Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos de cardiología de México
versión On-line ISSN 1665-1731versión impresa ISSN 1405-9940
Arch. Cardiol. Méx. vol.83 no.4 Ciudad de México oct./dic. 2013
https://doi.org/10.1016/j.acmx.2013.08.001
Investigación clínica
Continuous glucose monitoring in acute coronary syndrome
Monitoreo continuo de glucosa en pacientes con síndrome coronario agudo
Karina Alejandra Rodríguez-Quintanillab,*, Fernando Javier Lavalle-Gonzáleza,b, Leonardo Guadalupe Mancillas-Adamea,b, Alfonso Javier Zapata-Garridoa,b, Jesús Zacarías Villarreal-Péreza,b, Héctor Eloy Tamez-Péreza,b
a Servicio de Endocrinología, Departamento de Medicina Interna, Hospital Universitario Dr. José Eleuterio González, Facultad de Medicina, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México.
b Departamento de Medicina Interna, Hospital Universitario Dr. José Eleuterio González, Facultad de Medicina, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México.
* Corresponding author:
Calle Francisco I. Madero s/n Colonia Mitras Centro Monterrey,
Nuevo León 64460, México.
Tel.: +52 83487871; fax: +52 83487871.
E-mail address: karinamed07@hotmail.com (K.A. Rodríguez-Quintanilla).
Received 15 March 2012.
Accepted 19 August 2013.
Abstract
Background: Diabetes mellitus is an independent risk factor for cardiovascular disease.
Objective: To compare the efficacy of devices for continuous glucose monitoring and capillary glucose monitoring in hospitalized patients with acute coronary syndrome using the following parameters: time to achieve normoglycemia, period of time in normoglycemia, and episodes of hypoglycemia.
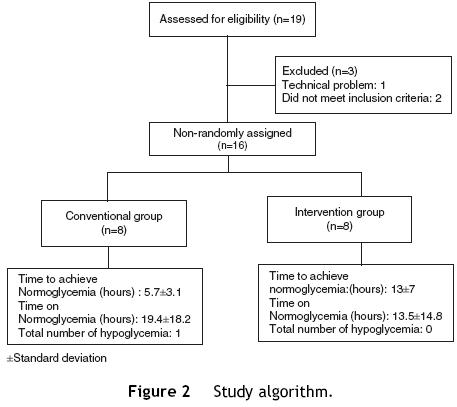
Methods: We performed a pilot, non-randomized, unblinded clinical trial that included 16 patients with acute coronary artery syndrome, a capillary or venous blood glucose ≥ 140 mg/dl, and treatment with a continuous infusion of fast acting human insulin. These patients were randomized into 2 groups: a conventional group, in which capillary measurement and recording as well as insulin adjustment were made every 4h, and an intervention group, in which measurement and recording as well as insulin adjustment were made every hour with a subcutaneous continuous monitoring system. Student's t-test was applied for mean differences and the X2 test for qualitative variables.
Results: We observed a statistically significant difference in the mean time for achieving normoglycemia, favoring the conventional group with a P = 0.02.
Conclusion: Continuous monitoring systems are as useful as capillary monitoring for achieving normoglycemia.
Keywords: Glucose; Blood monitoring glucose; Capillary glucose; Continuous glucose monitoring; Acute coronary syndrome; Mexico.
Resumen
Antecedentes: La diabetes mellitus es un factor de riesgo independiente de enfermedad cardiovascular.
Objetivo: Comparar la eficacia de los dispositivos de monitorización continua de glucosa y monitorización de glucosa capilar en pacientes hospitalizados con síndrome coronario agudo, mediante los siguientes parámetros: tiempo en lograr normoglucemia, periodo en normoglucemia y número de hipoglucemias.
Métodos: Ensayo clínico no aleatorizado, no ciego, que incluyó a 16 pacientes con síndrome coronario agudo, glucosa capilar o venosa ≥ 140mg/dl, en tratamiento con infusión de insulina humana de acción rápida durante 48 h. Se distribuyeron en 2 grupos: convencional, con medición y registro de glucosa capilar, y ajuste de insulina cada 4h, y de intervención, con medición y registro de glucosa intersticial y ajuste de insulina cada hora a través de un dispositivo de monitorización continua colocado vía subcutánea. Se aplicaron pruebas t para diferencia de medias y prueba de X2 para las variables cualitativas.
Resultados: Se observó diferencia significativa en la media del tiempo para lograr normoglucemia a favor del grupo convencional, con un valor de p = 0.02.
Conclusión: Los dispositivos de monitorización continua de glucosa son tan útiles como la monitorización de glucosa capilar para lograr normoglucemia.
Palabras clave: Glucosa; Glucosa sanguínea; Glucosa capilar; Monitoreo continuo de glucosa; Síndrome coronario agudo; México.
Introduction
The worldwide prevalence of type 2 diabetes mellitus is 6% (246 million individuals).1 According to the National Health Survey (ENSANUT 2006), the prevalence in Mexico is 14.4%, with this disease being the leading cause of death (11.2%).2 Diabetes mellitus (DM) is an independent risk factor for cardiovascular disease, due to the chronic inflammatory state induced by high glucose levels and their variability. The presence of DM or hyperglycemia in patients with ischemic heart disease increases mortality by 50% per year, and causes a higher rate of re-infarction and poor response to therapeutic measures.3 More than 50% of patients with their first acute coronary syndrome have glucose intolerance or undiagnosed DM, which are factors of poor outcome in the short and long term.4
The standardized methods of glucose control that are used are capillary glucose monitoring and venous glucose monitoring5; which provide, respectively, an accurate information to be obtained directly from the sample capillary and venous blood, also, frequent self-monitoring blood glucose (SMBG) has been correlated with an improvement of metabolic control, but the optimal number of measurements of SMBG is not defined6; by the above, a real-time method that permits assessment of glucose variability in the acute coronary setting is needed to achieve proper glucose control.
Continuous glucose monitoring provides information about direction, duration, frequency and causes of variability glucose changes; in contrast to blood glucose self-monitoring that corresponds to three measurements of capillary glucose each day, continuous glucose monitoring gives greater knowledge about ''all day'' glucose levels. Continuous readings provide information about glucose tendency and could help to identify and prevent hypoglycemic events.7,8 One of the advantages of continuous glucose monitoring is its ability to predict future glucose levels, this cannot be done with blood glucose self-monitoring9; however, there are several difficulties with continuous glucose monitoring, as an increase in the number of insulin adjustments per day, requirement of a trained operator and calibration every 12 h, which could make it less practical for in-hospital use. Several continuous glucose monitoring devices have been approved by FDA (Food and Drug Administration) for use in the United States and Europe, minimally invasive through continuous interstitial measurement involving cutaneous barrier and without puncturing a blood vessel, or with a non-invasive method through electromagnetic radiation from the skin to blood vessels. After 2 h of time synchronization and specific calibration process, each sensor can provide a glucose reading every 1 -10 min for a 72 h period. Some models have an alarm that activates if glucose levels get out of normal levels.10-13 Considering the existence of different methods of glucose monitoring and the lack of consensus about their usefulness in glycemic control of inpatients, our goal is to determine if continuous glucose monitoring devices are more effective than capillary glucose monitoring for achieving normoglycemia in patients with acute coronary syndrome in addition to preventing episodes of hypoglycemia due to the default alarms of hyper and hypoglycemia.
Methods
This is a pilot, non-randomized, unblinded clinical trial evaluating if continuous glucose monitoring devices are more effective than capillary glucose monitoring for achieving normoglycemia in patients with acute coronary syndrome. Patients' 20-70 years of age were enrolled if they were admitted to the emergency department of the Dr. José Eleuterio González University Hospital from January 1, 2010 to July 31, 2011 with a diagnosis of acute coronary syndrome with or without ST elevation, a blood or capillary glucose level greater than 140mg/dl, and with or without a prior history of acute coronary syndrome. Exclusion criteria included patients in cardiogenic shock with or without the use of vasopressors, acute renal failure and/or a calculated creatinine clearance less than 60ml/min according to the Crockoft-Gault formula,14 an admission diagnosis of diabetic ketoacido-sis or a hyperglycemic hyperosmolar state, and patients with alcohol withdrawal syndrome, chronic liver disease, cellulitis and/or herpes at the device site placement or those unable to provide informed consent. Acute coronary syndrome,15 hypoglycemia, and diabetes mellitus were defined according to current clinical guidelines.16
The study complies with the Declaration of Helsinki and was approved by the Ethics Committee of the Universidad Autónoma de Nuevo León Medical School and Dr. José Eleuterio González University Hospital with registration number 09-025. All patients provided written informed consent.
Patients were started on a continuous intravenous infusion of fast acting insulin titrated according to the Yale protocol.17 On admission patients were randomized into two groups, the conventional group, in whom measurement and recording of capillary glucose was performed every 4 h, and the intervention group, in whom a Medtronic Guardian® RT device was inserted subcutaneously in the lower abdomen 2 inches from the umbilicus.18 Five minutes after electrode (sensor) insertion, the MiniLink REAL-time transmitter was connected to the sensor, allowing the electrode to have contact with interstitial fluid. The monitor was placed at the bedside of the patient and data were received every 5 min through the transmitter. Two hours after the initialization time, a nurse was instructed to perform capillary glucose and insert the value into the continuous monitoring Medtronic Guardian® RT (Fig. 1) for the first calibration.19

All patients were monitored for 48 h. Decisions on dose adjustment of the insulin infusion were made based on the Yale protocol; every 4 h for the conventional group, and every hour for the intervention group with a glucose goal equal or less than 140mg/dl. If a hypoglycemia or hyperglycemia alarm occurred in the intervention group, the glucose value was confirmed with a capillary glucose reading and action was taken as suggested by the Yale insulin infusion protocol. Each glucose value and insulin dose was recorded on control sheets. Capillary glucose measurement was made with an Accu-Check Inform® Roche glucometer. Venous glucose readings and measurements were made every 8 h for both groups and capillary glucose measurement every 12 h in the intervention group for Guardian RealTime® device calibration. During monitoring, we conducted a lifestyle and prior history survey and all patients received a 25kcal/kg/day diet. A lipid profile, glycosylated hemoglobin, anthropometry, blood pressure measurements, creatinine level, and glomerular filtration rate to estimate kidney function, were performed. After discharge, each patient was followed by telephone after 30 days to assess the occurrence of complications, re-admission for acute coronary syndrome, cerebral vascular disease, arrhythmias and/or death.
The primary endpoints of the study were the time (hours) for achieving normoglycemia by group, the period of time that they remained in normoglycemia, and the presence of episodes of hypoglycemia. For study purposes normoglycemia was defined as a value less than 140mg/dl; hypoglycemia was defined by the presence of symptoms associated with hipoglycemia and capillary glucose value equal to or less than 70mg/dl according to current clinical guidelines.16
Secondary endpoints included were the day 1 to day 2 glucose difference, and the number of insulin dose adjustments per day between both groups and their difference.
Statistical analysis was performed using SPSS version 18.0. We compared the value distribution in both groups using the Kolmogorov test. Mean differences were determined in both groups with Student's t-test for independent samples; for qualitative variables, contingency tables were applied to X2 test. For analysis of variables within the same group an analysis of variance was used. All probability values reported are two-sided, and a value of P < 0.05 was considered significant.
Results
Nineteen patients participated in the study, three were eliminated, one due to electrode failure, and two more for not completing the requirements. The study algorithm is shown in Fig. 2. A population of 16 patients was randomized into two groups of eight patients each. The data distribution was normal according with Kolmogorov test. The demographic characteristics of the population, with means and standard deviations are shown in Table 1. In the control group, there were six men (75%) and two women (25%), whereas in the intervention group there were seven men (87.5%) and one woman (22.5%). Mean age was 55.2 years for the conventional group, and 54 years for the intervention group. We observed a statistically significant difference for dyslipidemia in both groups, with a P value of 0.002.
The anthropometric and clinical variables are shown in Table 2. We observed a statistically significant difference between groups in total cholesterol values, with a P value of 0.02, with a similar behavior for low-density cholesterol values, with a P = 0.01.
The values of glucose monitoring after performing data analysis are shown in Table 3, results were statistically significant in the mean time for achieving normoglycemia between groups, with a P value of 0.02. For variables that were analyzed in the same group (day 1 to day 2 glucose difference, insulin dose difference from day 1 to day 2, and total number of insulin doses adjustments from day 1 to day 2), we obtained significant differences in relation to day 1 to day 2 glucose in the intervention group with a P value of 0.07. With regard to the total number of insulin dose adjustments from day 1 to day 2, we observed a significant difference in the conventional group with a P value of 0.03. Only one event of hypoglycemia occurred in the conventional group.
Discharge diagnoses, treatment employed, risk stratification obtained according to the UKPDS risk Engine calculator v2.020 as well as complications and mortality showed no statistically significant differences between groups, and are shown in Table 4.
Discussion
Our study shows that continuous glucose monitoring devices were not superior to capillary glucose monitoring for improving the time to achieve normoglycemia and the time that the patient remains there. Despite this, patients with continuous glucose monitoring devices were more stable, as demonstrated by the mean glucose levels on day 1 and day 2. In addition, all patients in the interven-tional group reached levels of normoglycemia in comparison with the conventional group indicating that continuous glucose monitoring allows identification of more regular glucose values with minimum variability. Continuous glucose monitoring in hospitalized patients could be a tool to prevent hypoglycemic episodes, a fact that was demonstrated in this study, as there were none in the intervention group.
All studies that compare tight glucose control have been directed at evaluating capillary glucose monitoring in the intensive care unit at different time intervals with different target glucose levels and different effects on mortality.21 The NICE-SUGAR study demonstrated a higher mortality in critically ill patients with intensive glucose control, mainly attributed to a higher number of severe hypoglycemic episodes22; however, a post hoc analysis of the DIGAMI-2 trial did not show an association between hypoglycemic episodes and adverse outcomes.23
These findings make it necessary to expand efforts toward improved glycemic control in patients with acute coronary syndrome, since continuous glucose monitoring provides a real time information about glucose variability in comparison with capillary or venous glucose.
The main strength of our study is that it is a comparative study of continuous glucose monitoring devices and conventional capillary glucose monitoring in patients with acute coronary syndrome. Existing studies have been conducted to study the accuracy of continuous monitoring devices in comparison with capillary measurements.24 This study also considered the in-hospital use of this device and the technical difficulties that may arise with it. This study shows that there is a better glycemic control with continuous glucose monitoring, suggesting less glucose variability, gaining importance for clinical evolution and prognosis; however, more studies are needed with more patients to evaluate the effects of control on glucose variability and on prognosis and outcome of patients with acute coronary syndrome.
On the other hand, our study has several limitations. It is a study with few patients, also it is an open and non-randomized study making it difficult to control all variables, obtaining wide difference in terms of some variables assessed, such as the time evolution of the DM, the presence of dyslipidemia or family history of acute coronary syndrome, glycated hemoglobin values, where there were differences that indicate a heterogeneity between groups, which is a common problem in non-randomized studies; the technical difficulties associated with using this technology should also be taken into account, which have been described in some studies; Jacobs and colleagues performed a study on the tolerability and precision of a device for continuous glucose monitoring in a rural intensive care unit, finding that despite being well tolerated by the patient, it was not very accurate for glycemic control in the context of diabetic ketoacidosis due to technical difficulties associated with calibration of the device and electrode performance.10
Randomized clinical trials that include a greater number of patient are needed, aimed at comparing continuous glucose monitoring with conventional methods (capillary and venous glucose monitoring) and their effect on glycemic control, glucose variability, evolution and prognosis of critically ill patients, including those with acute coronary syndrome, to establish the best conditions for its in-hospital use.
Conclusion
Further studies are necessary to determine the effectiveness of continuous glucose monitoring devices in hospitalized patients and to establish the most useful clinical scenarios for their use, since it is an effective way to obtain more realistic glucose control and prevent hypoglycemic episodes.
Funding
Did not receive any sponsorship to conduct this study.
Conflict of interest
The author states have no conflicts of interest.
Acknowledgement
The authors are grateful to Dr. Sergio Lozano-Rodriguez for his critical review of the manuscript.
References
1. World Health Organization. Prevention of diabetes mellitus. Technical report series no. 844. Geneva: World Health Organization; 1994. [ Links ]
2. Olaiz Fernández G, Rivera Dommarco J, Shamah Levy T, et al. Encuesta Nacional de Salud y Nutrición 2006. Cuernavaca, México: Instituto Nacional de Salud Pública; 2006. [ Links ]
3. Czyzk A, Królewski AS, Szablowska S, et al. Clinical course of myocardial infarction among diabetic patients. Diabetes Care. 1980;3:526-9. [ Links ]
4. Conaway DG, O'Keefe JH, Reid KJ, et al. Frequency of undi-agnosed diabetes mellitus in patients with acute coronary syndrome. Am J Cardiol. 2005;96:363 -5. [ Links ]
5. Clement S, Braithwaite SS, Magee MF, et al. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27:553-91. [ Links ]
6. González Blanco C, Pérez Pérez A. Benefits of capillary glucose monitoring in patients with type 1 and type 2 diabetes treated with insulin. Av Diabetol. 2010;26:5 -8. [ Links ]
7. Ellis SL, Bookout T, Garg SK, et al. Use of continuous glucose monitoring to improve diabetes mellitus management. Endocrinol Metab Clin North Am. 2007;36:46-68. [ Links ]
8. Keenan DB, Mastrotaro JJ, Voskanyan G, et al. Delays in minimally invasive continous glucose monitoring devices: a review of current technology. J Diabetes Sci Technol. 2009;3:1207-14. [ Links ]
9. Joseph IJ, Hipszer B, Mraovic B, et al. Clinical need for continuous glucose monitoring in the hospital. J Diabetes Sci Technol. 2009;3:1309-18. [ Links ]
10. Jacobs B, Phan K, Bertheau L, et al. Continuous glucose monitoring system in a rural intensive care unit: a pilot study evaluating accuracy and acceptance. J Diabetes Sci Technol. 2010;4:636-44. [ Links ]
11. Baquette BW. Continuous glucose monitoring: real-time algorithms for calibration, filtering, and alarms. J Diabetes Sci Technol. 2010;4:404-18. [ Links ]
12. Nybäck-Nackell A, von Heijne M, Adamson U, et al. Accuracy of continuous nocturnal glucose monitoring after 48 and 72 hours in type 2 diabetes patients on combined oral and insulin therapy. Diabetes Metab. 2004;30:517-21. [ Links ]
13. Blevins TC. Professional continuous glucose monitoring in clinical practice 2010. J Diabetes Sci Technol. 2010;4:440-56. [ Links ]
14. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31-41. [ Links ]
15. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction Executive Summary. J Am Coll Cardiol. 2007;50:652-726. [ Links ]
16. American Diabetes Association. Standard of medical care in diabetes - 2011. Diabetes Care. 2011;34:S11 -61. [ Links ]
17. Goldberg AP, Siegel DM, Sherwin S, et al. Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Diabetes Care. 2004;27:461 -7. [ Links ]
18. Klonoff CD. Continuous glucose monitoring. Diabetes Care. 2005;28:1231-9. [ Links ]
19. Wayne BB. Continuous glucose monitoring: real-time algorithms for calibration, filtering, and alarms. J Diabetes Sci Technol. 2010;4:404-18. [ Links ]
20. Stevens RJ, Kothari V, Adler AI, et al. The UKPDS Risk Engine: a model for the Risk Coronary Heart disease in Type II diabetes (UKPDS 56). Clin Sci (Lond). 2001;101:671-9. [ Links ]
21. Kovalaske MA, Gandhi YG. Glycemic control in the medical intensive care unit. J Diabetes Sci Technol. 2009;3:1330-41. [ Links ]
22. The NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283-97. [ Links ]
23. Mellbin LG, Malmberg K, Waldenstrom A, et al. Prognostic implications of hypoglycemic episodes during hospitalization for myocardial infarction in patients with type 2 diabetes: a report from the DIGAMI 2 trial. Heart. 2009;95: 721-7. [ Links ]
24. Radermecker RP, Sultan A, Piot C, et al. Continuous glucose monitoring as a tool to identify hyperglycaemia in non-diabetic patients with acute coronary syndromes. Diabet Med. 2009;26:167-70. [ Links ]














