Introduction
At present, the epidemic of human immunodeficiency virus (HIV) affects more than 36.7 million people globally, with a mortality rate of 1.1 million/year1.
Many of these deaths were due to noninfectious complications like cardiovascular diseases. The first case reported of plexogenic pulmonary arteriopathy associated with HIV was carried out by autopsy2.
HIV-1 infection is one of the major causes of pulmonary hypertension in the world3.
This infection is a risk factor for the development of pulmonary arterial hypertension (PAH), increasing up to 2000-fold its odds4.
The pathogenesis for the development of endothelial vascular lesion in lung circulation like PAH associated to HIV (PAH/HIV) is still unclear.
PAH/HIV is a devastating and life-threatening condition with recent cohort studies reporting prevalence ranging from 2.6 to 15.5%5.
The survival rate of PAH/HIV patients is significantly reduced to one-half compared with HIV-infected individuals without PAH.
Nitric oxide (NO) is a potent pulmonary circulation vasodilator (Fig. 1) linked to homeostatic effects in different pathologies.

Figure 1 Synthesis of nitric oxide (NO) by endothelial nitric oxide synthetase, NO is produced when an electron from oxygen is transferred to an amino terminal nitrogen of L-arginine.
NO is synthesized from L-arginine and oxygen through a reaction catalyzed by endothelial NO synthase (eNOS)6,7.
Myriad effects of NO on pulmonary vascular cell tone such as proliferation, apoptosis, and angiogenesis have been demonstrated. Once released, it rapidly diffuses across cell membranes to reach the cytoplasm of adjacent vascular smooth muscle cells, where it binds to soluble guanylate cyclase and increases intracellular cyclic guanosine monophosphate (cGMP) levels. cGMP, in turn, phosphorylates cGMP-dependent protein kinase, which acts at several sites within the cell membrane and endoplasmic reticulum to lower intracellular calcium levels and reduce cross-linking of myosin light chain and decrease vascular tone8.
Asymmetric dimethylarginine (ADMA) competitively inhibits eNOS and, thus, is a mediator of endothelial dysfunction. NO inhibits endothelial apoptosis and increases vascular endothelial growth factor expression to facilitate angiogenesis.
There is no definitive proof that HIV directly causes PAH or infects pulmonary endothelial cells. Nevertheless, HIV proteins (Nef, Tat, and Env) play key roles in PAH-associated pulmonary vascular remodeling because their interactions with molecular partners in the infected cells induce inflammation, oxidative stress, and deregulate apoptosis and proliferation of vascular endothelial cells9.
In this work, we looked at the presence and expression of eNOS in multiple grades of pulmonary complex vascular lesions in HIV patients (PCVL/HIV) and made a comparison to non-PCVL/HIV.
Methods
Tissue and histological examination
Pulmonary tissues of patients deceased from January 2006 to December 2016 for HIV-pulmonary complications were collected during autopsies; in addition, lung tissues of HIV patients who died from acquired immunodeficiency syndrome (AIDS) with no data of PCVL (non-PCVL/HIV) cases were included in the study.
Tissues collected were formalin fixed and paraffin embedded. Lung serial sections were stained with hematoxylin and eosin (H&E).
For this study, we used a simplified of the classical Heath and Edwards histopathology classification10 (Table 1).
Table 1 Heath and Edwards pulmonary circulation simplified pathology classification
| Severity Grades |
|---|
| Grade I: Hypertrophy of the media of small arteries and arterioles and proliferation of the intima |
| Grade II: Thickening of the middle layer with hypertrophy and hyperplasia, showing plexiform lesions in the muscle |
| Grade III: Injury and cavernous angioma, with intimal hyalinization, fibrosis, and/or necrotizing artery |
Immunohistochemistry and immunochemiluminescence
Reagent used for the immunohistochemistry was the endothelial anti-NO synthase (Abcam®, ab66127, Cambridge, MA)11.
For the automated process of immunohistochemical staining, the Ventana® system (Tucson, Arizona) was used12.
The eNOS quantification was measured by chemiluminescence on slides stained with H&E first and processed by the image processing software named ImageJ, download free provided by the National Institutes of Health of the United States13.
The expression of the protein was measured in pixel units (arbitrary units).
Results
Lung tissues from a total a 57 subjects with HIV (52 men) with an average age of 38.3 years (SD 2.12). All patients were in AIDS (Stage C3) according to the classification of the Center for Disease Control and Prevention (CDC) in Atlanta, GA, USA.
The cause of death was mainly pulmonary complications (Table 2).
Table 2 Summary of demographic and disease characteristics HIV/AIDS study group
| n | 57 |
| Mean age, years (range) | 38.3 years ± 2.12 years (22-60) |
| Male (%) | 88 |
| HIV risk factor (%) | |
| Intravenous drug use | 1 |
| Homosexual | 41 |
| Heterosexual | 15 |
| Pulmonary coinfections | |
| PCP | 21 |
| Polymicrobial | 16 |
| CMV | 10 |
| Histoplasma sp. | 6 |
| MTB | 4 |
| Median CD4, SD cell count cells/µl (range) | 36 ± 3 cells (1-115) |
| Viral load count, SD (range) | 355,000 ± 165,000 (150,000-1 million) |
| Median follow-up, years (range) | 3.0 ± 2.3 (0-9) |
| HAART | |
| 37 used before hospitalization | |
| 10 initiated at or after HIV diagnosis in hospital | |
| 10 never received | |
PCP: Pneumocystis jiroveci; CMV: Cytomegalovirus; MTB: Mycobacterium tuberculosis; HAART: highly active antiretroviral therapy; AIDS: acquired immunodeficiency syndrome; HIV: human immunodeficiency virus; SD: standard deviation
Lung tissues were paraffin embedded and H&E stained and processed for immunohistochemistry and were examined microscopically by an experienced pathologist in pulmonary circulation (M.R.R.R.) who determined that 30/57 tissues (55%) showed PCVL with histological evidence of pulmonary vasculopathy or different types: proliferative (60%), plexiform (25%), and obliterative pattern (15%) (Fig. 2).
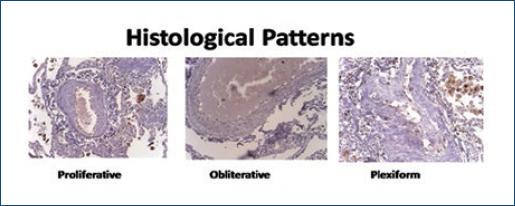
Figure 2 Examples of the most representative pulmonary circulation lesions in autopsy material of acquired immunodeficiency syndrome patients (hematoxylin and eosin staining).
PCVL/HIV histological presentation: eight cases in Grade I, 7 in Grade II, and 15 in Grade III. eNOS imagej chemiluminescence showed a marked decrease expression associated with the severity of the lesion: non-PCVL/HIV group (17 lung tissues) had 106 pixels (SD 5.10) and PCVL/HIV group: 97 pixels (SD3.20) in Grade I, 95 pixels (SD 3.94) in Grade II, and 93 pixels (SD 3.70) in Grade III, statistical analysis of the Wilcoxon test showed significance (p < 0.05) among the four groups.
The statistical analysis of the Wilcoxon test showed significance (p < 0.05) after comparison of the intensity of Grade I compared with Grade II, and of this compared to Grade III, showing lower expression of eNOS to increased severity of PCVL (Fig. 3)
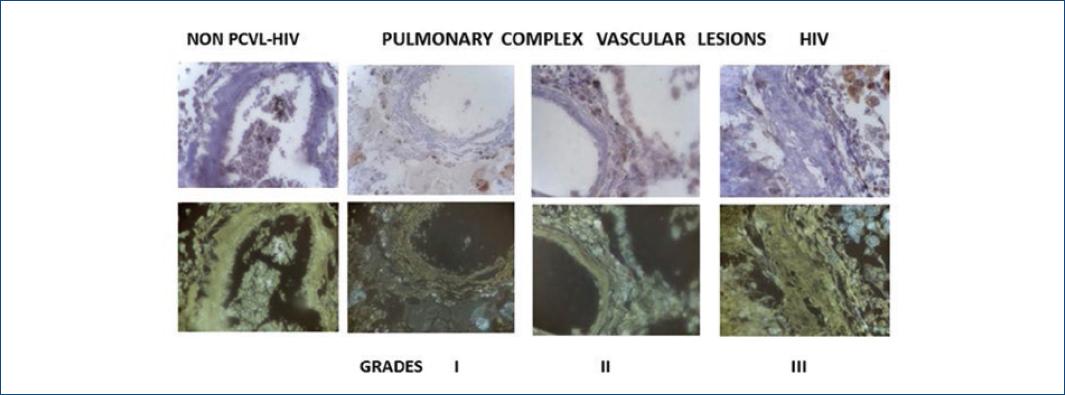
Figure 3 Seen at the top left by immunohistochemical nitric oxide synthetase staining (brown) in non-pulmonary complex vascular lesions (PCVL)-human immunodeficiency virus (HIV) lesions (all Grade III) and the different PCVL-HIV degrees (I-III).At the bottom, the tissues are subjected to the image processor (imageJ) observed the expression of endothelial nitric oxide synthetase (gray).*Non-PCVL-HIV: non-pulmonary complex vascular lesion in HIV patients.
In all measurements of eNOS chemiluminescence in PCVL/HIV have significant diminution than in comparison with the caused by non-PCVL/HIV (Fig. 4).
Discussion
Infection with HIV infection induces a chronic inflammatory state and persistent immune activation and dysregulation that could indirectly induce the release of pro-inflammatory cytokines and growth factors that may be implicated in the pathogenesis of pulmonary vasculopathy.
These features include concentric laminar intimal fibrosis, medial hypertrophy, recanalized thrombi, and plexiform lesions. Additional hallmarks include increased expression of smooth muscle cell/fibroblast growth factors such as platelet-derived growth factor; inflammatory cells are present in the perivascular of HIV tissues, suggesting that HIV-induced chronic inflammation and immune hyperactivation may enrich the pro-inflammatory milieu implicated in vascular lesions.
Endothelial injury has been proposed to be a critical step in the initiation and progression of vascular remodeling associated with PAH14.
Endothelial alterations precede the development of muscularization of pulmonary arteries in animal models15.
It has been considered to the PCVL-HIV as a process of dysfunction of the vascular endothelium where you can engage different mechanisms such as the accessory proteins of HIV (Nef, Tat, and Env)16 in the inactivation of NO conditioned by alterations in the role of eNOS. The exact role that NO plays in the pathophysiology of PAH is still unclear. Numerous studies have demonstrated that pulmonary hemodynamics and functional capacity can be improved in these patients by increasing NO delivery to the lung17-19.
Our study is limited by the lack of hemodynamic data before death for a conclusive diagnosis of PAH, due to the lack of clinical suspicion by the treatment group (internal medicine, infectious diseases, and pulmonologist specialist) for the request of an echocardiogram in addition to the impossibility of performing right cardiac catheterization in a patient with severe sepsis.
Pharmacologic therapies that target the NO/cGMP pathway represent one of the major approaches to medical management or the patient with PAH20,21.
Increase levels of ADMA are independently associated with HAP-HIV, the ADMA-NO axis is an important mechanism to be studied in the future22.
In non-human primates as animal models like macaques the infection with Simian immunodeficiency virus/nef recombinant virus demonstrated pulmonary vascular remodeling without lesions were found in outside lung organs, suggesting a pulmonary-specific target23.
Numerous pieces of the NO synthesis and signaling pathways are disrupted or altered in pulmonary vascular diseases. Although the data implicating NO deficiency in the pathogenesis of PAH are compelling, it is unclear which part of the biosynthesis pathway is impaired.
Evidence is accumulating that modification of deficiencies in NO synthesis and/or enhancement of its downstream signaling targets can attenuate pulmonary vascular remodeling.
Despite the increase in survival of HIV patients as a result of highly active antiretroviral therapy, pulmonary complications are still prevalent in the presentation of pulmonary vasculopathy even in asymptomatic patients. The accurate clinical diagnosis in the initial phase of the disease is necessary to improve the prognosis and survival.
These results show the preponderant reduce the presence of eNOS in pulmonary vasculopathy in AIDS patients. To the best of our knowledge, this is the first work that shows the significant diminution of eNOS in PCVL/HIV compared to non-PCVL/HIV.
It is important to continue the study in the future of NO and the inflammatory mechanism of the retroviruses on the pulmonary circulation, to promote a biological marker to detect PAH-HIV in asymptomatic patients and guide the therapy in the initial stages of this pathology24,25.











 nueva página del texto (beta)
nueva página del texto (beta)



