A twenty-seven year-old pregnant female with history of smoking for the last 5 years. In the seventh month of pregnancy began with progressive dyspnea and ankle edema. At her initial evaluation, she had acute heart failure, with bilateral pleural effusion and apex displaced to the 6th intercostal space. On auscultation, systolic murmur was heard in tricuspid and mitral focus grade II/IV radiated to axilla. N-terminal pro-B-type natriuretic peptide was of 14,530 pc/dl. Electrocardiogram revealed sinus tachycardia with heart rate of 110 bpm. The chest X-ray showed cardiomegaly with cardiothoracic index of 0.57, pulmonary venocapillary hypertension, and right pleural effusion. Transthoracic echocardiogram showed dilation of four cavities, global hypokinesia, left ventricular systolic dysfunction with ejection fraction of 31%, and mild mitral and tricuspid regurgitation. A cardiac magnetic resonance imaging (CMRI) corroborated the dilation of the four cavities and also revealed anteroseptal and inferoseptal intramyocardial late gadolinium enhancement (LGE), with the left ventricular ejection fraction of 19% and the right ventricular ejection fraction of 13%, bilateral pleural effusion, and pericardial effusion (Fig. 1), compatible with peripartum cardiomyopathy (PPCP).
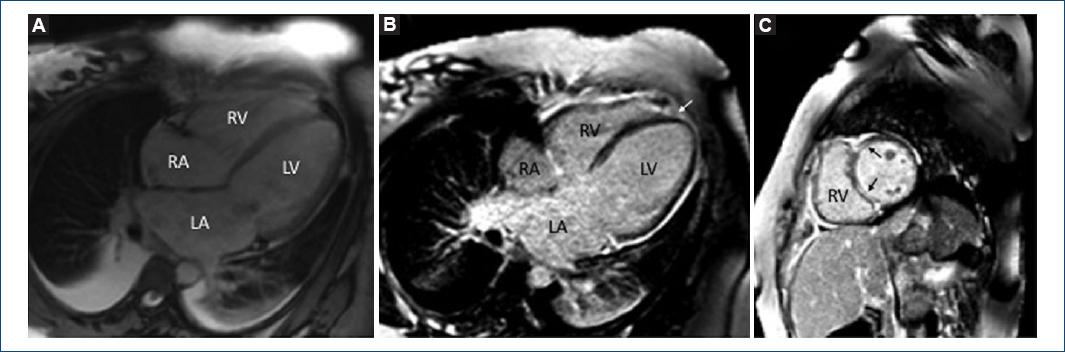
Figure 1 A: Dilation of cardiac cavities, pericardial effusion, and bilateral pleural effusion was observed. B: Four chambers, C: Short axis at the level of both ventricles, showing intramyocardial anteroseptal and inferoseptal (black arrows) late gadolinium enhancement, also in the site of the left ventricular junction with the right ventricle (white arrow).
After 1 year of delivery, she is in NYHA functional Class III, despite complete medical treatment for heart failure.
PPCP has an incidence of 1:100-1:1500. Even though it is more common in women older than 30 years, it has been reported across a wide range of age groups. Most symptoms occur in the context of a normal pregnancy. About 19% of patients may present with symptoms before the past gestational months. It develops during the past 3 months until 6 months after delivery. It must be suspected in a younger age. Among the physiopathological explanations are nutritional deficiency, abnormalities in small coronary arteries, hormonal effects, toxemia, and maternal response to fetal antigen. Clinical follow-up is very variable1-3. LGE seems to be associated with a poor prognosis in the setting of PPCM. CMRI seems to have promising practical implications in the diagnosis and prognosis of PPCM patients. Up to 50% of cases show complete recovery of the left ventricular systolic function after 6 months of delivery, but the other 50% develop progressive dilation and ventricular dysfunction that leads to premature death due to heart failure4,5. In our patient, CMRI demonstrated LGE, a parameter of poor prognosis and she is in chronic heart failure.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 nueva página del texto (beta)
nueva página del texto (beta)


