Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Archivos de cardiología de México
versão On-line ISSN 1665-1731versão impressa ISSN 1405-9940
Arch. Cardiol. Méx. vol.79 no.1 Ciudad de México Jan./Mar. 2009
Artículo de investigación: cardiología clínica
Ten–year clinical and echocardiographic follow–up of patients undergoing percutaneous mitral commissurotomy with Inoue balloon
Comisurotomía mitral percutánea con balón de Inoue: seguimiento clínico y ecocardiográfico a 10 años
Mauricio López–Meneses*, Marco Antonio Martínez Ríos, Jesús Vargas Barrón, Jesús Reyes Corona y Francisco Sánchez
Instituto Nacional de Cardiología Ignacio Chávez, Tlalpan, México D.F. , México.
*Corresponding author.
Correo electrónico: maulm@yahoo.com.
Recibido el 31 de octubre de 2007.
Aceptado el 19 de septiembre de 2008.
Abstract
Percutaneous mitral commissurotomy (PMC) has emerged as an effective nonsurgical technique for the treatment of patients with symptomatic mitral stenosis. This report highlights the immediate and long–term follow–up results of this procedure in an unselected cohort of patients with rheumatic mitral stenosis from a single center.
PMC with Inoue balloon was performed in 70 patients in a 2–year period (1993–1994). Age of patients ranged from 18 to 67 years (mean 38 ± 11). Atrial fibrillation was present in 18 (30%) patients. A detailed clinical and echocardiographic (two–dimensional, continuous–wave Doppler and color–flow imaging) assessment was done at follow–up. The procedure was technically successful in 61 (85%) patients with an increase in mitral valve area (MVA) from 0.96 ± 0.2 to 1.7 ± 0.28 cm2 (P < .001) and a reduction in mean trans–mitral gradient from 14.3 ± 4.8 to 6.0 ± 2.8 mmHg (P < .01). Mitral regurgitation appeared or worsened in 25 (30%) patients, of which 3 (4%) developed severe mitral regurgitation. Urgent mitral valve replacement was performed in these 3 patients. Data of 52 patients followed over a period of 105 ± 10 months revealed MVA of 1.4 ± 0.4 cm. Elective mitral valve replacement was done in 14 (23%) patients. Mitral restenosis diagnosed with echocardiography was seen in 24 (50%) patients, of which 14 were having recurrence of class III or more symptoms and were treated with surgery. Thus, percutaneous mitral commissurotomy is an effective and safe procedure and over 2/3 of the patients were event–free at the end of follow–up. The benefits are sustained in most of these patients on long–term follow–up.
Keywords: Percutaneous mitral commissurotomy; Long term follow–up; Mitral stenosis.
Resumen
La comisurotomía mitral percutánea (CMP) es una excelente alternativa no quirúrgica en pacientes con estenosis mitral sintomática. El objetivo de este trabajo es reportar los resultados inmediatos y a largo plazo de una cohorte de pacientes atendidos en el Instituto Nacional de Cardiología.
Se realizó una CMP en 70 pacientes utilizando el balón de Inoue, en el período 1993–1994. Su intervalo de edad fue de 18–67 años (media ± desviación estándar de 38 ± 11 años), la fibrilación auricular estaba presente en 18 (30%) de los pacientes. Se realizó un análisis ecocardiográfico cuidadoso durante la fase intrahospitalaria y en el seguimiento. El procedimiento fue técnicamente exitoso en 61 (85%) pacientes, con un incremento en el área valvular mitral de 0,96 ± 0,2 a 1,7 ± 0,28 cm2 (p < 0,001) y una reducción en el gradiente medio de 14,3 ± 4,8 a 6,0 ± 2,8 mmHg (p < 0,01). Se observó insuficiencia mitral en 25 (30%) de los pacientes, pero sólo en 3 (4%) fue de grado severo y fue necesario un cambio valvular mitral urgente. Los hallazgos ecocardiográficos de los 52 pacientes con un seguimiento de 105 ± 10 meses demostraron un área valvular promedio de 1,4 ± 0,4 cm2. El cambio valvular mitral electivo se realizó en 14 (23%) pacientes. La reestenosis mitral se diagnosticó por ecocardiograma en 24 (50%) pacientes, de los cuales 14 tuvieron recurrencia de síntomas con clase funcional III y fueron sometidos a cirugía de cambio valvular mitral. Se puede concluir que la comisurotomía mitral percutánea es un procedimiento efectivo y seguro, y dos terceras partes de los pacientes se encuentran libres de eventos recurrentes a largo plazo.
Palabras clave: Comisurotomía mitral percutánea; Seguimiento a largo plazo; Estenosis mitral.
Percutaneous mitral commissurotomy (PMC) has been accepted as an alternative to surgical mitral commissuroto–my in the treatment of patients with symptomatic rheumatic mitral stenosis. PMC produces good immediate hemodynamic and clinical improvement in most patients with mitral stenosis and the safety and immediate efficacy have been widely demonstrated for > 10 years. However, the consequences of its widespread use are less well known, because large published series report mainly midterm follow–up1–4.
The aim of the present study was to describe and analyze long–term clinical and echocardiographic follow–up, in which clinical events are detailed according to the quality of the immediate results.
Material and methods
From January 1993 to December 1994, a consecutive series of 70 patients with mitral stenosis (mean age 38 ± 11) underwent PMC at the Interventional Cardiology Department of the National Institute of Cardiology Ignacio Chávez in Mexico City.
Indications for PMC included New York Heart Association (NYHA) functional class III or I V, and/or echocardiographic findings indicating a moderate to severe mitral stenosis and presence of no more than mild mitral regurgitation (MR). The usual contraindications to the procedure were previously detailed4–6.
Technique
All procedures were performed via antegrade transvenous approach with the Inoue balloon according to the stepwise technique, under echocardiographic guidance. Balloon size was selected according to body surface area (26 mm if < 1.5 m2, 28 mm if 1.5 to 1.7 m2, and 30 mm if > 1.7 m2). Left ventriculography was performed before and after the last balloon inflation.
Preprocedural and postprocedural assessments
Clinical status was determined by NYHA classification. All patients underwent and Echo–Doppler and transesophageal study before PMC. Evaluation included Wilkins scoring, mitral valve area (MVA) calculation (pressure half–time method), and mitral regurgitation (graded as none, mild, moderate, or severe by color Doppler semiquantitative method). The degree of MR was assessed according to Sellers' classification on left ventriculography in a 30° right anterior oblique view. If a > 1 grade discrepancy in MR grading existed between left ventriculography and Doppler, both studies were reviewed, and a consensus was reached finally.
Follow–up
Clinical follow–up was performed at 1–year intervals since 1993. Clinical evaluation was performed by direct or telephone interview with the patient. The interviewer was masked to the echocardiographic score and immediate outcome of PMC. Follow–up was concluded in January 2005 in 52 of 61 patients (85%) with a successful procedure, and the median duration was 105 ± 10 months.
Definitions
Good immediate results were defined by a composite end point that associated a mitral valve area > 1.5 cm2 and regurgitation moderate or less. Clinical improvement after PMC was considered as NYHA class < 2.
End points of follow–up were cardiac death, mitral valve replacement (MVR), repeat PMC, and clinical evaluation according to the New York Heart Association (NYHA) functional classification of congestive heart failure. Restenosis was defined as loss of 50% of initial gain and MVA < 1.5 cm2. Survival status was censored at the time of surgery or repeat dilatation.
Statistical analysis
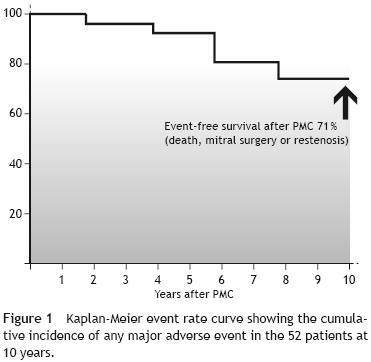
Continuous variables are presented as mean (± SD). Categorical data were expressed as percentages. A value of P < .05 was considered significant. Discrete data were compared by χ2 analysis and comparisons before and after PMC were made by using paired Student's 2 tailed t test. Event–free survival rate for several single and composite end points was estimated with the use of Kaplan–Meier analysis.
Results
Baseline characteristics and initial results are displayed in table 1. The Inoue balloon diameter was 27.4 ± 2.1 mm. Global results were summarized as good results in 61 (87%), insufficient opening in 6 (9%). Severe mitral regurgitation was observed in 3 (4%) cases and required in–hospital mitral surgery. Two patients showed an atrial septal defect with a Qp/Qs flow ratio of > 1.5:1, which closed spontaneously as demonstrated at 4–year follow–up. No other adverse events occurred.
After PMC, the mean valve area increased from 0.96 ± 0.2 to 1.7 ± 0.28 cm2 (P < .001) and mean gradient decreased from 14.3 ± 4.8 to 6.0 ± 2.36 mmHg (P < .01). Mitral regurgitation was mild in 44 (72%) patients and moderate in 4 (7%) patients. The late MVA was 1.42 ± 0.41 cm2 and the mean gradient was 6.3 ± 3.3 mmHg (table 1).
Late results
Follow–up events were: (1) death in 1 patient due to a non cardiac cause; (2) mitral replacement in 14 (22%), 2 patients underwent surgery indicated by mitral regurgitation prosthetic endocarditis in 2, and restenosis in 10. In four patients. it was necessary to replace the aortic valve due to stenosis (table 2).

In the 52 patients with follow–up, 10–year actuarial rate was 71% (37 patients) for survival with no need of surgery or repeated dilatation (fig. 1). In 47 (77%) patients with ecochardiographic follow–up, restenosis was observed in 24 (50%) who met the restenosis definition (MVA < 1.5 cm2) but only 14 were in functional class >3 and were treated with surgery. Several variables (age, sex, cardiac rhythm, Wilkins score, postprocedural MVA, MR and mean transmitral gradient) were tested as potential predictors of event–free survival or restenosis. None variable were statistical associated probably for small number of patients.
Discussion
Percutaneous commissurotomy techniques have developed significantly since the early attempts of catheter valvuloplasty were pioneered at our institution in the 1950s by Rubio, Limón and Soní7. Today, PMC for mitral stenosis is considered the method of choice in selected patients for several reasons. First, PMC is a nonsurgical method with results similar to those of surgical intervention but without the unnecessary risks and complications of general anesthesia and an extracorporeal circulation pump. Second, both acute and long term results of randomized trials comparing PMC vs. surgical commissurotomy are comparable and depict similar restenosis rates4–14.
The overall success rate has been 95% in several studies, and the "hospital" (30–day) mortality rate was 4.5%. The early death rate is similar to that observed by other investigators (from 1% to 9%) and in the multicenter NHLBI Registry15.
Our study demonstrates that PMC for MS was successfully completed in 87% of patients in whom it was attempted. The actuarial 10–year survival was 98%; the event–free survival was 71% in the 52 patients that completed follow up. Most of the patients were functionally improved initially; this improvement was largely maintained on further follow–up.
In several studies Wilkins score was the best periprocedural predictor of mitral opening, but the procedural result (mitral area and regurgitation) was the most important independent predictor of major event–free survival. Other independent predictors of major adverse cardiac events were atrial fibrillation, pulmonary artery wedge pressure (PAWP) greater than 18 mmHg and moderate to severe tricuspid insufficiency11–24.
Our report involves PMC in a population of mostly middle–aged men with a low Wilkins score, this fact explains the favorable results, with a low incidence of complications. Some increases in regurgitation were observed at follow–up, but severe MR was a rather unexpected complication. In our study, we found a 46% with moderate MR, without clinical impairment at 10 years. Clinical implications of stable moderate regurgitation require further investigation in long–term studies. Recently, Kim et al25 reported long–term prognostic factors of significant MR after PMC. Echocardiographic and clinical follow–up data were analyzed in 380 patients that underwent PMC with the Inoue balloon. The 8–year event–free survival rate was significantly lower in patients with significant MR than in those without (47 ± 8% versus 83 ± 3%, P < .001) and was significantly higher in patients with commissural versus noncommissural MR (63 ± 11% versus 29 ± 11%, P < .001). Of the 47 patients with significant MR, who were followed for 74 ± 29 months, 19 patients (40%) underwent mitral valve replacement, and 28 patients (60%) received medical treatment only.
Restenosis is an ambiguous definition that includes a mixture of poor results, very early area loss, true restenosis and disease progression. Its definition can be made on a clinical basis or in terms of mitral area. In several studies, the restenosis rate after PMC has ranged from 3 to 50% at 1 to 3 years. Our study demonstrated 24 (50%) patients with echocardiographic restenosis but only 25% with clinical deterioration.
Several studies are available regarding long–term follow–up of PMC, the long–term event–free survival was between 75% and 97% and depended on the length of follow–up. In our study, the event–free survival was of 71% at 10 years.
Other studies have reported 4–and 5–year results after PMC. Cohen et al20 and coworkers reported follow–up data on 145 patients for a period averaging 36 ± 20 months. The actuarial 5–year survival was 76%, and actuarial event–free survival was 51%, which is lower than that seen in the present study.
In the preliminary report from the NHLBI Registry, at a mean follow–up of 3.2 years, at 4 years the actuarial survival was 84% and the actuarial event–free survival was 60%15.
Multivariate predictors of mortality included NYHA class IV, higher echocardiographic score, higher postprocedural PA systolic pressure, and higher left ventricular end diastolic pressure19–41.
Our study has some limitations. First, it concerned a single center cohort study, although patients were representative of a population that underwent PMC contemporaneously. Second, information concerning long–term follow up was available in only 52 patients (85%).
Our data show that the 10–year results of PMC are good in selected subgroups of patients. These findings of favorable mid–term results strengthen the previous conclusions that PMC should be the procedure of first choice in selected patients in centers with experience and skill in performing this procedure.
Conclusions
PMC is a safe and effective procedure for patients with mitral stenosis. This single–center series confirms the long–term efficacy of PMC in a large population comprising a variety of patient subsets. Patients with a good score obtain better initial and long–term results. Continuing good results can be expected in patients with favorable characteristics.
References
1. Seltzer A, Cohn KE. Natural history of mitral stenosis: a review. Circulation. 1972;45:878–90. [ Links ]
2. Mazur W, Parilak LD, Kaluza G, Defelice C, Raizner AE: Balloon valvuloplasty for mitral stenosis. Current Op Cardiol. 1999;14: 95–105. [ Links ]
3. Inoue K, Owaki T, Nakamura T. Application of transvenous mitral commissurotomy by a new balloon catheter. J Thorac Cardiovasc Surg. 1984;87:394–402. [ Links ]
4. Bonow RO, Carabello B, De León AC, Edmunds LH, Fredderly BJ, Freed MD, et al. ACC/AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Commitee on management of patients with valvular heart disease). J Am Coll Cardiol. 1998;32:1486–588. [ Links ]
5. Rubio AV, Limón LR, Soní J. Valvulotomia intracardíaca por medio de un catéter. Arch Inst Cardiol Mex 1953;23:183–6. [ Links ]
6. Herrmann HC, Wilkins G T, Abascal VM, Weyman AE, Block PC, Palacios I F. Percutaneous mitral balloon valvotomy for patients with mitral stenosis. Analysis of factors influencing early results. J Thorac Cardiovasc Surg. 1988;96:33–8. [ Links ]
7. Martínez–Ríos MA, Tovar S, Luna J, Eid–Lidt G. Percutaneous mitral commissurotomy. Cardiol Rev. 1999;7:108–16. [ Links ]
8. Tsuji T, Ikari Y, Tamura T, Wanibuchi Y, Hara K. Pathologic analysis of stenosis following percutaneous transluminal mitral commissurotomy. Catheter Cardiovasc Interv. 2002;57:205–10. [ Links ]
9. Fawzy ME. Percutaneous mitral balloon valvotomy. Catheter Cardiovasc Interv. 2007;69:313–21. [ Links ]
10. Wilkins G T, Weyman AE, Abascal VM. Percutaneus balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J. 1988;60:299–308. [ Links ]
11. Heger JJ, Wann LS, Weyman AE, Dillon JC, Feigenbaum H. Long–term changes in mitral valve area after successful mitral commissurotomy. Circulation. 1979;59:443–8. [ Links ]
12. Vahanian A, Cormier B, Iung B. Percutaneous transvenous mitral commissurotomy using the Inoue technique: international experience. Cathet Cardiovasc Diagn. 1994; Suppl 2:8–15. [ Links ]
13. Vahanian A, Michel PL, Cormier B, Vitoux B, Michel X, Slama M, et al. Results of percutaneous mitral commissurotomy in 200 patients. Am J Cardiol. 1989;63:847–52. [ Links ]
14. Cheng T, Tsung O, Holmes D. Percutaneous mitral valvuloplasty by the inoue balloon technique: the procedure of choice for treatment of mitral stenosis. Am J Cardiol. 1999; 84:624–8. [ Links ]
15. The NHLBI Balloon Valvuloplasty Registry Participants. Multicenter experience with balloon mitral commissurotomy. Circulation. 1992;85:448–61. [ Links ]
16. Reyes V P, Raju BS, Wynne J, Stephenson LW, Raju R, Fromm BS, et al. Percutaneous balloon valvuloplasty compared with open surgical commissurotomy for mitral stenosis. N Engl J Med. 1994; 331:961–7. [ Links ]
17. Nobuyoshi M, Hamasaki N, Kimura T, Nosaka H, Yokoi H, Yasumoto H, et al. Indications, complications, and short–term clinical outcome of percutaneous transvenous mitral commissurotomy. Circulation. 1989;80:782–92. [ Links ]
18. Abascal VM, Wilkins G T, O'Shea J P, Choong C Y, Palacios I F, Thomas JD, et al. Prediction of successful outcome in 130 patients undergoing percutaneous balloon mitral valvotomy. Circulation. 1990;82:448–56. [ Links ]
19. Herrmann HC, Ramaswamy K, Isner JM, Feldman TE, Carroll JD, Pichard AD, et al. Factors influencing immediate results, complications, and short–term follow–up status after Inoue balloon mitral valvotomy: a North American multicenter study. Am Heart J. 1992;124:160–246. [ Links ]
20. Cohen DJ, Kuntz RE, Gordon SPF, Piana RN, Safian RD, McKay RG, et al. Predictors of long–term outcome after percutaneous balloon mitral valvuloplasty. N Engl J Med. 1992;327: 1329–35. [ Links ]
21. Arora R, Kalra GS, Murty GS, Trehan V, Jolly N, Mohan JC, et al. Percutaneous transatrial mitral commissurotomy: immediate and intermediate results. J Am Coll Cardiol. 1994;23:1327–32. [ Links ]
22. Arora R, Nair M, Kalra GS, Nigam M, Khalilullah M. Immediate and long–term results of balloon and surgical closed mitral valvotomy: a randomized comparative study. Am Heart J. 1993; 125:1091–4. [ Links ]
23. Lung B, Cormier B, Ducimetiere P, Porte JM, Nallet O, Michel PL, et al. Immediate results of percutaneous mitral commissurotomy: a predictive model on a series of 1514 patients. Circulation. 1996;94:2124–30. [ Links ]
24. Palacios I F, Tuzcu ME, Weyman AE, Newell JB, Block PC. Clinical follow–up of patients undergoing percutaneous mitral balloon valvotomy. Circulation. 1995;91:671–6. [ Links ]
25. Kim MJ, Song JK, Song JM, Kang OH, Kim YH, Lee CW, et al. Long term outcomes of significant mitral regurgitation after percutaneous mitral valvuloplasty. Circulation. 2006;114: 2815–22. [ Links ]
26. Dean LS, Mickel M, Bonan R, Holmes DR, O'Neill WW, Palacios I F, et al. Four–year follow–up of patients undergoing percutaneous balloon mitral commissurotomy: a report from the National Heart, Lung, and Blood Institute balloon valvuloplasty registry. J Am Coll Cardiol. 1996;28:1452–7. [ Links ]
27. Chen CR, Cheng TO. Percutaneous balloon mitral valvuloplasty by the Inoue technique: A multicenter study of 4832 patients in China. Am Heart J. 1995;129:1197–203. [ Links ]
28. Orrange SE, Kawanishi D T, Lopez BM, Curry SM, Rahimtoola SH. Actuarial outcome after catheter balloon commissurotomy in patients with mitral stenosis. Circulation. 1997;95:382–9. [ Links ]
29. Pavlides GS, Nahhas G T, London J, Gangadharan C, Troszak E, Barth–Jones D, et al. Predictors of long–term event–free survival after percutaneous mitral valvuloplasty. Am J Cardiol. 1997;79: 1370–4. [ Links ]
30. Bassand J P, Schiele F, Bernard Y, Anguenot T, Payet M, Ba SA, et al. The double–balloon and Inoue techniques in percutaneous mitral valvuloplasty: comparative results in a series of 232 cases. J Am Coll Cardiol. 1991;18:982–9. [ Links ]
31. Palacios I F, Block PC, Wilkins G T, Weyman AE. Follow–up of patients undergoing percutaneous mitral valvotomy: analysis of factors determining restenosis. Circulation. 1989;79:573–9. [ Links ]
32. Desideri A, Vanderperren O, Serra A, Barraud P, Petitclerc R, Lesperance J, et al. Long–term (9 to 33 months) echocardiographic follow–up after successful percutaneous mitral commissurotomy. Am J Cardiol. 1992;69:1602–6. [ Links ]
33. Ben Farhat M, Ayari M, Maatouk F, Betbout F, Gamra H, Jarrar M, et al. Percutaneous balloon versus surgical closed and open mitral commissurotomy: seven–year follow–up results of a randomized trial. Circulation. 1998;97:245–50. [ Links ]
34. Lung B, Cormier B, Ducimetiere P, Porte JM, Nallet O, Michel PL, et al. Functional results 5 years after successful percutaneous mitral commissurotomy in a series of 528 patients and analysis of predictive factors. J Am Coll Cardiol. 1996;27: 407–14. [ Links ]
35. Ommen SR, Nishimura RA, Grill DE, Holmes DR, Rihal CS. Long–Term results of percutaneous mitral balloon valvulotomy with closed transventricular mitral commissurotomy at a single north american institution. Am J Cardiol. 1999;84:575–7. [ Links ]
36. Hernandez R, Bañuelos C, Alfonso F, Goicolea J, Fernandez–Ortiz A, Escaned J, et al. Long–term clinical and echocardiographic follow up after percutaneous mitral valvuloplasty with the inoue balloon. Circulation. 1999;99:1580–6. [ Links ]
37. Padial LR, Abascal VM, Moreno PR, Weyman AE, Levine RA, Palacios I F. Echocardiography can predict the development of severe mitral regurgitation after percutaneous mitral valvulo–plasty by the inoue technique. Am J Cardiol. 1999;83:1210–3. [ Links ]
38. Lung B, Garbarz E, Michaud P, Helou S, Farah B, Berdah P, Michel PL. Late results of percutaneous mitral commissurotomy in a series of 1024 patients. analysis of late clinical deterioration: frequency, anatomic findings and predictive factors. Circulation. 1999;99:3272–8. [ Links ]
39. Hildick S, Taylor G, Shapiro L. Inoue balloon valvuloplasty: long term clinical and echocardiographic follow–up of a predominantly unfavourable population. Eur Heart J. 2000;21:1690–7. [ Links ]
40. Martinez–Reding J, Cordero A, Kuri J, Martinez–Rios MA, Salazar E. Treatment of severe mitral stenosis with percutaneous balloon valvotomy in pregnant patients. Clin Cardiol.1998;21: 659–63. [ Links ]
41. Lung B, Garbarz E, Michaud P, Fondard O, Helou S, Kamblock J. Immediate and mid–term results on repeat percutaneous mitral commissurotomy for restenosis following earlier percutaneous mitral commissurotomy. Eur Heart J. 2000;21:1683–9. [ Links ]














