Background
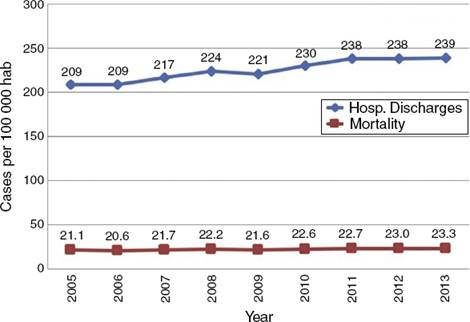
Mexico is a federal republic in North America, with a population of 121 million distributed in almost two million square kilometers.1 It has an estimated gross domestic product (GDP) of USD $1.3 trillion (purchase power parity), a gross national income (GNI) per capita of USD $9870 and a minimal daily salary of USD $5.82,3. The Mexican population is becoming older, with an average life expectancy of 74.5 years and an aging-index value of 31 old people per 100 young.4,5 In addition, there are 60 economically-dependent individuals per 100 productive-aged people.6 Cardiovascular diseases (CVD) are the main cause of mortality and disability in Mexico and worldwide. Every year, more than 17 million people die and more than 393 million of disability-adjusted life-years (DALYs) are lost due to CVD.7,8 In Mexico 109,309 people died due to CVD and the mortality rate is still rising (Fig. 1).9,10 Unfortunately, 92% of all CVD deaths happened before the patients could get to hospital.11 Every year, around 250,000 patients are discharged from hospital after a CVD hospitalization.12 Mexican authorities reported more than 3.3 million DALYs, higher than World Health Organization average (2.3 million). That represents a loss of USD $61 billion of GDP.13 Fifty-three percent of Mexicans have social security (IMSS 43.4 million, ISSSTE 8.3 million, SEDENA-SEMAR-PEMEX (2 million), 9 million have a private insurance, and the rest are protected by ‘‘Seguro Popular’’ (51.1 million). In 2012, Mexico assigned 6.2% of its GDP to health-care services, the third lowest proportion in the world according to the Organization for Economic Co-operation and Development (OCDE, the world average is 9.3%). Every year, university hospitals train more physicians and experts in several specialties, but this number remains below the OCDE standard.14
Cardiac rehabilitation and prevention programs (CRP), are worldwide recommended by several associations and colleges of cardiology. The target population (class I-A recommendation) are basically those individuals with atherosclerosis, heart failure, myocardial infarction, peripheral artery disease, chronic stable angina and finally patients who underwent to myocardial revascularization procedure (PTCA or CABG).15–27 In Mexico, CRP-programs were initiated in 1944 by Prof. Nicandro Chávez at the National Institute of Cardiology.28 From then new CRPs appeared and others vanished. In 2009, the first National Registry of Cardiac Rehabilitation Centers (RENAPREC) showed us, for the very first time how these centers operate.29 At that time there were only 14 CRP-units to treat more than 200,000 patients that survived a cardiovascular event every year. The aim of this paper is to compare several aspects of the results published in RENAPREC with new data obtained in 2015. We shall focus on assistance, training of health-providers and research. Furthermore, this article evaluates the barriers that inhibit CRP development.
Methods
RENAPREC-2015 is a descriptive study of CRP units in México. This second survey intended to include every single CRP center, and the recruitment strategy was as follows: first, all authors of RENAPREC-2009 were requested to participate. Second, all former students that had graduated from the cardiac rehabilitation post-degree program (Medicine Faculty, National University of Mexico, UNAM) were also invited. Cardiac rehabilitation leaders that regularly participate in academic activities of the Mexican Society of Heart Care (SOMECCOR) or the Mexican Society of Cardiology were also contacted. Then we performed an internet search to find other centers that were advertised online, and an email was sent asking them to take part in this research. Finally, we included all CRP units that were directly recommended from other centers.
Selection criteria for CRP units
We included all Mexican centers that answered the request and completed the research questionnaires. All incomplete reports were disqualified. There were open and closed questions covering several subjects about CRP. Questionnaires were sent by email or undertaken by telephone as necessary. This information was stored in a database and variables were classified as nominal, categorical, ordinal or numerical as appropriate. These centers were distributed in two groups: RENAPREC-2009 centers that participated in 2015 (n = 10) and the new CRP units (n = 14). These units were compared with RENAPREC-2009 participants (n = 14).
Statistical analysis
The data was processed using SPSS 19 and was presented in the form of frequency (percentage), median (minimum to maximum) or mean (standard deviation) according to variable’s distribution. Chi2 and Wilcoxon range tests were applied. All p values less than 0.05 were considered stochastically significant.
Results
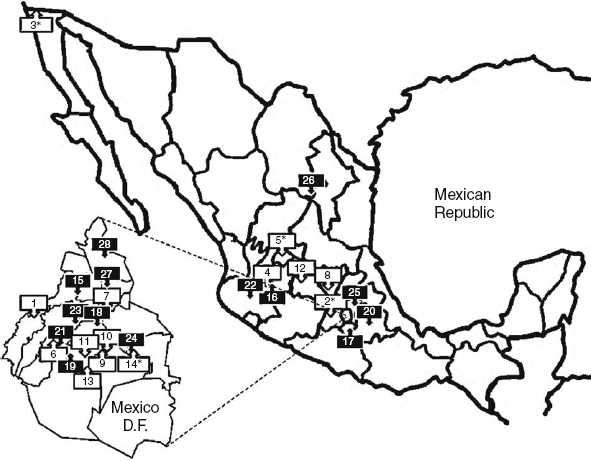
RENAPREC 2015 summarizes information of 24 centers, 10 of them had participated in RENAPREC 2009 (Table 1). Two former centers disappeared; one of them has closed and two were combined to make one. Another two centers did not respond to our calls. General characteristics of CRP-centers are shown in (Table 2). First, the number of units in Mexico increased approximately 71% since 2009, with 4 new public centers and 6 private clinics. The geographic distribution of CRP-units shows a centripetal pattern (Fig. 2).
Table 1 Cardiac Rehabilitation Centers included.
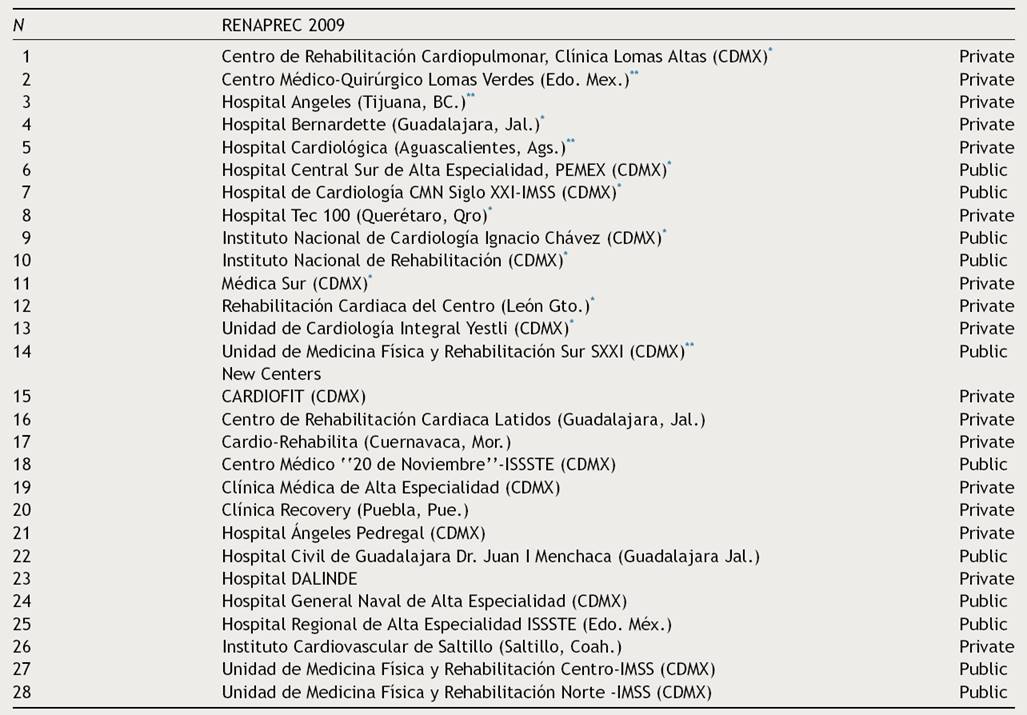
* CRP-centers that have participated in both surveys.
** Centers that were not included in RENAPREC 2015.
Abrev. Aguascalientes (Ags), Baja California (B.C.), Centro Médico Nacional (CMN), Coahuila (Coah), Distrito Federal (CDMX), Estado de México (Edo. Mex), Guanajuato (Gto), Instituto Mexicano de Seguro Social (IMSS), Instituto de Seguridad Social y Servicios para los Trabajadores del Estado (ISSSTE), Jalisco (Jal), Morelos (Mor), Petróleos Mexicanos (PEMEX), Puebla (Pue), Querétaro (Qro).
Table 2 General characteristics of CRP units included.
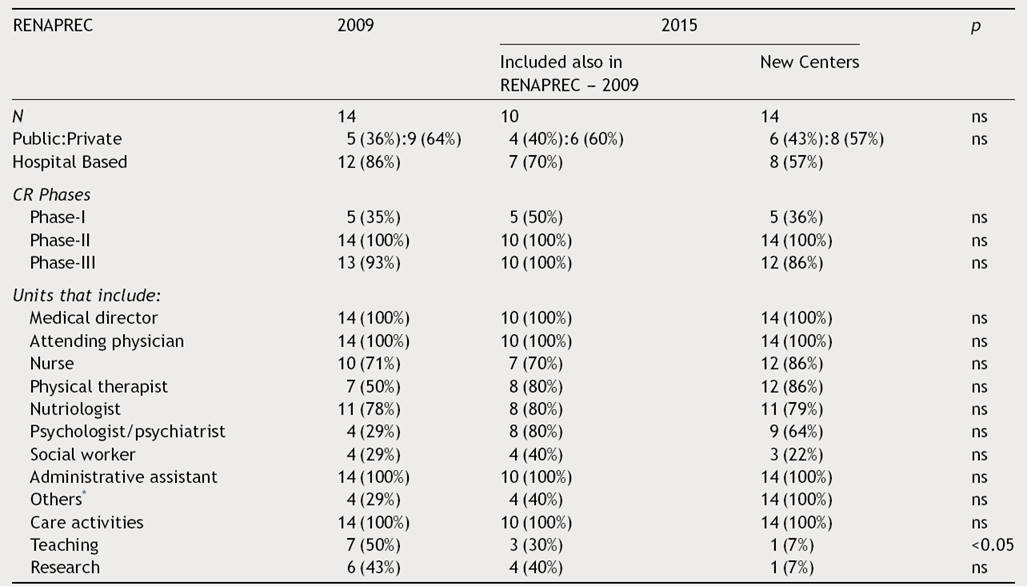
Compared data from RENAPREC-2009 vs. RENAPREC 2015, composed with centers that were included in 2009 and participated again in this survey, plus 14 new centers.
* Respiratory therapist, resident doctor, sport medicine, endocrinology, electrodiagnostic technician.
All centers had a director who was a cardiologist post-graduate in cardiac rehabilitation (67%), clinical cardiologist (17%), physiatrist (12%) or sports medicine specialist (4%). Twenty-one directors (87%) were certified as specialists (Cardiology or Rehabilitation Medicine), and 76% of them also had a specific cardiac rehabilitation certification.30
The Mexican Council of Cardiology has certified 2549 clinical cardiologists, 422 hemodynamic specialists, and 27 cardiologists with a postgraduate degree in cardiac rehabilitation (UNAM). Thus, the ratio of Clinical Cardiologists to Cardiac Rehabilitation Specialists is 94:1, and the ratio of Intervention Specialists to cardiac rehabilitation experts is 16:1.30 In this study, the coverage of CRP-units was 0.02 centers per 100,000 inhabitants.
In Mexico, 11,648 patients were included in a CRP-program in 2014. That represents only 4.4% of eligible patients (254,957 discharges/year). The activities performed by CRP-units and the general characteristics of the patients are summarized in (Fig. 3) and (Table 3) respectively. The time between hospital discharge and the beginning of phase II became shorter in 2015 compared to 2009 (18 vs. 30 days), and the number of new patients attended, increased from 3.2 to 10.4 patients/100,000 inhabitants in 2015. Patients have attended more than 90% of phase-II sessions.
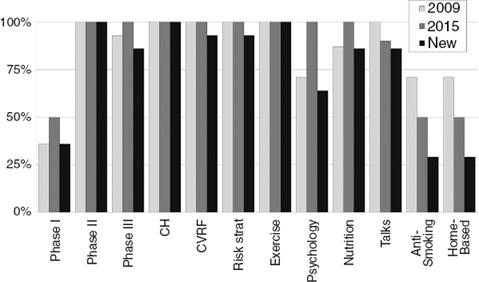
Figure 3 Cardiac Rehabilitation Care Activities (% of CRP Centers). Abbrev. Cardiovascular risk factors control (CVRF), clinical history (CH), home-based cardiac rehabilitation (Home-Based), risk stratification process (Risk Strat), secondary prevention lectures (talks).
Table 3 General characteristics of patients.
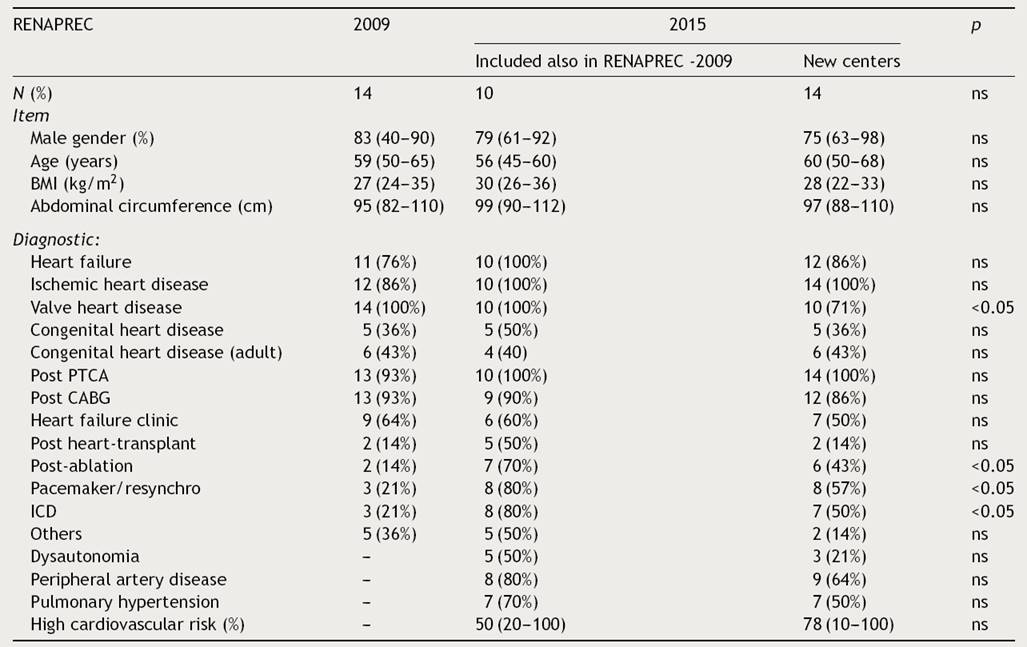
This table shows the demographics of patients treated in CRP programs in 2009 vs. 2015.
Abbrev. Body mass index (BMI), coronary artery bypass graft (CABG), implantable cardiac-defibrillator (ICD), percutaneous transluminal coronary angioplasty (PTCA), resynchronization electrotherapy (Resynchro).
Patients’ risks were classified using several stratification methods like the Framingham Risk Score (85%), the Heart Score (71%) and the ASCVD-2013 score (46%). Home-based exercise training was applied by 38% of the CRP units, and 45% of centers offered a follow-up over a period longer than a year. A clinical history, identification and control of cardiovascular risk factors and physical training programs were performed by all CRP units. Basic and advanced life support programs were implemented in 96% of CRP-units, with qualified staff in 92%. However, only 42% of centers regularly undertake BLS-ACLS training to keep their skills ready-for-service. The physical training characteristics are displayed in (Fig. 4).
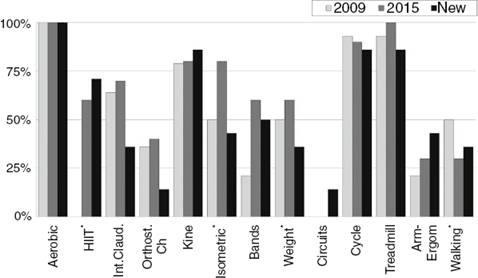
Figure 4 Exercise Training Modality (% of CRP Centers). Abbrev. Arm-ergometry (Arm-Ergom), cycle-ergometry (Cycle), high intensity interval training (HIIT), intermittent claudication (Int. Claud.), kinesiotherapy (kine), orthostatic challenge (Orthost. Ch), rubber bands (bands), weight lifting (weight). Stochastic differences with a p value less than 0.05 (*)
Cardiac rehabilitation costs in Mexico varied from USD $600 to USD $3400, and were covered by private insurance (4%), patients (8%), social security (8%), the government (20%) or mixed models (60%). Only 50% of CRP units in 2015 have a specific program for business-administrative guidance and few have control systems in place or under-take auditing. There were 4 training centers for human resources (16%) and UNAM has offered a postgraduate degree in cardiac rehabilitation for cardiologists since 2007, and for physical therapists since 2013. There are 27 cardiologists with a postgraduate degree in cardiac rehabilitation, and 22 of them are still working at CRP units. Only 21% of CRP-units researching lines in exercise testing, physical training, risk factor control, ischemic heart disease, heart failure, cardiac transplantation/ventricular assistance devices, congenital heart disease, and complexity sciences, among others.
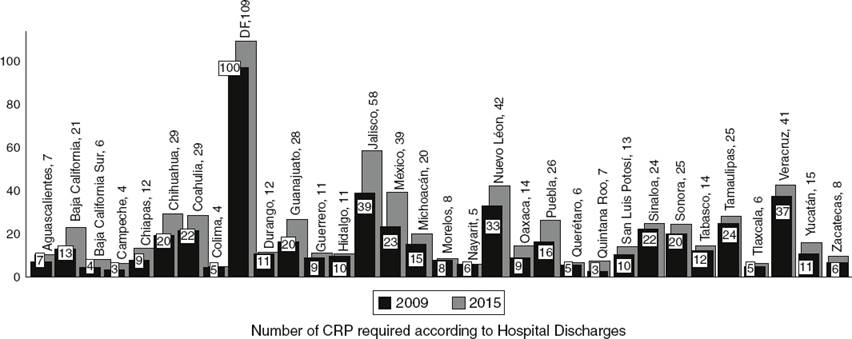
It is generally observed in Mexico that cardiac rehabilitation is hampered by several barriers like financial crisis (83%), lack of skilled personnel (67%), deficient equipment (46%), inadequate areas (42%) and a reduced number of operating centers (38%). Eighty-three percent of the CRP-unit medical directors stated that clinical cardiologists at hospitals do not send eligible patients to the cardiac rehabilitation centers because they are not aware of the available units. In Mexico, 640 CRP-units are needed to attend to the quarter of a million patients who are discharged from the hospital every year (Fig. 5).
A final report of patient’s activities and testing results are sent to the referring physician in 87% of all centers. Electronic information is remarkably underused in CRP-units; only 29% of centers utilize email and only 21% use social networks. Only 8% of all centers have a website, and none use telemedicine programs.
In Mexico, patients have to wait 33 ± 24 days to start a CRP-program. Patients’ adherence is about 86% ± 14% of phase-II sessions, and the patient’s dropout rate is around 12.8 ± 13%. The main causes of lack of attendance were remoteness (38%), financial troubles – need to work (42%), comorbidity (17%), lack of family support (17%) and incompatibility of schedule in 38%.
Discussion
RENAPREC 2015 is the second national register of cardiovascular rehabilitation and prevention centers in Mexico. Although two former centers have closed, the number of CRP-units grew 71% during the last 6 years, and the total coverage increased more than 7 fold. For many reasons nowadays there are much more kinds of cardiovascular pathology in Mexico and patients with these conditions could benefit from CRP-programs. Cardiac rehabilitation in children with congenital heart disease is a specialty that has been recently developed in our country.
While all centers offered rehabilitation services, less than a half undertook teaching and research activities. Also, the way to perform cardiac-rehabilitation activities varies widely from one center to another. The educational system for cardiac rehabilitation professionals is maturing; whereas previously the knowledge of such workers went unrecognized in the educational context, they now study in the framework of university-recognized curricula which is certified by the Mexican Council of Cardiology.
However, the growth in the number of centers remains insufficient to cover the actual needs of the Mexican population. More than two thirds of Mexico does not have any CRP-center, especially in northern, southeastern and coastal states. Furthermore, the most important problem is that the referring of patients to CRP-programs is very low (<5%), because of ignorance or due to distrust. There are more private than public CRP-units, but insurance companies do not regularly cover this type of therapy. In Mexico, the costs for the patient are high mainly due to the relatively high initial cost for investment in modern technology. Furthermore, operating expenses contribute to this burden, against a very low number of referred patients.
Mexicans need an improvement in cardiac rehabilitation and prevention programs. To achieve this goal, it is mandatory that our group promotes a national legislation on this topic, restructures the corresponding specific guidelines, procedures and obtains financial funding. It would be useful to have a new National Registry of Patients in Cardiac Rehabilitation and Prevention Programs so physicians could have accurate records for detailing patients’ condition and statistics to provide an overall picture of the national CVD situation. For example, the Mexican Institute of Social Security (IMSS) is working on a program to develop institutional cardiovascular rehabilitation and prevention. For this purpose, IMSS managers are modernizing older centers, creating eight new CRP units and finally inviting cardiac rehabilitation centers to adopt a national program centered on an ‘‘Infarction-Code’’ program.
Study limitations. Not all CRP-units that operate in Mexico responded to the invitation to partake in this survey, mainly due to their lack of interest. We also think that, several centers do not provide the minimum quality standards and so their managers decided to avoid this questionnaire. Another limitation is that RENAPREC information is obtained directly from every head of department, and not from an ad-hoc multicenter database. So there may be questions regarding the reliability of these data because it depends on the opinions of the medical directors.
Conclusions
Cardiac rehabilitation programs in Mexico have existed since 1944 and they are still in the process of maturing. Mexican CRP-centers have several strengths like the quality of the education of professionals, the multidisciplinary programs, the guideline-implementation and a national society that leads and instructs the team co-workers. However, the lack of reference of patients and the heterogeneity of procedures are still their main weaknesses. Furthermore, as the rest of the world, the most important barrier that CRP-programs have is their underuse. This problem may lead to a higher mortality rate, a poorer quality of life and more expensive health services for the patients that survive a cardiovascular event.











 nueva página del texto (beta)
nueva página del texto (beta)