Introduction
Atherothrombosis (AT), the leading cause of mortality in the Western world, is defined as an atherosclerotic plaque disruption with superimposed thrombosis1. AT is the main cause of ischemic heart disease, ischemic stroke, and peripheral arterial disease2. AT may also occur in patients with arrhythmias, such as atrial fibrillation, and in those who have undergone percutaneous or surgical revascularization procedures.
Human platelets are involved in normal and pathological hemostasis. During the AT process, platelets act as essential mediators of several thrombotic and inflammatory events. Clopidogrel (CLO), an antiplatelet drug, inhibits the P2Y12 receptor, which is responsible for mediating the platelet aggregation by adenosine diphosphate3.
Inhibition of platelet aggregation with drugs such as CLO and acetylsalicylic acid constitutes the main preventive treatment of AT. CLO is one of the most commonly used therapeutic drugs for the secondary prevention of cardiovascular events in patients with acute coronary syndromes4. However, considerable inter-individual variation in CLO response has been documented, resulting in suboptimal therapy and an increased risk of recurrent adverse effects in some patients5.
CLO is a prodrug that requires conversion to an active metabolite by hepatic cytochromes p450 (CYP) to accomplish an antiplatelet effect. The enzyme CYP2C19 has been reported to be the CYP isoform that activates CLO to its active metabolite6. Several single nucleotide polymorphisms (SNPs) in the CYP2C19 gene (OMIM124020) have been identified as strong predictors of CLO-diminished pharmacological response4. Furthermore, a non-satisfactory effect has been observed in 20% of patients with CLO7. CYP2C19 is a liver enzyme that metabolizes a broad range of xenobiotics with clinical importance, such as benzodiazepines, antidepressants, mephenytoin, some proton pump inhibitors, and CLO8.
It has been demonstrated that genetic variants in the CYP2C19 gene affect the pharmacological and clinical response to the standard 75 mg daily maintenance dose of CLO. Furthermore, at least 16 variants have been associated with changes in CYP2C19 enzymatic activity and seven specific variants result in an inactive enzyme. CYP2C19*1 is the wild-type allele, while CYP2C19*2 (rs4244285) is the null allele (rs4244285; 681G>A) and CYP2C19*3 (rs4986893; 636G>A) results in an inactive enzyme9. Recently, the loss-of-function CYP2C19*2 allele has been associated with decreased activation of CLO, poor antiaggregant effect, and increased cardiovascular events10. In high-risk vascular patients, the CYP2C19*2 polymorphism is a strong predictor of adverse cardiovascular events and particularly of stent thrombosis10.
Materials and Methods
Study population
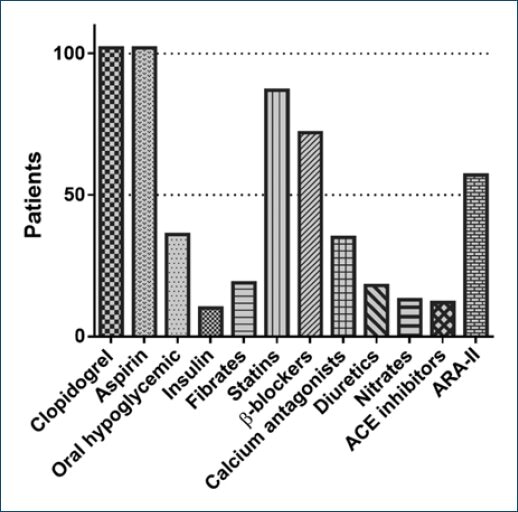
A total of 102 patients from Northeastern Mexico diagnosed with high risk of cardiovascular disease who attended the Cardiology Service of the Hospital Universitario Dr. José Eleuterio González (UANL) and the Institute for Cardiac Arrhythmias and Cardiovascular Diagnosis, S. C. of Monterrey, Mexico, were included. The individuals were recruited from January to August 2015, with a mean age of 68 (35-91) years. The inclusion criteria were as follows: males and females over 18 years, diagnosed with high risk of cardiovascular disease, and who have received treatment with CLO at a maintenance dose of at least 75 mg daily during the last nine consecutive days before the inclusion to the study. Exclusion criteria were the following: pregnant women, people who are taking prasugrel or ticlopidine, people who are taking proton pump inhibitors, or people who have stopped treatment with proton pump inhibitors for 1-7 days before starting treatment with CLO and history of CLO allergy (Fig. 1). This study was approved by the Ethics Committee of UANL and registered under the resolution number C414-004. Informed consent was obtained from all patients.
Genotyping
Blood samples were collected in tubes containing EDTA, and DNA was extracted using Wizard® Genomic DNA Purification Kit (Promega, Madison, WI, USA). DNA quality was assessed according to standard spectrophotometrically procedures using a NanoDrop spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA). Genomic DNA was genotyped for the polymorphism CYP2C19*2 (681G>A, dbSNP rs4244285) using real-time polymerase chain reaction (PCR) (quantitative polymerase chain reaction [qPCR]) and Taqman® probes (Applied Biosystems; Thermo Fisher Scientific, Inc., HS) according to the manufacturers protocol. StepOne System (Applied Biosystems; Thermo Fisher Scientific, Inc.) was used to perform the real-time PCR, and data were analyzed in the SPSS v20 software (IBM Corp., Armonk, NY, USA). The call rate was >99% in the qPCR experiment.
Platelet aggregometry
P2Y12 reaction unit (PRU) levels were measured utilizing the VerifyNow P2Y12 assay (Accumetrics, San Diego, CA, USA). This method was used to assay patients platelet reactivity to antiplatelet medication with CLO. Platelet antiaggregation was determined after a maintenance dose of at least 75 mg/day for a period of not less 9 days.
Statistics
KolmogorovSmirnov test was used to determine the distribution of the numerical variables (normal or not normal), and a parametric test was performed with Students t-test for comparison of means. The level of significance was established at a value of p less 0.05. Analysis was conducted using the Statistical Package SPSS v20 Software (IBM Corp., Armonk, NY, USA) and GraphPad Prism v6.0 (La Jolla, CA, USA).
Results
One hundred and two patients were included in the study and their demographic characteristics are summarized in Table 1. The mean age was 68 years, and 62.7 % were male; the risk factors among our population were: 57.8 % showed hypertension, 35.3 % showed diabetes mellitus, and 53.9% showed dyslipidemias at the sample collection moment.
Table 1 Population characteristics
| Characteristics (n = 102) | n (%) |
|---|---|
| Male | 64 (62.7) |
| Female | 38 (37.3) |
| Age mean (range) | 68 (35-91) |
| Obesity | 30 (29.4) |
| Smokers | 29 (28.4) |
| Dyslipidemia | 55 (53.9) |
| Hypertension | 59 (57.8) |
| Diabetes mellitus | 36 (35.3) |
| Acute myocardial infarction | 28 (27.4) |
| Unstable angina | 10 (9.8) |
| Stable angina | 42 (41.1) |
| Transient ischemic attack | 5 (4.9) |
| Supraventricular tachycardia | 11 (10.7) |
| Neurocardiogenic syncope | 8 (7.8) |
| Heart block | 4 (3.9) |
| X syndrome | 3 (2.9) |
| Hypothyroidism | 5 (4.9) |
| Prostatic hyperplasia | 5 (4.9) |
| Dyspepsia | 11 (10.7) |
| Cancer | 4 (3.9) |
n: sample size; %: percentage.
Genotype
A total of 102 patients from Northeast Mexico diagnosed with high risk of cardiovascular disease were genotyped for CYP2C19*2 (681G>A, dbSNP rs4244285). The genotype frequencies obtained were 74.5% (G/G), 21.6% (G/A), and 3.9% (A/A). Patients were categorized by CYP2C19 metabolizer status based on *2 genotypes using the common consensus star allele nomenclature as normal metabolizer (G/G), intermediate metabolizer (G/A), and poor metabolizer (A/A), respectively (Table 2)8.
CLO response
According to the aggregometry results, the patients were classified into three groups. Group 1: 47 patients (46%) were classified as good responders, with a PRU level ≤ 194 evidencing a > 40 % block of the P2Y12 receptor; Group 2: 28 patients (27.5%) with a PRU level of 194-235 (20 to 40% of P2Y12 receptor blocking), classified as intermedium responders; and Group 3: 27 patients (26.5%) with ≥ 235 PRU less 20% of P2Y12 receptor blocking) as poor responders.
Genotype/phenotype
Most of the patients with PRU levels less 235 presented the G/G homozygous genotype for the CYP2C19*1 wild-type isoform. In contrast, patients who presented ≥ 235 PRU levels presented the SNP CYP2C19*2 in at least one allele (G/A or A/A). This finding denotes that CYP2C19-reduced enzymatic function shows a significant difference (p = 0.003) when compared to the enzymatic activity of CYP2C19 wild-type isoform in CLO activation (Fig. 2).
Discussion
CLO has very special and complex pharmacodynamic characteristics, including first pass hepatic metabolism, variation in absorption, drugdrug metabolism, and SNPs in the enzymes responsible for CLO metabolism. As a result, a very variable and unpredictable inter-individual response to this therapy is observed favoring the treatment failure. The estimated resistance to CLO fluctuates between 4 and 30%11. In our specific population, the biomarkers necessary for the measurement of resistance to this therapy have not been explored.
This study describes the CYP2C19*2 (681G > A) presence in a group of patients with high cardiovascular risk from the northeast area of Mexico with genotype frequency of 74.5% for G/G, 21.6% for G/A, and 3.9% for A/A. The allele CYP2C19*2 was present in 25.5% of the patients, with a 3.9% of homozygous genotype among patients. This finding is in agreement with a previous study performed in a sample of 51 Mexican mestizo patients from the central region of Mexico with a 17% genetic frequency and 3.9% of the patients having A/A in a homozygous fashion12.
CYP2C19*2 accounts for 75-85% of the alleles responsible for the poor metabolizer phenotype in Caucasians and East Asians13. This allele is significantly more frequent in East Asian populations (14-39%) than among Caucasians (8-16%) and Africans (18-25%)13. However, in Koreans, the frequency of CYP2C19*2 is reported to be 28%, similar to 27% in the Japanese population, but showing a large difference from the Chinese population13. CYP2C19*2 transmission pattern has been observed how an autosomal recessive and autosomal codominant traits14,15.
According to the results of the aggregometry, 46% of the patients were classified as good responders, 27.5% showed of 20-40% of the P2Y12 blocking effect, and 26.5% were classified as poor responders. This observation agrees with the reported by Viveros et al., 2016, where 40% of the patients were good responders while 60% of the patients were non-responders12. Most of the patients (98.6%) with the G/G genotype presented PRU levels less 234 were classified as responders. In contrast, carriers of at least one A allele (G/A and A/A) showed a PRU ≥ 235 indicating less 20% blocking effect of the P2Y12 and were classified as resistant or non-responder patients. Discrepancies in response to drugs are partially due to polymorphisms in genes involved in drug metabolism and transport. Furthermore, it has been shown that the frequency, pattern, and impact of these polymorphisms vary among populations16,17.
The principal problem that physicians face when prescribing antiplatelet agents is the lack of a standardized method for the antiplatelet function. In addition, a cut-point for this function to provide a clear patient classification as responder or non-responder to CLO treatment has not been established18.
The resistance to CLO can be classified as clinical or laboratory-based resistance. Clinical resistance could be defined when a cardiovascular event happens in an individual who is currently receiving the antiplatelet treatment. Meanwhile, the laboratory-based resistance is defined as the in vitro failure of the platelet block activity of an individual who is currently under CLO treatment17.
Several laboratory methods have been proposed for the diagnosis of CLO antiplatelet resistance, yet all of them present advantages and disadvantages18. The big variability reported in the levels of resistance to CLO is due to the absence of a unified definition of the current laboratory tests and to the heterogeneity in the different study groups and protocols.
The results observed in this cohort reflect the importance of both the genotype game of CYP2C19 and the platelet aggregation test as an important predictor to the response and resistance to CLO in patients with high cardiovascular risk.
The prevalence of reduced CLO effectiveness is associated with the presence of CYP2C19*2 polymorphism among patients. This finding denotes that CYP2C19-reduced enzymatic function show a significant difference (p = 0.003) when compared to the enzymatic activity of CYP2C19 wild-type isoform in CLO activation.











 nueva página del texto (beta)
nueva página del texto (beta)