Servicios Personalizados
Revista
Articulo
Indicadores
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos de cardiología de México
versión On-line ISSN 1665-1731versión impresa ISSN 1405-9940
Arch. Cardiol. Méx. vol.79 no.3 Ciudad de México jul./sep. 2009
Investigación básica: electrofisiología y arritmias
Antiarrhythmic and cardioprotective effects of remifentanil in anesthetized dogs
Efectos antiarrítmicos y cardioprotectores de remifentanil en perros anestesiados
Pastor Luna–Ortiz,1 Gabriela Zarco–Olvera,1 Margarita Ramírez–Ortega,1 Fermín A Tenorio–López,2 Alfonso Gutiérrez,3 Martín Martínez–Rosas,2 Leonardo Del–Valle–Mondragón,1 and Gustavo Pastelín1
1 Departamento de Farmacología.
2 Departamento de Fisiología, Instituto Nacional de Cardiología Ignacio Chávez.
3 Centro de Investigación en Computación IPN.
Corresponding author:
Gustavo Pastelín,
Departamento de Farmacología,
Instituto Nacional de Cardiología Ignacio Chávez,
Juan Badiano No. 1, Col. Sección XVI,
México, D.F. CP 14080
Received: December 10, 2008.
Accepted: July 27, 2009.
Abstract
Objective: To study the antiarrhythmic effect of remifentanil in experimental arrhythmias in dogs.
Methods: We used dogs weighing 12 kg–18 kg anesthetized with 30 mg/kg sodium pen–tobarbital given intravenously. Ventricular arrhythmia, ventricular fibrillation and death were induced with digoxin (9 ug/kg/min). In another model, two types of arrhythmia were induced in the right atrium, one of them with aconitine crystals placed on the right atrium and the other was induced in the basement of the right atrium by electrical stimulation. The potential antiarrhythmic action of remifentanil was investigated in ventricular and atrial arrhythmias by the administration of an intravenous bolus after toxic signs were evident. Thus, two arrhythmias with different mechanisms were generated. Leads DM, unipolar left intraventricular and right atrial leads, and left ventricular pressure were used to record control tracings and tracings in presence of remifentanil, during ventricular arrhythmia.
Results: Remifentanil abolished toxic effects of digoxin, it eliminated the A–V dissociation and ventricular extrasystoles, reverting to sinus rhythm in each case. Remifentanil extended the time to reach lethal doses from 63.25 ± 11.3 to 100 ± 11.8 min. These effects were blocked by naloxone (0.01 ug/kg) applied before remifentanil. In the two arrhythmias model, remifentanil suppressed both, ectopic focus and atrial flutter.
Conclusions: Remifentanil elicits antiarrhythmic and cardioprotective effects in experimental ventricular arrhythmias induced by digoxin and in a model of two atrial arrhythmias induced by aconitine and by electrical stimulation.
Key words: Remifentanil; Antiarrhythmic action; Cardioprotection; Opioids.
Resumen
Objetivo: Estudiar el efecto antiarrítmico del remifentanil en las arritmias experimentales en perros.
Métodos: Se utilizaron perros con peso entre 12 kg y 18 kg, anestesiados con pen–tobarbital sódico 30 mg/kg por vía intravenosa. Se les administró digoxina (9 mg/kg/min) hasta inducir intoxicación, manifestada por arritmias ventriculares, disociación A–V, fibrilación ventricular y muerte. Por otra parte, se generó un foco ectopico en la aurícula derecha inducido por cristales de aconitina y en la orejuela derecha se generó un movimiento circular con estimulación, estableciendo el modelo de la doble arritmia El remifentanil (0.05 ug/kg) se aplicó en bolo intravenoso. Se registraron las derivaciones Dll, las unipolares del ventrículo izquierdo, aurícula derecha, orejuela derecha y se registró la presión intraventricular izquierda.
Resultados: El remifentanil fue capaz de revertir los efectos tóxicos de la digoxina, eliminando la disociación A–V, las extrasístoles ventriculares multifocales, con reversión a ritmo sinusal en todos los casos. El remifentanil prolongó el tiempo de la dosis letal de 63.25 ± 11.3 min a 100 ±11.8 min. Estos efectos del remifentanil fueron bloqueados al administrar, previamente, naloxona. En el modelo de la doble arritmia auricular, el remifentanil eliminó el foco ectopico y el flutter auricular.
Conclusiones: El remifentanil tiene un efecto antiarrítmico y cardioprotector en las arritmias experimentales en el perro.
Palabras clave: Remifentanil; Acción antiarrítmica; Cardioprotección; Opiáceos.
Introduction
Recent evidence suggests that agonists of opioid receptors induce cardioprotection.1,2 Cardioprotection can be produced pharmacologically through different pathways. To this regard, Schultz et al. (1995) demonstrated that opioids produce cardioprotection through a G–protein–linked mechanism in a myocardial infarct rat model.3 Miki et al. demonstrated that the cardioprotection induced by morphine in the myocardium of rabbits is mediated by the protein kinase C (PKC).4 Opioids can induce a mechanism mediated by multiple kinases similar to those involved in the preconditioning of ischemia. Among the reported kinases are the PKC, the tyrosine kinase, and a family of mitogen–activated protein kinases (MAP kinases).5 Regarding the final effect of cardioprotection, involvement of ATP–modulated potassium channels in the cellular membrane (KATP) and in the mitochondria (mito KATP) is known. It has been demonstrated that TAN–67 an agonist of the delta–1 receptor produces a potent antiarrhythmic and antifibrillatory effect on ischemia that can be abolished by KATP antagonists in the mitochondria.6 KATP inhibitors, such as glibenclamide, can abolish this cardioprotection.7 Agonists of opioid receptors can also have antiarrhythmic properties as part of their cardioprotective effect. Márquez Montes et al. demonstrated a beneficial effect of morphine on the electrical fibrillation threshold of the ventricle in anesthetized dogs;8 these authors used morphine (3 mg/kg IV) and elevated the fibrillation threshold from 10 mA to 20 mA. Fentanyl, an agonist of the mureceptor, increases the ventricular fibrillation threshold in 14% in anesthetized dogs.9,10 Yu et al, in 1999, suggested that the stimulation of kappa–opioid receptors produces cardioprotection against arrhythmias and intracellular calcium oscillations induced by beta–adrenergic stimulation.11 Nekrassov and Peón, from the Instituto Nacional de Cardiología "Ignacio Chávez", studied the effect of conorphone (3 mg/kg IV) on an experimental myocardial infarction in rats by administering the drug 10 min before ligating the anterior descending coronary and found a statistically significant decrease in the infarct size. Besides, by electron microscopy, these authors observed intracellular edema and destruction of crests and membranes of the mitochondria, in the control group. However in the conorphone–treated group they observed mitochondrial vacuoles without other manifestations of cellular damage.12 Recently, Cho et al. demonstrated that opioid peptides that act on the mitochondria, diminish the myocardial infarction in rats induced by ischemia–reperfusion, and arrhythmias were less frequent and severe than in the control group.13
Remifentanil is an opioid of the 4–anilido–piperidine family with an agonist effect on mu, delta, and kappa receptors.14 Remifentanil presents a short elimination half–life of approximately 3min to 10 min; its chemical structure has an ester linkage that undergoes rapid hydrolysis by non–specific tissue and plasma esterases.14 It is widely used in surgery for its pharmacokinetic properties and because the recovery from remifentanil anesthesia is much faster than with any other opioid studied until now.15
The objective of this study was to determine if remifentanil exerts antiarrhythmic action in experimental arrhythmias in the dog (atrial flutter, atrial ectopic focus induced by aconitine and in arrhythmias induced by digitalis intoxication) and to assess its cardioprotective effect by measuring the time course of a lethal dose (LD) of digoxin.
Material and methods
We studied 25 mongrel dogs of either sex, weight between 12 kg and 18 kg, anesthetized with sodium pento–barbital at a dose of 30 mg/kg applied IV. Tracheotomy was performed for pulmonary ventilation with 30 ml/kg of ambient air (Palmer CF ventilator, Mod. London 8W2). Arterial blood samples were taken to measure pH, PCO2, and PO2 before, during, and at the end of the experiment to corroborate that pulmonary ventilation was adequate. The chest was opened through median sternotomy and the pericardium was dissected to expose the heart and place four pairs of recording and stimulating electrodes: two pairs in the right atrium and two pairs in the right atrial appendage (RAA). Four more electrodes were placed in the limbs for the electrocardiographic recording of lead Dll. To record arterial pressure the right carotid artery was dissected and cannulated and connected to a U–shaped Hg manometer. A Swan–Ganz catheter was passed through the femoral artery to the left ventricle to record the intraventricular pressure (IVP). The femoral vein was cannulated for the administration of fluids (Hartman solution, 100 ml/h), anesthesia, and the drugs to be studied. AVR6 Electronics for Medicine polygraph with interphase for data acquisition in a personal computer was used.
Animals were divided in five groups. Group I (n = 5) received remifentanil at 0.1 and 1 μg/kg, to determine the dose–effect relationship on arterial pressure IVP, and heart rate (HR), as well as to find the dose with the minimal hemodynamic effect to be used in the other groups.
Group II (n = 5) received digoxin by means of an infusion pump at a speed of 9 μ/kg/min to determine the temporal course of digitalis intoxication and measure the time (min) to reach the LD.16
Group III (n = 5) received digoxin infusion (9 mg/kg/ min) until reaching the first signs of digitalis intoxication (sustained A–V block, ventricular extrasystoles), after that remifentanil was administered as a single bolus. In two additional experiments, two remifentanil boluses were administered. The first bolus was given at the beginning of the digitalis intoxication, and the second one, 5 min thereafter.
Group IV (n = 5) received digoxin (9 mg/kg/min) to induce digitalis intoxication, once the early electrocardio–graphic intoxication signs have appeared, naloxone was administered at a single dose of 0.01 mg/kg. Afterwards, remifentanil was administered in a single bolus.
In group V (n = 5), we studied the effect of remifentanil in the double arrhythmia model. This method consists in inducing simultaneously two arrhythmias in the right atrium of the anesthetized dog with the open chest. By clamping the base of the atrial appendage, the rest of the atrium becomes electrically isolated. A very small aconitine crystal was placed near to the tip of the atrial appendage, which induces an ectopic focus with a frequency usually higher than 5 beats per second. In the remnant atrium, a flutter was produced by the circular movement of a stimulus following the method of Rosenblueth and Garcia Ramos.17 This method is based on high–frequency electrical stimulation (20 Hz).18 These approaches yielded an experimental model of two arrhythmias of different mechanisms that were recorded in the same atrium. Figure 1: Once both arrhythmias have been produced, they were observed for 20 min to confirm their stability and to administer remifentanil in a single bolus. Results are presented as mean ± standard deviation (SD).

Results
The remifentanil dose with minimal hemodynamic effect in the barbiturate–anesthetized dog was of 0.5 mg/kg (group I; n = 5). During the temporal course recording of the digitalis intoxication (group II) it was found that digoxin (9 mg/kg/min) reached the LD (0.527 ± 0.079 mg/ kg; n = 5) in an average time of 63.25 ±11.3 min. This is consistent with the report published in 1964 in which, during the temporal course of digitalis intoxication, an A–V block is produced early and then continues until reaching ventricular fibrillation and asystolia.19 In group II, remifentanil given as a single bolus abolished the effects produced by digoxin in all cases, reverting the A–V dissociation and eliminating the multifocal ventricular extrasystoles, returning to a sinus rhythm and delaying the LD time to 100 ± 11.8 min.
The Figure 2 illustrates these results. Panel A shows the control recordings. Panel B corresponds to the beginning of digoxin administration (74 min). Panel C, at 121 min of digitalis infusion, an atrial asystolia in right atrium (RA) can be observed, as well as absence of P wave in Dll, and a drop of IVP, just before that remifentanil bolus was applied. Panel D ,1 min afterwards, depicts the remifentanil effect, observing again the trace in RA, the sinus rhythm is recovered in DM, and the HR returns to control values. E and F (18 and 20 min afterwards, respectively) depict the reestablishment of the digitalis intoxication course that continues until producing ventricular fibrillation and atrial and ventricular asystoli'a. When using two remifentanil boluses (n = 2), the LD time increased to 145 min in one dog; in the other dog, neither ventricular fibrillation nor death occurred even after 3 hours of recording and maintaining the digoxin infusion (electrocardiographic data not shown).

In group IV, once digoxin and naloxone were administered, remifentanil was not able to revert the digitalis intoxication. Figure 3 illustrates these effects. Panel A depicts the control electrocardiographic recording. Panel B depicts the first signs of the digoxin–induced intoxication (70 min.), C shows the atrial flutter, the irregular rhythm in left ventricular (LV), and ventricular fibrillation in DM; at this moment, naloxone was administered (80 min), 3 min later, remifentanil was administered in a single bolus, but it did not produce any appreciable effect on the digoxin–induced changes, as observed in E and F.
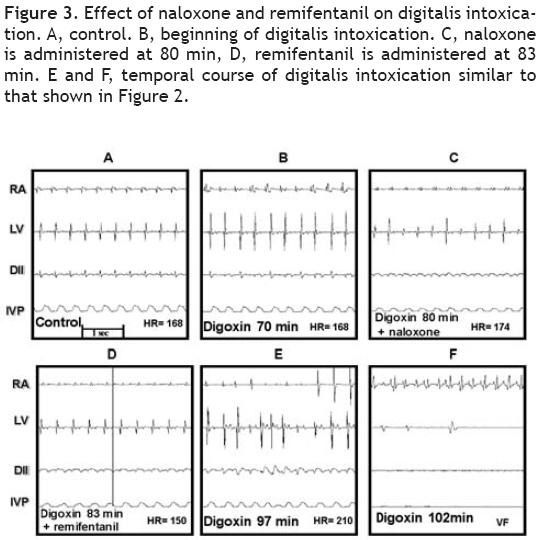
The average time LD (min) obtained in the previous groups is show in Figure 4. In the digitalis–induced intoxication group (D) the LD was of 63.25 ±11.3 min (n = 5); in the digoxin plus remifentanil group (D + R), LD was of 100 ±11.8 min (n = 5). The third bar corresponds to the value obtained in a single animal (145 min) that received two boluses of remifentanil (D+R(2)). It is important to take in account that the other dog that also received the two remifentanil boluses, it was not considered in this graph. The last bar corresponds to the digoxin, naloxone, and remifentanil (D+N+R) group in which the LD was similar to that of the control group, 65.2±13.8 (n = 5).

The Figure 5 illustrates one of the results obtained with group V, using the double arrhythmia model to study the effect of a single remifentanil bolus (0.5 mg/kg).
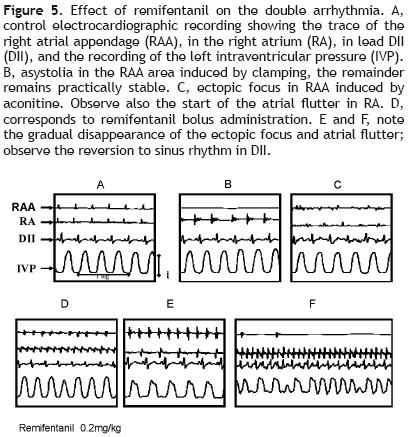
Panel A shows the control recording. Panel B depicts the asystoli'a in the RAA area induced by its clamping, the other recordings remain practically stable. In C, the ectopic focus produced by aconitine in RAA can be seen as well as the start of the atrial flutter in RA. Once the double arrhythmia has been established, the remifentanil bolus is applied (panel D). Panel E shows the gradual disappearance of the ectopic focus and atrial flutter, as well as reversal to sinus rhythm in DM. In F it was not possible to maintain the antiarrhythmic effect in the aconitine–induced arrhythmia; however, it can be observed that the rest of the tracings remain close to the control tracing, although at a higher frequency. Remifentanil, in this experimental model, eliminated three of the five atrial tachycardias induced by aconitine and two of the five atrial flutters.
Discussion
Opioids have been demonstrated to possess antiarrhythmic activity especially in those arrhythmias associated to an ischemia–reperfusion injury.1–6 Our results demonstrate the antiarrhythmic effect of remifentanil in arrhythmias induced by digitalis intoxication and in the double arrhythmia model in anesthetized dogs. The remifentanil dose used (with the minimal hemodynamic effect) was 0.5 μg/kg (group I). This value correlates with that reported by other authors, who measured the anesthetic potency of remifentanil in dogs anesthetized with enflurane, finding that a 0.72 mg/kg/min dose produces a 50% decrease in the minimal alveolar concentration (MAC).20 This remifentanil dose abolished the A–V dissociation and the ventricular extrasystoles, reverting to a sinus rhythm in all animals of the digitalis intoxication group (group III). This effect seems to be mediated by opioid receptors since naloxone was able to inhibit the antiarrhythmic effect of remifentanil, as observed in the presence of this antagonist. To determine the type receptors involved in these effects more specific studies are needed.
In the double arrhythmia model, remifentanil presented an interesting effect on the ectopic focus although transient. Besides, it only eliminated three of the produced ectopic foci. Remifentanil exerted a lower effect on the circular movement although more prolonged in time, since it was maintained until the last stage of recording. This could be due to an increase in the refractory period induced by remifentanil, being enough to prolong the wavelength. Likewise, remifentanil presented a partial antiarrhythmic effect, as it eliminated only two of the five induced atrial flutters. In summary, in our experimental conditions, we observed a 59% and 129% (the latter in only one case; (Figure 4) increase in the LD of digoxin induced by remifentanil, plus one case in which it was not possible to maintain the digitalis intoxication toward fibrillation and death using a double remifentanil dose. These data suggest that remifentanil is capable of activating dose–dependent myocardial protective effects; this suggestion requires additional research for its confirmation. The antiarrhythmic effects of remifentanil could be related to changes in the ionic channels activity of the myocardium. In this sense, a morphine–induced increase in duration of the cardiac action potential and hyperpo–larization of the membrane resting potential, due to an increase in the potassium current IK1, in rabbit ventricular myocytes have been reported.21 Currently, there is no consensus regarding the mechanism of opioids involved in the induction of cardioprotection and increase in the resistance to arrhythmogenic factors; however it seems that rather diverse mechanisms are involved. Some authors suggest that the autonomous nervous system –in its sympathetic branch– plays an important role in this mechanism.22 Other authors attribute the beneficial effects of opioids to activation of opioid receptors of the myocardium that inhibit adenylcyclase activity with the consequent decrease in cAMP production.11 This would lead to a negative effect in cardiac inotropism and chronotropism.
On the other hand, it has been proposed that activation of opioid receptors stimulates the production of nitric oxide, which could contribute to the electrical stability of the heart acting on the endothelium of the coronary vessels and increasing blood flow to the myocardium.23 It has also been reported that opioid peptides increase the resistance not only to ischemia–reperfusion–induced arrhythmias but also to catecholamine– and aconitine–induced arrhythmias.24 There are other arrhythmogenic mechanisms on which the antiarrhythmic activity of opioids has not been tested, such as arrhythmias due to atrial flutter re–entry and the different types of arrhythmia produced by digitalis intoxication. In the present study, we found that remifentanil has an antiarrhythmic effect on arrhythmias induced in the atrium (double arrhythmia model) as well as on the ventricular arrhyhtmia produced by digitalis intoxication.
Most opioid agonists show affinity to a certain type of opioid receptor. Remifentanil is mainly a mu–agonist but it also exerts an effect on delta and kappa receptors.14 Opioid receptors are present in practically all organs and tissues but differ in the distribution of the subtypes. In the human heart, there are three subtypes distributed in the atrium and in the ventricle at different proportions.25 Therefore, activation of opioid receptors can induce heart resistance to the cardiotoxic and arrhythmogenic effect of diverse pharmacological agents. According to our results, probably the highest resistance to digitalis intoxication, the partial reversal to digoxin intoxication, and the antiarrhythmic activity induced by remifentanil resulted from the action of the opioidergic system, mainly on the opening of the sarcolemal and mitochondrial KATP channels, aside from the simultaneous inhibition of the glycogen–synthase–kinase 3–beta, as proposed by other authors.26 Lishmanov et al. suggest that activation of opioidergic receptors exerts antiarrhythmic action against aconitine–induced arrhythmias by inhibiting the sodium–calcium (Na/ Ca) exchange,5 we could add to this mechanism the action of opioids exerted on the KATP channels. This effect could explain one of the electrophysiological conditions to suppress re–entry phenomena, as is the prolongation of wavelength postulated by Rosenblueth.17 The cardio–protective and antiarrhythmic effect of opioids could be mediated by diverse intracellular signaling pathways and by indirect effects as summarized in Figure 6.
Aside from these mechanisms, other less characterized ones have been proposed to participate in the opioid effects, such as release of adenosine induced by opioids and the production of nitric oxide in the cardiac myocyte.23
Clinical implications
Opioids are widely used as analgesic in intensive care units and during surgery as part of the anesthesia for cardiac and non–cardiac surgeries. Remifentanil is preferred for its rapid onset and the fast recovery from anesthesia.
Recently, it has been reported that remifentanil avoided prolongation of the QTc interval associated to tracheal intubation during anesthesia induction with sevoflurane.27 Figure 7 depicts the case of a patient with digitalis intoxication, in whom remifentanil infusion at 0.15 ug/kg/ min reverted the characteristic bigeminism induced by this intoxication.
These clinical findings, together with our results, justify the use of opioids for cardioprotection during pre–and post–conditioning of ischemia and for the prevention of myocardial damage induced by ischemia–reperfusion in patients subjected to coronary angioplasties and to coronary arteries revascularization surgery.28,29
Bibliography
1. Fryer RM, Hsu AK, Nagase H, Gross GJ. Opioid–induced cardioprotection against myocardial infarction and arrhythmias: mitochondrial versus sarcolemal ATP–sensitive potassium channels. J Pharmacol Exp Ther 2000; 294:451 –57. [ Links ]
2. Song W, Shin J, Lee J, Kim H, Oh D, Edelberg JM, et al. Potent opiate agonist protects against myocardial stunning during myocardial ischemia and reperfusion in rats. Coron Art Dis 2005;16:407–10. [ Links ]
3. Schultz J, Rose E, Ao Z, Gross GJ. Evidence for involvement of opioid receptors in ischemic preconditioning in rat heart. Am J Physiol 1995; 268:H2157–61. [ Links ]
4. Miki T, Cohen MV, Downey JM. Opioid receptor contributes to ischemic preconditioning through protein kinase C activation in rabbits. Mol Cell Biochem 1998;186:3–12. [ Links ]
5. Lishmanov YB, Maslov LN. Opioid receptors and heart resistance to arrhythmogenic factors. Bull Exp Biol Med 2004; 13:107–12. [ Links ]
6. Patel HH, Ludwig LM, Fryer RM, Hsu AK, Warltier DC, Gross GJ. Delta opioid agonists and volatile anesthetics facilitate cardioprotection via potentiation of K(ATP) channel opening. FASEB J 2002;16:1468–70. [ Links ]
7. Gross GJ, Auchampach JA. Blockade of ATP–sensitive potassium channels prevents myocardial preconditioning in dogs. Circ Res 1992;70:223–33. [ Links ]
8. Márquez–Montes J, Goiti JJ, Castillo Olivares JL, de Teresa E, Avello F, de Artaza M. Efecto beneficioso de la morfina sobre el umbral de fibrilación eléctrico del ventrículo. Arch Inst Cardiol Mex1997;47:714–8. [ Links ]
9. Saini V, Carr DB, Hagestad EL, Lown B, Verrier RL. Antifibrillatory action of the narcotic agonist fentanyl. Am Heart J 1988; 115:598–605. [ Links ]
10. Saini V, Carr DB, Verrier RL. Comparative effects of the opioids fentanyl and buprenorphine on ventricular vulnerability during acute coronary artery occlusion. Cardiovasc Res 1989;23:1001–6. [ Links ]
11. Yu XC, Wang HX, Pei JM, Wong TM. Anti–arrhytmic effect of K–opioid receptor stimulation in the perfused rat heart:involvement of a CAMP–dependent pathway. J Mol Cell Cardiol 1999;31:1809–19. [ Links ]
12. Nekrasov V, Peon JM. Efecto de la conorfona sobre las dimensiones del infarto del miocardio y las alteraciones ultraestructurales del tejido adyacente. Arch Inst Cardiol Mex 1988; 58:505–9. [ Links ]
13. Cho J, Wong K, Wu D, Soong Y, Liu S, Szeto H, et al. Potent mitochondria–targeted peptides reduce myocardial infarction in rats. Coron Art Dis 2007; 18:215–20. [ Links ]
14. Patel SS, Spencer CM: Remifentanil. Drugs 1996;52:417–27. [ Links ]
15. James MK. Remifentanil and anesthesia for the future. Exp Opin Invest Drugs 1994;3:331–4. [ Links ]
16. Pastelín G, De Micheli A, Valadez F, Méndez R: Efectos antagónicos y aditivos del propranolol con los digitálicos en los vasos y en el corazón. Arch Inst Cardiol Mex 1967;37:221 –35. [ Links ]
17. Rosenblueth A, García Ramos J. Estudios sobre el flutter y la fibrilación: La influencia de los obstáculos artificiales en el flutter auricular experimental. Arch Inst Cardiol Mex 1947;17:441 –5. [ Links ]
18. Pastelín G, Méndez R, Moe GK. Participation of atrial specialized conduction pathways in atrial flutter. Cir Res 1978;42:386–93. [ Links ]
19. Erlij D, Méndez R. The modification of digitalis intoxication by excluding adrenergic influences on the heart. J Pharmacol Exp Ther 1964;144:97–103. [ Links ]
20. Michelsen LG, Salmenpera M, Hug CC, Szlam F, VanderMeer D: Anesthetic potency of remifentanil in dogs. Anesthesiology 1996;84:865–72. [ Links ]
21. Xiao GS, Zhou JJ, Wang Gy, Cao CM, Li GR, Wong TM. In vitro electrophysiologic effects of morphine in rabbit ventricular myocites. Anesthesiology 2005;103:280–6. [ Links ]
22. Mikhailova SD, StorozhakovGI, Popov MA, Semushkina TM, Beb–yakova NA. Role of the autonomic nervous system in the development of cardiac arrhythmias in cats with acute myocardial ischemia receiving thyroliberin. Bull Exp Biol Med 2003; 135:545–7. [ Links ]
23. Guo Y, Stein AB, Wu WJ, Zhu X, Tan W, Li Q, et al. Late preconditioning induced by NO donors, adenosine A1 receptor agonists, and d1–opioid receptor agonists is mediated by iNOS. Am J Physiol Heart Circ Physiol 2005; 289:H2251 –7. [ Links ]
24. Maslov LN, KrylatovAV, Lishmanov luB, Galo G, Ma K, Stakheev DL. The mechanism of antiarrhythmic action of the endogenous ORL1 receptor agonist nociceptin. Eksp Klin Farmakol 2004;67:32–5. [ Links ]
25. Villemagne PSR, Dannals RF, Ravert HT, Frost J. PET imaging of human cardiac opioid receptors. Eur J Nucl Med 2002;29:1385–8. [ Links ]
26. Gross ER, Hsu AK, Gross GJ. GSK3beta inhibition and K(ATP) channel opening mediate acute opioid–induced cardioprotection at reperfusion. Basic Res Cardiol 2007; 102:341–9. [ Links ]
27. Kweon TD, Nam SB, Chang CH, Kim MS, Lee JS, Shin CS, et al. The effect of bolus administration of remifentanil on QTc interval during induction of sevoflurane anaesthesia. Anaesthesia 2008;63:347–51. [ Links ]
28. Schultz JEJ, Gross GJ. Opioids and cardioprotection. Pharmacol Ther 2001; 89:123–37. [ Links ]
29. 29. Barron BA. Opioid peptides and the heart. Ed Cardiovasc Res 1999;43:13–6. [ Links ]














