Introduction
The transradial approach for percutaneous coronary interventions (PCIs) has shown some benefits compared to the transfemoral approach1. These include fewer vascular events2, fewer bleeding complications, lower mortality, and earlier ambulation3,4. These factors favor the transradial approach over the transfemoral approach5. However, some factors make the transradial approach a less favorable option for treating coronary arteries. Such factors include: the tortuosity of arm and forearm arteries, a longer learning curve and artery spasms that can complicate, delay and impede coronary artery interventions6. The latter complication is usually caused by the changing and manipulation of catheters. Typically, both femoral and transradial access requires one catheter to assess each coronary artery and another to treat the affected vessel. Nevertheless, models have shown that femoral catheters used in the transradial approach have a very different catheter landing on the aortic root compared to the transfemoral approach. To this effect, catheter exchange has been related to increased procedural time, contrast use, bleeding, and radial artery spasm7.
We performed a study to evaluate the feasibility of a single catheter to assess and treat coronary arteries.
Methods
Study population
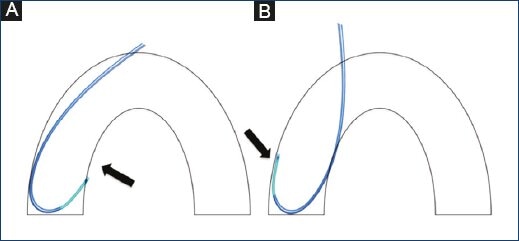
We included 327 consecutive patients undergoing coronary assessment and treatment for whom a single catheter was used for the entire procedure. Patients were enrolled between January 2014 and December 2015. An Ikari left catheter was used (Terumo Medical Corporation, Tokyo, Japan). For patients shorter than 5'6", the Ikari 3.5 cm curve left catheter was used. For patients over 5'6", the 4 cm curve catheter was used (Fig. 1).
Study endpoints and definitions
The primary endpoint was the rate of procedural success and complications. Complications were one or more of the following:
1. Crossover determined as the failure of a single catheter to perform both the angiography and angioplasty.
2. Access site-related injury defined as dissection, stenosis, perforation, rupture, arteriovenous fistulae, pseudoaneurysm, hematoma, compartment syndrome or hemostatic device failure documented either clinically or by imaging studies8.
3. Artery spasm defined as an increase of vascular tone resulting in a difficulty in manipulating the catheter accompanied by pain in the arm of the forearm of the patient. It was considered significant when it prevented the operators from continuing or when the patient suffered considerable pain exceeding five on the verbal numeric scale9.
Procedural considerations
All patients agreed to participate in the study and signed an informed consent form before the procedure whenever possible or after the procedure in emergent cases.
All lesions were evaluated by a group of four interventional cardiologists and were considered significant according to the ACC/AHA/SCAI guidelines10,11.
Catheter manipulation technique
For all cases, a 6- French Ikari Left catheter was used. The catheter was connected to pressure and contrast lines through a "Y" connector. A 0.035-inch J-tipped 110-cm guidewire was directed into the catheter through the "Y" connector, and the whole system was flushed outside the patient with heparinized saline. The catheter was then inserted through the introducer sheath and advanced through the forearm and arm arteries to the aortic root with the "J" Guidewire. The J Guidewire was then retracted into the catheter. For stable elective patients, angiography was started near the non-affected artery. If the affected artery was unknown or if multiple vascular lesions were suspected, angiography was initiated on the left coronary artery (LCA). In the cases of acute coronary syndromes, the procedure was started with angioplasty of the suspected artery.
Left artery cannulation was performed by pushing the J-Guidewire to the aortic valves. Then, the catheter was brought down to the aortic valves, and the guidewire was retracted into the catheter. Subsequently, the catheter was retracted, directed toward the left coronary cusp and then pushed down to bend the curve just to the point necessary to cannulate the left coronary ostium.
Right artery cannulation was performed by pushing the J-guidewire down toward the aortic valves. The catheter was then pushed down and turned clockwise toward the right coronary cusp. Then, the Guidewire was retracted while pushing the catheter at the same time to cannulate the right coronary artery (RCA) (Fig. 2).
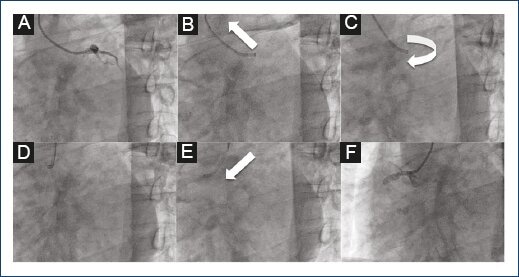
Figure 2 Image which shows the left and right coronary artery cannulation technique. (A-F). Cannulation of the left coronary artery (LCA) which shows contrast injection into the LCA system (A), retraction of the catheter to the ascending aorta to disengage the LCA (B), clockwise 90' rotation of the catheter to change the tip of the catheter to the contralateral sinus (C), stabilization of the catheter on the aorta will allow continuing with changing of the sinus (D), advancement and simultaneous 90' rotation of the catheter down to the aortic root and the right coronary ostium will place the catheter correctly (E), cannulation and contrast injection into the right coronary artery (F).
Access site evaluation
Clinical follow-up and access site evaluation were performed daily during hospitalization and at discharge. A detailed examination of the puncture area was performed looking for complications such as bleeding, hematoma, ecchymosis, loss of arterial pulse, cyanosis, paleness, or any other change. All changes compared to baseline were registered.
Statistical analysis
Demographic variables such as sex, age, height, and weight were obtained. Diagnosis, clinical presentation, and treated artery information were also collected. Outcomes such as procedural success, arterial spasm, bleeding, and complications were analyzed.
Continuous variables are presented as the mean (standard deviation) or median (25th-75th interquartile range) depending on variable distribution. Categorical variables were analyzed by frequency distribution represented as percentages. Analyses between affected vessels were performed with ANOVA. p less than 0.05 was considered statistically significant. All analyses were conducted using the statistical package SPSS version 19 (IBM, Armonk, NY, USA).
Results
Patients and baseline characteristics
We analyzed 327 consecutive patients who underwent coronary artery assessment and intervention using the transradial approach. Baseline and procedural characteristics of the study population are shown in Table 1. The male sex was predominant, with 70% of all patients (234 males/93 females). The mean age was 63.3 ± 11.1 years. Anthropometric measures revealed a mean height of 165.9 ± 7.7 cm, mean weight of 73.3 ± 11.3 kg, and mean body index of 26.5 ± 3.5 kg/m2. Contrast use was 158.5 ± 60.5 ml. Three vessels were treated in 3% of all cases, two vessels in 32%, and one in 65% of all cases. Procedural success was achieved in 94.5% of all cases performed with a single catheter using the transradial approach. A second catheter was required in 9 cases (2.7%), and crossover to the femoral approach was performed in 9 cases (2.7%) due to lack of support, artery spasm, difficult anatomy, or the need of a larger catheter. Three complications were related to access, including a Class 2 hematoma that was treated conservatively with no further complications. Specific analysis of the treated vessels and ipsilateral and contralateral arteries was performed, with no significant difference observed with fluoroscopy or contrast use among left anterior descending (LAD) + RCA, LAD + circumflex artery (Cx) or RCA + Cx (Table 2). Analysis was also performed in cases of failure to complete the procedure with a single catheter.
Table 1 Demographics, clinical and procedural characteristics of patients
| n (%) | |
|---|---|
| Male sex | 234 (70) |
| Age (years) | 63.3 ± 11.1 |
| Body mass index (Kg/m2) | 26.5 ± 3.5 |
| Contrast use | 158.5 ± 60.5 ml |
| Three vessels treated (%) | 3 |
| Two vessels treated (%) | 32 |
| One vessel treated (%) | 65 |
| Single catheter success (%) | 95.4 |
Table 2 Clinical and procedural characteristics between culprit vessel
| LAD + RCA | LAD + Cx | RCA + Cx | p value | |
|---|---|---|---|---|
| Age | 64 ± 12 | 66 ± 10 | 66 ± 9 | 0.92 |
| Fluoroscopy | 17 ± 9 | 21 ± 12 | 24 ± 16 | 0.63 |
| Contrast (ml) | 163 � 29 | 175 � 37 | 187 � 37 | 0.48 |
LAD: Left anterior descending, RCA: Right coronary artery, Cx: Circumflex artery
Baseline and procedural characteristics among failed procedures with crossover or two-catheter use
A total of 18 patients required two-catheter use or crossover to femoral access. Reasons for two-catheter use included lack of support in nine patients and unfavorable coronary anatomy for the catheter on the remaining six patients. 12 of the 15 patients were male (80%) and their mean age was 71 ± 12.1 years. Anthropometric characteristics included a mean weight of 73.5 ± 12.9 kg, mean height of 163.5 ± 6.7 cm, and mean body mass index of 27.7 ± 3.4 kg/m2. Procedural characteristics included a mean fluoroscopy time of 10.1 ± 5.2 minutes. The mean contrast volume used was 186 ± 83.7 ml. The procedural context was ST-segment elevation myocardial infarction (STEMI) in 9 of 15 patients (60%). 50% of the patients required three-vessel interventions and the remaining 50% required two-vessel intervention. Procedural success with a single catheter was achieved in 312 of the 327 patients (95.4%) (Table 3).
Discussion
Coronary procedures usually require different catheters to evaluate, measure, and treat different lesions. Femoral access may facilitate backup, catheter stability, and adequate control of the lesion.
Most of the problems reported when using transradial access were an inability to access radial artery, arterial spasm, anatomical limitations, failure to cannulate the target vessel, and inadequate catheter support12.
The incidence of crossover due to spasm or anatomy abnormalities is reported to be approximately 3.9%. Some factors that cause an increase of radial artery spasm include anatomical abnormalities, young age, female gender, therapeutic procedures, pain, procedural time, and the use of three or more catheters13.
Dehghani et al. showed a procedural failure of 4.7% during 2,100 transradial procedures with a total of 1.2 ± 0.6 catheters used for successful procedures versus 1.4 ± 0.6 catheters for failed procedures when treating the RCA and 1.2 ± 0.6 catheters for successful procedures versus 1.6 ± 1.0 catheters for failed procedures when treating the LCA. During transradial failures, operators used six and seven catheters for RCA and LCA, respectively, before crossover to TF14.
Some factors have been studied associated with PCI failure. They have been described as a failure of arterial access, inability to advance the catheter into the ascending aorta and inability to complete the PCI due to lack of guide support. 13% of the cases had an inadequate arterial puncture. Among cases of failure to advance the catheter into the ascending aorta, 34% of patients had radial artery spasm, 10% had radial artery loop or tortuosity, 6% had radial artery dissection, and 1% had radial artery stenosis. Failure to complete PCI due to lack of guide support was due to subclavian tortuosity in 18% and inadequate guide backup support in 17%.
The importance of catheter selection may directly be related to appropriate support, adequate access to coronary ostium, and procedural success15.
An additional backup catheter (Voda, XB, and EBU) may improve procedural success with different modalities. However, there have been limitations with treating left main lesions, short left main with ostial circumflex lesions and right coronary lesions (Fig. 3). The Amplatz right catheter facilitates ostial access to right proximal, mid-, or distal coronary lesions. However, when significant tortuosity is present, it may be difficult to stabilize or advance the catheter. Furthermore, it does not offer adequate support, stability or control when treating the left coronary system. The Amplatz left catheter may provide good support and stability to the RCA and may ease balloon and stent placement. Nevertheless, when treating proximal and ostial lesions, the complexity might increase. In addition, it does not offer good support for interventions of the LCA through the transfemoral approach (Figs 4A-4D).
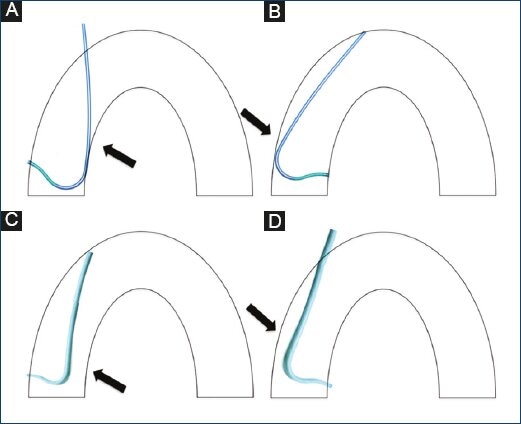
Figure 4 Diagram of the Amplatz left catheter in the right coronary ostium (A), Amplatz left catheter in the left coronary ostium. Note the low one-point support on the contralateral wall. (B) Right Amplatz catheter in the on the right coronary ostium. Note the absence of support on the contralateral wall. (C) Right Amplatz catheter in the left coronary ostium. Note the lack of support on the contralateral wall when performed by the transradial approach (D).
The Judkins traditional JL and JR catheters have good curvature and support for the femoral approach but do not transmit the same force when used in the transradial approach (Figs 5A-5D).
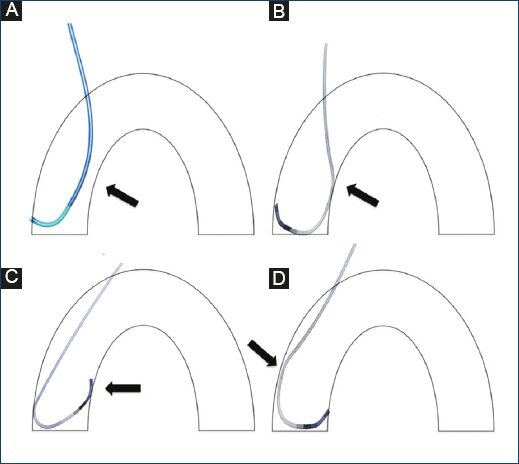
Figure 5 Diagram of the Judkins right coronary catheter in the right coronary ostium. Note the lack of support on the contralateral wall (A). Ikari left catheter in the right coronary ostium (B). Judkins left coronary catheter in the left coronary ostium. Note the absence of a landing zone on the ostium (C). Ikari left catheter on the left coronary ostium. Note the support on the contralateral wall when performed using the transradial approach (D).
Feasibility of single-catheter use for the right and LCAs
Procedural success requires both optimal stent profile and guidewire support. Some principles of guide catheter selection are necessary for successful PCI. Backup support and coaxial engagement are two features of catheter properties necessary for every procedure. Ikari showed that the Ikari L catheter has some modifications from the Judkins L catheter that may facilitate procedures:
1. A shorter length between the third and fourth angles
2. Longer length between the second and first angles
3. A first angle to fit the brachiocephalic artery.
As shown in Fig. 5, these properties improve backup support for the LCA. When used in the RCA, it may be used in a passive way as with the Judkins R. catheter. However, when more force is necessary, the contralateral aortic wall will increase backup support not provided by any other catheters as shown during in vitro studies16.
Benefits of single-catheter use for right and LCAs
Operator dexterity and learning curve have some influence on rates of procedural success, radial spasm, artery dissection, procedural time, and contrast use. However, single-catheter use shows some benefits over the selection of two or more catheters.
For STEMI patients, transradial access has fewer bleeding complications.
Both the total and procedural times are minimized, thus eliminating the catheter exchange time. Therefore, door-to-balloon time is shortened. Fluoroscopy time is reduced because the tip of the catheter always remains over the valvular plane and only clockwise rotation is needed to place the catheter in the coronary ostium.
Radial artery spasm is diminished because the arterial path is minimally manipulated.
Bleeding is low because the system is always closed and no catheter exchange is needed. Finally, after the procedure, it has the benefits of radial access.











 nueva página del texto (beta)
nueva página del texto (beta)