Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos de cardiología de México
versión On-line ISSN 1665-1731versión impresa ISSN 1405-9940
Arch. Cardiol. Méx. vol.85 no.3 Ciudad de México jul./sep. 2015
https://doi.org/10.1016/j.acmx.2015.04.001
Investigación clínica
Third national registry of acute coronary syndromes (RENASICA III)
Tercer Registro Nacional de Síndromes Coronarios Agudos (RENASICA III)
Carlos Jerjes-Sanchez, Carlos Martinez-Sanchez*, Gabriela Borrayo-Sanchez, Jorge Carrillo-Calvillo, Ursulo Juarez-Herrera, Juan Quintanilla-Gutierrez
Executive Committee of RENASICA III, Mexico.
* Corresponding author at:
Instituto Nacional de Cardiologia "Ignacio Chávez",
Calle Juan Badiano 1, Tlalpan, Sección XVI, 14080
Ciudad de México, Distrito Federal, Mexico.
Tel.: +52 55 5573 2911.
E-mail address: carlos.martinez@cardiologia.org.mx (C. Martinez-Sanchez).
Received 3 October 2014
Accepted 22 April 2015
Abstract
Objective: RENASICA III is a prospective, multicenter registry on acute coronary syndromes (ACS). The main objective will be to identify the outcome in tertiary and community hospitals and perform strategies to improve quality of care in Mexico.
Methods: RENASICA III will enroll 8000 patients in public health and private hospitals. The registry began in November 2012 with a planned recruitment during 12 months and a 1-year follow-up. The study population will comprise a consecutive, prospective cohort of patients >18 years with ACS final diagnosis and evidence of ischemic heart disease. The structure, data collection and data analysis will be based on quality current recommendations for registries. The protocol has been approved by institutional ethics committees in all participant centers. All patients will sign an informed consent form.
Currently in Mexico, there is a need of observational registries that include patients with treatment in the everyday clinical practice so the data could be validated and additional information could be obtained versus the one from the clinical trials. In this way, RENASICA III emerges as a link among randomized clinical trials developed by experts and previous Mexican experience.
Keywords: Acute coronary syndromes; ST-elevation myocardial infarction; Non-ST elevation myocardial infarction; Unstable angina; Registries; México.
Resumen
Objetivo: RENASICA III es un registro prospectivo multicéntrico en síndromes coronarios agudos (SCA). El principal objetivo será identificar en México la evolución en hospitales de segundo y tercer nivel para establecer estrategias para mejorar la calidad de la atención.
Métodos: RENASICA III ingresará 8000 pacientes en hospitales de instituciones de salud y privados. El registro inició en noviembre de 2012 con un reclutamiento durante 12 meses y un seguimiento al alta hospitalaria de 12 meses. La población en estudio incluirá una cohorte prospectiva de pacientes >18 años con diagnóstico final de un SCA y evidencia objetiva de cardiopatía isquémica. La estructura del registro, la recolección de datos y el análisis se basó en las recomendaciones actuales para la calidad de los registros en enfermedad cardiovascular. El protocolo fue aprobado por los comités institucionales de ética de todos los centros participantes. Todos los pacientes firmarán un consentimiento informado.
En la actualidad existe en México la necesidad de registros observacionales que incluyan pacientes sometidos a tratamiento en la práctica clínica contemporánea para validar los datos y obtener información complementaria de los grandes estudios aleatorizados controlados. RENASICA III emerge como un vínculo entre estudios aleatorizados controlados conducidos por expertos y la experiencia mexicana previa.
Palabras clave: Síndromes coronarios agudos; Infarto del miocardio con elevación del ST; Infarto del miocardio sin elevación del ST; Angina inestable; Registros; México.
Introduction
In the last decades, ischemic heart disease and acute coronary syndromes (ACS) remain part of chronic degenerative diseases. In developed and less developed countries they could be seen also as an expression of demographic and epidemiological transition with a deep impact in terms of mortality, quality of life and resource use. In countries with strong economies and capacities, mortality reduction has been achieved through changes in socioeconomic status, risk factors control, effective treatments and resources that translate clinical studies results into clinical practice. Recent evidences from GRACE and CRUSADE registries show that guidelines compliance improves the outcome of ACS patients.1
In Mexico, the first national registry of acute coronary syndromes2 (RENASICA I) identified epidemiologic characteristics, therapeutic trends and risk stratification. Through the second national registry (RENASICA II3), RENASCA4 and ACCESS5 registries, previous observations were confirmed and better therapeutic approaches and high-risk groups were identified.6,7 A substudy of RENASICA II8 showed similar antithrombotic treatment compliance compared with CRUSADE in non-ST elevation ACS patients. As an interesting observation, no difference in mortality among Mexicans (4%), Hispanics (4%) and White (5%) patients was observed.
Considering previous evidences in Mexico,3–8 time reduction between onset of symptoms and first hospital contact (>3.5 h), increased pharmacological (<35%) and mechanical (<10%) reperfusion and more patients under fibrino-specific lytic agents and better anticoagulation is a challenge. However, in spite of long ischemia times and low access to reperfusion approaches, in-hospital mortality (10%,3 8%,4 2%5) remains low probably due to an underestimation of the total deaths in our tertiary centers and lack of follow-up at discharge; as a consequence of all this process ventricular dysfunction (17%,3 39%4 and 30%5) was the most frequent in-hospital complication. Similar results have been observed in developed countries.5 RENASICA III intends to identify a high-risk stratification, diagnosis and treatment approaches in community and tertiary hospitals to optimize resources and to define strategies to improve quality of health care.
Methods
Registry design
RENASICA III is a prospective, multicenter registry on ACS male and female patients. The project is an initiative of the Mexican Cardiology Society supported by Sanofi and it was designed to obtain a sample free of trends with statistical impact. The main objective will be to identify outcome in tertiary and community hospitals and perform strategies to improve quality of care. The registry is planned to enroll 8000 patients from public health and private hospitals.
The registry began in November 2012 with a planned recruitment during 12 months and 1-year follow-up (Figure 1). The protocol has been approved by institutional ethics committees in all participant centers. The registry will be conducted in accordance with the Declaration of Helsinki, International Conference on Harmonization-Pharmaco-Epidemiology and Good Clinical Practices. National requirements coming from COFEPRIS will be considered as well. As an observational registry, no specific treatments, tests, or procedures will be mandated or withheld from the patients; participants will be free to withdraw from the registry at any time. All patients will sign an informed consent.
Study population
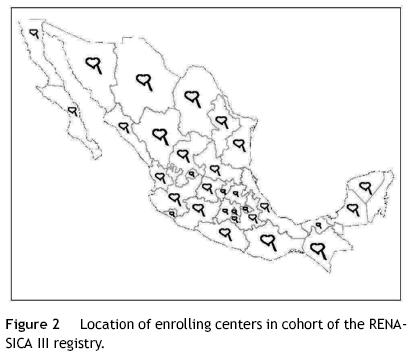
The study population will comprise a consecutive, prospective cohort of patients >18 years with ACS final diagnosis and objective evidence of ischemic heart disease. Patients admitted to emergency departments, coronary care units, intensive care units, hospital and hemodynamic laboratories with high clinical suspicion and subsequently proven diagnosis will be eligible. The initial diagnosis will be established by physician in charge based on clinical and electrocardiographic findings in all cases. The structure, data collection and data analysis were based on current quality recommendations for registries.9 ACS nomenclature will be standardized at admission and for epidemiologic reasons unstable angina or infarction at discharge. Principal investigators will be selected in community and tertiary hospitals with a geographical distribution covering the entire country (Figure 2).
Objectives
Primary: To identify clinical diagnostic and therapeutic characteristics in Mexico. Secondary: (a) to assess adherence to guidelines for diagnosis and treatment of ACS; (b) to identify issues and establish health system strategies to improve patient care; (c) to identify standards of acute and in-hospital patient care in participating centers; (d) to propose therapeutic approaches according to available resources and technology; (e) establish accessible risk stratification in ACS through mortality predictive variables observed in RENASICA II.3
Patient screening
All patients with high-clinical suspicion of ACS will be included through risk factors, chest pain symptoms and ECG findings. At the beginning four groups will be considered based on ST segment electrocardiographic findings: normal or unspecific ECG, ST depression, transient ST elevation,10 or persistent ST elevation. At discharge objective evidence of ischemia by invasive or noninvasive testing must be proved. Patients with secondary ischemia (anemia, pulmonary embolism, myocarditis, and etcetera) and type II infarction will not be included.
Quality criteria
The following criteria will be used to improve quality data: (a) standardized definitions, data and reports; (b) tools for immediate feedback; (c) meetings among the scientific and executive committee; (d) ethics procedures review; e) electronic, simple and accessible data collection; (f) randomized centers selection; (g) consecutive patients enrollment to obtain representative sample; (h) random centers audit; (i) centralized data and statistical analysis; (j) report all data and consistent conclusion; and (k) transparency of funds for any publication.9 Furthermore, the quality of this registry will also be measured by the number of publications and presentations in national and international meetings as previously done.11
Follow-up
Clinical adverse events, therapeutic approaches and revascularization procedures will be included (Figure 1). The standardized definitions can be explored in Appendix A.
Data collection
Data will be sent to the registry coordinating center through a web site addressed at http://www.renasica.mx/. All patients will have a unique personal identification to ensure their anonymity. A simple format to facilitate data entry using the most relevant variables of previous registries will be used.3,4 Electronic case report forms will be reviewed by the coordinating center to determine data quality and to generate queries that will be sent to each center. All participating institutions will have regular access to a data entry clerk; to ensure data quality, monitoring will be randomly made in 20% of the centers.
Technical support
Ongoing programs to update, maintain, and improve the electronic database have been established. Every center will have a timely provision of case report forms. Training meetings will be scheduled for electronic database and definitions. The coordinating center will have a 01–800 number to provide technical advice online. Monthly newsletters with statistical reports of the main variables will be coordinated by the executive committee. Follow-up by telephone contact visit will be achieved through coordinating center. In specific cases, follow-up will be made by the physician in charge. Monthly cleaning database will be scheduled for a correct and expeditious final analysis. The system has searching tools by criteria and generates reports plotted in real time.
Training strategies to improve care
The executive and scientific committees will coordinate workshops to standardize care process in first contact area patients.
Publications policies
Executive committee established appropriate guidelines to allow all investigators an expedited process for publication or presentation at national and international meetings following the appropriate channels.
Sample size determination
Risk stratification in ACS patients has shown high prediction of major cardiovascular events. According to the findings of RENASCA4 50% of patients do not receive adequate treatment, and only 8% of patients have percutaneous coronary intervention (PCI), leading to 30% of left ventricular failure as a complication. In RENASICA II3 only 15% of patients received PCI and 17% had left ventricular failure as a complication. This difference will allow us to calculate the smaller sample size for this outcome: statistical power 80%, alpha value 0.05, delta value 13%, relationship between exposed and unexposed 1:1, confidence interval (CI) 95%. It will require 182 patients per group, plus 20% loss yields 220 patients per group. Lower delta value for mortality of 2% requires 3975 patients treated and not treated with PCI. This implies that the registry requires 8000 subjects to be included.
Statistics
Differences between continuous variables with normal distribution will be examined by Student's t test. The test of Wilcoxon rank sum will be used when continuous variables have failed in normality tests. To analyze categorical variables X2 will be used by Fisher's exact test or Yates correction. A two-tailed test with a p value ≤0.05 will be considered as statistically significant. Logistic regression analysis will be used to select independent predictors in those variables that by univariate regression analysis had obtained a p ≤ 0.05. To avoid confusion, through logistic regression the relationship between historical variables for atherosclerosis and cardiovascular events will be examined. With the Cox proportional risk multivariate model will assess the relationship between each of these variables. Kaplan–Meier survival curves to cumulative survival curves for the risk of mortality and differences between the curves for significance by the log-rank statistic. The Cox proportional risk model will be used for adjusted survival analysis. A p value ≤0.05 will be considered as statistically significant. Data will be expressed as percentages, mean, standard deviation, odds ratio and confidence interval (CI) 95%.
Considerations
In Mexico, ischemic heart disease is being the leading cause of death in the elderly and second in the general population. In 2011, ischemic heart disease was responsible for 71,072 deaths, accounting for approximately 11% of all deaths in Mexico.7 The RENASICA III registry will describe the management and clinical outcomes of a cross section of patients with a broad clinical spectrum of ACS in real-life practice. Data will be collected from newly diagnosed patients with ACS irrespective of whether they were receiving any reperfusion approach and will offer insights into outcomes of non-reperfused patients. Considering previous evidence from RENASICA II,3,8 RENASCA4 and ACCESS,5 we are able to know the epidemiologic characteristics, therapeutic trends and risk stratification in the last decade. Currently, it is important to identify if more invasive and pharmacologic reperfusion are used in STMI and compliance guidelines in terms of anticoagulation and antithrombotic treatment. Additionally, it will be interesting to know the role of new antiplatelet agents (prasugrel and ticagrelor) in the setting of ACS. In the transition of therapeutic approaches of ACS, through RENASICA III several questions will be answered: will non-specific fibrinolytic drugs be used in the majority of ST-elevation myocardial infarction? Or unfractionated heparin is the anticoagulant choice?
RENASICA III will show if invasive and pharmacologic reperfusion, anticoagulation and antithrombotic treatment have been improved in ACS patients. In randomized controlled clinical trials of ACS, regulatory authorities mandate very close or strict control of inclusion and exclusion criteria and will be conducted by an expert. This strategy will result in lower rates of in-hospital mortality and bleeding complications than those usually observed in real-life clinical practice. Thus, accurate assessment of reperfusion and antithrombotic approaches is more difficult to reach. Currently, there is, therefore, a need for a national observational registry of patients treated in everyday clinical practice to test the external validity of the trial data and provide complementary information to that from the trials.11 RENASICA III emerges as a link among randomized controlled trials conducted by experts and previous Mexican experience.2–8
Funding
Authors: None. The registry had unrestrictive support by Sanofi-Aventis.
Conflict of interest
The authors declare no conflict of interest.
References
1. Granger C.B., Gersh B.J. Clinical trials and registries in cardiovascular disease: competitive or complementary? Eur Heart J. 2010;31:520-1. [ Links ]
2. Por el Grupo Cooperativo RENASICA. El Registro Nacional de los Síndromes Coronarios Agudos (RENASICA). Arch Cardiol Mex. 2002;72:S45-64. [ Links ]
3. Garcia A., Jerjes-Sanchez C., Martinez B.P., et al. Renasica II. Un Registro Mexicano de los Síndromes Coronarios Agudos. Arch Cardiol Mex. 2005;75: Suppl. 2:S6-19. [ Links ]
4. Borrayo-Sánchez G., Madrid-Miller A., Arriaga-Nava R., et al. Riesgo estratificado de los síndromes coronarios agudos. Resultados del primer RENASCA–IMSS. Rev Med Inst Mex Seguro Soc. 2010;48:259-64. [ Links ]
5. The ACCESS Investigators. Management of acute coronary syndromes in developing countries: ACCESS (ACute Coronary Events – a multinational Survey of current management Strategies) registry. Am Heart J. 2011;162, 852.e22-859.e22. [ Links ]
6. Juarez-Herrera U., Jerjes-Sanchez C., González-Pacheco H., et al. In-hospital outcome in patients with ST-elevation myocardial infarction and right bundle right branch block. Arch Cardiol Mex. 2010;80:154-8. [ Links ]
7. Juárez-Herrera U., Jerjes-Sanchez C. Risk factors, therapeutic approaches, and in-hospital outcomes in Mexicans with ST-elevation acute myocardial infarction: the RENASICA II multicenter registry. Clin Cardiol. 2013;36:241-8. [ Links ]
8. Jerjes-Sanchez C., García B.E., Sanchez C.J.R., et al. Clinical characteristics, process of care, and outcomes among Mexican, Hispanic and Non-Hispanic white patients presenting with non-ST elevation acute coronary syndromes. Data from RENASICA and CRUSADE Registries. Arch Cardiol Mex. 2012;82:14-22. [ Links ]
9. Gitt A.K., Bueno H., Danchin N., et al. The role of cardiac registries in evidence-based medicine. Eur Heart J. 2010;31:525-9. [ Links ]
10. García-Sosa A. Cuál es el mejor abordaje terapéutico en pacientes con elevación transitoria del ST? In: Juan Verdejo Paris, editor. Clínicas Mexicanas de Cardiología. Volumen 4. Planeación y Desarrollo Editorial SA de CV, Publicado por la Sociedad Mexicana de Cardiología, 2012, January. pp. 33-8. [ Links ]
11. Kakkar A.K., Mueller I., Bassand J.P., et al. International longitudinal registry of patients with atrial fibrillation at risk of stroke: global anticoagulant in the field (GARFIELD). Am Heart J. 2011;163:13-190. [ Links ]
12. Jerjes-Sánchez C., Pozas G.G., Ibarra M. Programa para mejorar la calidad de la atención de los síndromes coronarios agudos. Instituto de Cardiología y Medicina Vascular, TEC Salud del Sistema Tecnológico de Monterrey. In: Juan Verdejo Paris, editor. Clínicas Mexicanas de Cardiología. Volumen 4. Planeación y Desarrollo Editorial SA de CV, Publicado por la Sociedad Mexicana de Cardiología, 2012, January. p. 1-22. [ Links ]
13. Quintanilla J., Jerjes-Sánchez C., Barrera F. Programa institucional en infarto con elevación del ST. Instituto de Cardiología y Medicina Vascular, TEC Salud del Sistema Tecnológico de Monterrey. In: Juan Verdejo Paris, editor. Clínicas Mexicanas de Cardiología. Volumen 4. Planeación y Desarrollo Editorial SA de CV,, Publicado por la Sociedad Mexicana de Cardiología, 2012, January. p. 55-68. [ Links ]
14. Sodi-Pallares D, Medrano G, Bisteni A, Ponce de León J, eds. Electrocardiografía clínica, Méndez Editores, 1998. p. 100-32. [ Links ]
15. Sgarbossa E.B., Pinski S.L., Barbagelata A., et al. for the GUSTO-1 investigators. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med. 1996;334:481-7. [ Links ]
16. Thygesen K., Alpert J.S., White H.D. on behalf of the Joint ESC/ACCF/AHA/WHF. Task force for the redefinition of myocardial infarction. Circulation. 2007;116:2634-53. [ Links ]
17. Montalescot G., White H.D., Gallo R., et al. for the STEEPLE investigators. Enoxaparin versus unfractionated heparin in elective percutaneous coronary intervention. N Engl J Med. 2006;355:1006-17. [ Links ]
18. Gibson C.M., Cannon C.P., Murphy S.A., et al., for the TIMI Study Group. Relationship of TIMI myocardial perfusión grade to mortality after administration of thrombolytic drugs. Circulation. 2000;101:125-30. [ Links ]
19. Jerjes-Sánchez C. Pulmonary embolism. From molecular basis to clinical practice. Pulmonary embolism: causes, symptoms and treatment, 1ª ed., USA: Nova Publisher; 2012. p. 1-20. [ Links ]














