clinical data consistent with HCM49.
p.Arg719Trp: Anan et al. conducted a genetic study in four different families with a history of HCM and at least 22 cases of sudden death, which determined a higher risk of adverse effects for the carriers of the variant123.
p.Asn391Thr: Feng et al. studied an extended family of the Han ethnic group (China) diagnosed with HCM, which included three generations and 22 individuals, out of which three died with a diagnosis of HCM; the age at disease symptoms onset was in most cases < 20 years58.
p.Gly716Arg: Hwang et al. studied a Korean family composed of 32 members belonging to four generations. In this family, there was a history of four individuals with sudden death at an early age; genetic testing showed that 13 individuals were carriers of the variant124.
p.Arg403Gln: Marian et al. studied a family with seven positive cases for this variant. In this family, the onset of symptoms occurred on average at 22 years of age; however, a 10-year-old male individual was asymptomatic. Kaplan-Meier survival analysis showed that p.Arg403Gln variant carriers have an 11% likelihood of remaining alive at 60 years of age125. This variant had been previously reported with a high incidence of sudden death in other three families126-128.
p.Arg453Cys: This variant was recognized in the 1990 decade in a family with 13 individuals affected with HCM and a history of six sudden death cases. Initially, screening for the detection of variants was carried out with the help of ribonuclease protection studies, and at the familiar level, the disease was associated with the variant found by means of linkage analysis; this change produces a modification in amino acid charge (-1) and has been related to lower survival128.
p.Glu848Gly: This glutamic acid substitution by glycine gives raise to a negative dominant effect by altering the protein-protein (MYH7-MYPC3) bonds that drive to systolic dysfunction and increased risk of sudden death67.
p.Asn391Thr: Nonsense variant found during the study of a family originating in China that had multiple individuals affected by HCM and a history of four members with sudden death58.
Conclusion
MCH is a highly heterogeneous disease due to the large number of affected genes and genes identified as causal factors; in addition, the presence of one or more mutations in proteins that make up the contractile apparatus of the cardiac muscle and, ultimately, environmental influence, give rise to a particular phenotype with variable clinical course, in which sudden death can be the first manifestation. Among the genes that encode proteins that are part of the cardiac muscle contractile apparatus, thick filament MYBPC3 and MYH7 genes are the most frequently identified as causal factors in world medical publications, considering all populations, with more than 350 pathogenic or probably pathogenic variants reported for each gene.











 nueva página del texto (beta)
nueva página del texto (beta)