Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos de cardiología de México
versión On-line ISSN 1665-1731versión impresa ISSN 1405-9940
Arch. Cardiol. Méx. vol.78 no.4 Ciudad de México oct./dic. 2008
Investigación clínica
Improvement of diastolic function after regression of left ventricular hypertrophy
Mejora de la función diastólica tras regresión de la hipertrofia ventricular izquierda
Raúl Teniente–Valente,* Sergio Solorio,** Enrique Vargas–Salado,*** Carlos Aguirre–Vázquez,* Martha A Hernández–González,** José Antonio Olvera–Lopez,* Leticia Rodríguez–Mariscal,* Miguel Angel Luna–Ruiz,*** José Manuel Guillén Contreras,** Blanca Olivia Murillo Ortiz**
* Cardiology Department. UMAE 1 Bajío, Mexican Institute of Social Security. Leon, Guanajuato, Mexico.
** Unit of Clinical Research, UMAE Bajío 1. Mexican Institute of Social Security. Leon, Guanajuato, Mexico.
*** School of Medicine. University of Guanajuato. León, Guanajuato, Mexico.
Correspondence:
Sergio Eduardo Solorio Meza.
Unit of Clinical Research, UMAE Bajío 1.
Mexican Institute of Social Security.
Blvd Lopez Mateos esq. Insurgentes SN.
Col. Los Paraísos. 37320
Leon, Guanajuato, Mexico.
Tel. (52) 477 7174800 ext 31742,
E–mail: sergio.solorio@imss.gob.mx; dr.teniente@yahoo.com
Recibido: 12 de diciembre de 2007
Aceptado: 15 de abril de 2008
Abstract
Objective: To evaluate the diastolic function after regression of left ventricular hypertrophy, in mild to moderate hypertension treated with angiotensin converting enzyme(ACE) inhibitor and, if necessary, with a diuretic.
Methods: Ninety–eight hypertensive patients with left ventricular hypertrophy (LVH) and abnormal left ventricle diastolic function indexes received captopril (Capotena® ) 50 to 200 mg/day plus chlortalidone during 12 months to reach blood pressure control, defined as a diastolic blood pressure < 90 and systolic blood pressure < 140 mm Hg. Left ventricular (LV) mass index was calculated by M mode and two–dimensional echocardiography, and left ventricular diastolic function was assessed by transmitral pulsed Doppler ultrasound every 3 months.
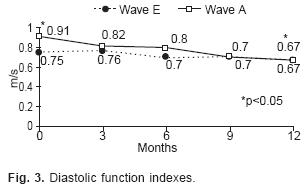
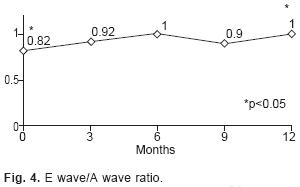
Results: Sixty–three patients were women and 35 were men, mean age was 53.4 ± 8.4 years (range 34–70). Thirty–six patients had mild (36.7%) and 62 (63.3%) moderate hypertension. Treatment reduced significantly both systolic pressure from 165 ± 13 to 137 ± 12.9 mm Hg (p < 0.05) and diastolic pressure from 99 ± 8.6 to 86 ± 6.37 mm Hg (p < 0.05). LV mass index decreased from 155.4 ± 32.9 to 121.7± 29.14 g/m2 (p < 0.05). Late diastolic filling velocity (A wave) and the ratio of E/A waves improved (p < 0.05), but early diastolic filling velocity (E wave) and isovolumetric relaxation time did not change with treatment.
Conclusions: Some indexes of diastolic function improved after regression of left ventricular hypertrophy and good blood pressure control with captopril and chlortalidone.
Key words: Diastolic function. Left ventricular hypertrophy. Hypertension.
Resumen
Objetivo: Evaluar la función diastólica después de revertir la hipertrofia ventricular izquierda, en hipertensión leve a moderada tratada con inhibidores de la enzima convertidora angiotensina (ECA) y, si era necesario, con un diurético.
Métodos: Noventa y ocho pacientes hipertensos con hipertrofia ventricular izquierda e índices de función diastólica anormal del ventrículo izquierdo recibieron captopril 50 a 200 mg/día (Capotena®) más clortalidona durante 12 meses para lograr el control de la presión arterial, definido como presión diastólica < 90 mm Hg y presión sistólica < 140 mm Hg. El índice de masa ventricular izquierdo fue calculado por ecocardiografía modo M y bidimensional y la función diastólica ventricular izquierda fue determinada por Doppler pulsado transmitral cada 3 meses.
Resultados: Sesenta y tres pacientes eran del género femenino y 35 del género masculino, con edad de 53.4 ± 8.4 años (rango 34–70). Treinta y seis pacientes (36.7%) tenían hipertensión leve y 62 (63.3%) hipertensión moderada. El tratamiento redujo significativamente tanto la presión sistólica de 165 ± 13 a 137 ± 12.9 mm Hg (p < 0.05) como la presión diastólica de 99 ± 8.6 a 86 ± 6.37 mm Hg (p < 0.05). El índice de masa ventricular izquierda disminuyó de 155.4 ± 32.9 a 121.7 ± 29.14 g/m2 (p < 0.05). La velocidad diastólica de llenado tardío (onda A) y la relación E/A mejoraron (p < 0.05), pero la velocidad diastólica de llenado temprano (onda E) y el tiempo de relajación isovolumétrica no cambiaron con el tratamiento.
Conclusiones: Algunos índices de la función diastólica mejoraron después de la regresión de la hipertrofia ventricular izquierda y del buen control de la presión arterial con el captopril y clortalidona.
Palabras clave: Función diastólica. Hipertrofia ventricular izquierda. Hipertensión.
Background
Left ventricular hypertrophy (LVH) is often a complication of systemic arterial hypertension, especially in uncontrolled hypertension. LVH increases the risk of coronary artery disease, stroke, ventricular arrhythmias, sudden death, and congestive heart failure.1,2 LVH produce, at least in part, left ventricle wall stiffness and alteration of left ventricle diastolic function (LVDF).3–6 Other factors can alter LVDF, including aging, increased heart rate, high left ventricle filling pressure, and adrenergic hyperactivity.7 Altered LVDF is associated to LVH, it can be asymptomatic or precipitate congestive heart failure (CHF) with normal systolic function. A condition found in 51% of patients with systemic arterial hypertension, increasing their morbidity and mortality.8
The regression of LVH has been documented to occur with appropriate antihypertensive drugs, except with vasodilators, such as hydralazine and minoxidil. The most effective drugs to reverse LVH are angiotensin–converting enzyme (ACE) inhibitors.9,10 However, results from several studies that evaluated diastolic function after LVH had been corrected are contradictory.11–17
These results could be explained mainly based on differences in the duration of the studies and, in some cases, by the poor hypertension control. Thus, if the systolic overload of the LV is eliminated through suitable blood pressure control, regression of the LVH could be expected, and therefore the stiffness of the LV wall might be corrected reversing the diastolic dysfunction. The objective of this study was to evaluate the effect of treatment with captopril and whether a diuretic was necessary for LVH and LVDF in patients with mild and moderate high blood pressure (HBP).
Patients and methods
Patients were eligible for enrollment when:
1. Mild HBP (arterial diastolic pressure higher than 90 but lower than 99 mm Hg and/or arterial systolic pressure higher than 140 but lower than 160 mm Hg); or moderate HBP (arterial diastolic pressure higher than 99 but lower than 115 mm Hg and/or arterial systolic pressure higher than 160 but lower than 180mmHg);
2. LVH determined by echocardiogram (left ventricular mass > 110 g/m2 in women and > 134 g/m2 in men);18
3. Altered LVDF (isovolumetric relaxation time higher than 73 ± 12 msec; maximum speed of wave E diminished below 86 ± 16 cm/sec, maximum auricular contraction speed over 56 ± 13 cm/sec, and a relationship E wave/A wave ratio lower than 1.6 ± 0.5);19
4. Normal LV systolic function (ejection fraction > 50%) by echocardiogram Doppler (echo–Doppler).
Patients with secondary arterial hypertension, myocardial ischemia (stable or unstable angina, acute myocardial infarction, silent ischemia), resting electrocardiogram (ECG) with ischemia, lesion or necrosis; positive ECG for myocardial ischemia during an exercise treadmill test; LV wall motion abnormalities in the echocardiogram; valvular heart disease, overweight higher than 20%, creatinine plasma levels higher than 1.6 mg/dL, abnormal hepatic function tests, and well–known hyper–sensitivity to captopril or chlortalidone were excluded.
Elimination criteria were: Drug side effects or poor tolerance to medications, rapidly progressive hypertension, and development of any cerebrovascular complication or abnormal kidney function test. All patients gave their informed written consent to participate in the study. The protocol was approved by the Institutional Ethics Committee.
Study design
A prospective, longitudinal study was performed in 98 hypertensive patients. Sample size was calculated considering a 15% prevalence rate of hypertension, in the population of the city of León with LVH (30% of them), and expecting an improvement in LVH of at least 50%, a power of 90%, and an a value of 5%. Eligible patients were withdrawn from their antihypertensive medication two weeks before tests to confirm mild or moderate hypertension. A full medical history and physical examination were obtained from each patient. They had a laboratory screening (BH, fasting blood glucose, urea, creatinine, electrolytes, total cholesterol and triglycerides), ECG at rest and during a stress test with Bruce protocol and an echo–Doppler. Patients meeting all the selection criteria were invited to participate. All of them were folio wed–up during 12 months; once a month, we evaluated them with physical examination, laboratory tests (blood glucose, urea, creatinine, potassium), and adjusting the antihypertensive medication. An echo–Doppler was recorded every 3 months until completing the 12 months.
Arterial blood pressure measurement and treatment follow–up
Arterial blood pressure was measured indirectly with a standard sphygmomanometer (bladder size, 12.5 cm wide and 48 cm long), with the patient comfortably seated, arms resting at heart level, without having smoked or drunk coffee within the last 30 minutes. Systolic blood pressure (SBP) was indicated by phase I of Korotkoff sounds (sudden appearance of sounds); while diastolic BP (DBP) was marked by phase V (all sounds disappear completely). Each measurement was made in triplicate after 5 minutes of rest; at least 2 minutes were allowed between successive measurements and the mean value was recorded. The main goal of treatment was to achieve a SBP below 140 and a DBP below 90 mm Hg or to reduce 20 mm Hg the systolic and/ or diastolic BP in relation to the basal figures. Initial captopril dose was 25 or 50 mg (Capotena®) twice a day for mild or moderate HBP, respectively. This dose was adjusted every month according to the arterial blood pressure measurements, up to a maximum of 200 mg/day. When patients did not reach the treatment goal, a diuretic (Chlortalidone) was added at a dose of 12.5 mg/day that could be increased to 25 mg/day. To monitor adherence to treatment, patients were asked to bring all their medications to each appointment and tablets were counted. Antihypertensive dosage adjustments were required only in the first 4 months of the study.
Echo–Doppler measurements
Echocardiograms were recorded in the M, B/D, and Doppler modes using a Toshiba equipment (Toshiba Sonolayer SSA–270A, Tochigi Ken 329–26, Japan), with a 3.5–MHz transducer. Patients were in the left lateral decubitus position with the transducer placed on the 4th or 5th left intercostal space. Recordings were made preferably in a long axis view at the level of the tip of the papillary muscles according to the recommendations of the ASE.20 The following measurements were recorded: interventricular septum thickness (IVS), left ventricular posterior wall (LVPW), end–diastolic and end–systolic diameter of the left ventricle (LVED, LVES). Fractional shortening and ejection fraction (EF) were estimated. LV mass was calculated using the formula proposed by Devereux 21 as follows: LV Mass = 1.04 (LVPW+IVS+LVED)3–(LVED)3–13.6. Results were corrected for each patient's body surface area (BSA) and expressed in g/m2 BSA.
Left ventricular filling was obtained as follows: Mitral velocities were obtained by placement of the Doppler sample volume within the valve leaflets just distal to the annulus. The sample volume was aligned parallel to the interventricular septum and then adjusted in the non visualized plane until the optimal wave form was found, at the end of non forced expiration. Measurements were obtained for LV isovolumetric relaxation time, early diastolic "E" wave associated with the rapid left ventricular filling phase, followed by an "A" wave associated with atrial contraction. The E wave/A wave ratio was calculated. All echo–Doppler recordings were made blind in relation to patient HBP control, as well as to previous recordings or results.
Statistical analysis
Data collected were assumed to be normally distributed and are described as mean and standard deviation. To test the differences in the parameters evaluating LVH and LVDF a one–way ANO–VA was used. The level of significance chosen was the 5% (p < 0.05). Post hoc analysis was made using Scheffe's test. The statistical program NCSS version 2001 was used for the calculations.
Results
Of the 342 evaluated patients, 98 met the selection criteria and formed the study group. Their mean age was 53.4 ± 8.4 years (range 34 –70). There were 63 women and 35 men (Table I). All of the patients were known to be hypertensive for at least 1 year and all were taking antihypertensive drugs different from the medications used in this study. Mild HBP was present in 36 patients and moderated HBP in the remainder. Only 74 patients completed the study; 18 abandoned it, 5 had persistent cough with medication, and 1 presented a significant elevation in blood glucose.

Drug therapy: The average initial captopril dose was 82.9 ± 38.9 mg/day and the average final dose was 167.57 ± 46.58 mg/day; 34 patients required Chlortalidone at a dose of 25 mg/day.
Blood pressure measurements: All patients had their SBP or DBP or both reduced by at least 20 mm Hg after 12 months of treatment. SBP diminished from 165 ± 13 to 137 ± 13 mmHg(p< 0.05); DBP lowered from 100 ± 8.7 to 86.7 ± 6.4 mmHg (p < 0.05) (Fig. 1). In 26 patients, it was not possible to diminish the SBP below 140 mm Hg and in 5 more it was not possible to diminish DBP to less than 90 mm Hg.

Left ventricular mass: After 12 months of treatment, LVPW diminished from 12.2 ± 1.4 to 10.9 ±1.36 mm (p < 0.05); IVS thickness was reduced from 12.8 ± 1.5 to 11.4 ± 1.46 mm (p< 0.05) and LVED decreased from 46.2 ± 5.17 to 43.9 ± 4.5 mm (p < 0.05). The LVES did not change in value (26 ± 4.7 and 26.6 ± 4.03; p = ns) (Table II). The LV mass diminished significantly from 155.4 ± 32.9 to 121.7 ± 29.14 g/m2 BSA (p < 0.05) after treatment, as shown in Figure 2.

Diastolic function indexes: After the 12–month period, LV isovolumetric relaxation diminished from 105 ± 18 to 104.1 ± 23.73 msec (p = ns). The maximum wave E speed decreased from 75 ± 0.25 to 67 ± 0.19 cm/sec (p = ns), the maximum wave A speed lowered significantly from 91 ± 0.3 to 67 ± 0.16 cm/sec (p < 0.05) (Fig. 3), and the E wave/A wave ratio decreased from 0.82 ± 0.11 to 1 ± 0.28 (p < 0.05) (Table III and Fig. 4).
Discussion
As in similar studies, we documented a significant 21 % regression of the LV mass, a reduction that is larger than previously reported of about 15%.8,9 The difference could be explained by the higher captopril dose, use of diuretics, agents known to reduce LV diastolic diameter, and the longer observation period in our study.8,9 Shahi et al.22 reported a similar reduction in LV mass (22%) in their 18 month study on 25 hypertensive patients. These authors used a similar combination of captopril and a diuretic to control HBP. They did no find changes in LVDF after 9 or 18 months of treatment.
Thus, contradictory results have been found in relation to LVDF and regression of LVH in hypertension. A clear improvement in diastolic function was documented by White et al.14 They studied nine hypertensive patients with LVH and altered diastolic function. None of the patients had received any drug treatment before the study, and they prescribed metoprolol at an average dose of 167 mg/day during 6 months. They reported a significant 11% decrease of the LV mass (p < 0.05). The rate of LV fast filling (measured by nuclear medicine) improved from 1.89 ± 0.24 to 2.09 ± 0.27 end diastolic volume/sec (p < 0.01). Trimarco et al.12 treated hypertensive patients with a (3–blocker (tertatolol) and showed a reduction in HBP, regression of the LVH, and improvement in diastolic function, although half of the patients had abnormal systolic function at the beginning of the study. The reduction in BP and the sympathetic inhibition could be responsible for the improvement. However, other investigators have not been able to confirm these results with (3–blockers.16 Habid et al.23 studied 27 hypertensive patients with LVH and diastolic dysfunction to whom they administered long acting nifedipine or diltiazem for 7 months. They observed a 34% decrease in LV mass and an improvement in diastolic function. All of their results were statistically significant and were not different from those observed in a control group of normotensive subjects. LVH regression in this 12 study is larger than in any other reports8,9 including ours. On the other hand, Szlachcic et al.24 in a controlled randomized double blind study on 24 patients with slightly moderate hypertension, LVH, and alteration in diastolic function and treated with either diltiazem or a placebo during 16 weeks, demonstrated a 10% regression in ventricular hypertrophy in the active treatment group. However, they did not record indexes of diastolic function. Zakynthinos et al.25 reported that after 6 months of treatment with losartan, an angiotensin II receptor blocking agent, LV mass was reduced in 6.2% in a group of patients with mild or moderate HBP but diastolic dysfunction was not modified.
Although long term treatment of hypertension is known to result in regression of existing left ventricular hypertrophy, the effect of hypertension treatment on myocardial function is less well understood. Solomon et al.25 in the VALIDD study (a multicentric study) only a small but significant improvement associated with blood pressure lowering was observed, whereas in other studies no changes were observed in diastolic function.26,27
This study was performed in chronic hypertensive patients who reached the proposed treatment goal for their HBP. Further, our results are in agreement with previous observations that an ACE inhibitor in combination with a diuretic is able to control the hypertension in over 90% of cases with mild to moderate disease. These patients had been diagnosed at least one year before and were receiving some form of drug treatment but with poor BP control. In our study, there were more patients with moderated HBP than with mild HBP. All of the patients had important LVH, alteration of the LV diastolic filling pressure, prolonged myocardial relaxation, and a changed compliance (type I of Tajik) usually observed in a hypertrophic heart with normal ventricular size.
Based on the present evidence, an improvement in LVDF would require sustained normalization of the BP level to eliminate the hemodynamic overload. This has been demonstrated in patients with LVH and diastolic dysfunction secondary to aortic stenosis by Villari et al.28 These latter authors found a larger reduction in LVH followed by recovery in LVDF, which required from months to years for normalization. This finding might be due, initially, to improvement in hypertrophic cardiomyocytes and, in the long term, to reduction in collagen content, which plays a role in myocardial stiffness.28
Study limitations: Magnetic resonance imaging is considered the ideal method for the determination of LV mass because of its high spatial resolution, generally good image quality, and ability to reconstruct the heart's shape in three dimensions. However, it is not widely used clinically because of higher costs, reduced availability, and limited access for critically ill patients or patients with implanted electronic devices (for example, pacemakers and defibrillators).29 The superiority of 3–D echocardiographic LV mass calculations over values calculated from M–mode–derived or 2–D echocardiography has been convincingly shown. Current limitations include the requirement of regular rhythm, relatively poorer image quality of real–time 3–D echocardiography as compared to 2–D images, and the time necessary for off–line data analysis. However, the greater number of acquired data points, the lack of geometric assumptions, increasingly sophisticated 3–D image, and measurements solutions set off these limitations.30 Echocardiographic imaging with single dimensional (M mode) and two–dimensional techniques is the most widely available clinical tool to detect LV hypertrophy, as determined by the calculated LV mass. Echocardiographic techniques have the advantage of being widely available, non–invasive, and relatively inexpensive. However, echocardiography is limited by imaging artefacts and by the planar nature of the imaging technique when the LV cavity is misshapen. Indeed, each step in LV mass measurement is a potential source of variability. In M–mode measurement, differences of approximately 5% may translate into differences in LV mass between 8% and 15%, which can represent about 50 g. This variability can be attributed particularly to the measurement of wall thicknesses and border layer definition.31
Conclusion
Improvement in most indexes of LVDF and regression of the LVH were observed when an appropriate control of HBP had been achieved with captopril alone or plus chlortalidone in patients with mild or moderate HBP, LVH, and alteration of the diastolic function. The changes are linked to obtaining a proper control of blood pressure and the time of its maintenance.
References
1. LEVY D, GARRISON RJ, SAVAGE DD, KANNEL WB, CASTELLI WP: Prognostic implications ofechocardiographically determined left ventricular mass in The Framingahm Heart Study. N Engl J Med 1990; 322: 1561–1566. [ Links ]
2. KOREN MJ, DEVEREUX RB, CASALE PN, SAVAGE DD, LARAGH JH: Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med 1991; 114: 345–352. [ Links ]
3. HANRATH P, MATHEY DG, SIEGERT R, BLEIFELD W: Left ventricular relaxation and filling pattern in different forms of left ventricular hypertrophy: an echocardiographic study. Am J Cardiol 1980; 45: 15–23. [ Links ]
4. FOUAD FM, SLOMINSKI JM, TARAZI RC: Left ventricular diastolic function in hypertension: relation to left ventricular mass and systolic function. J Am Coll Cardiol 1984; 3: 1500–6. [ Links ]
5. DRESLINSKI GR, FROHLICH ED, DUNN FG, MESSERLI FH, SUAREZ DH, REISIN E: Echocardiographic diastolic ventricular abnormality in hypertensive heart disease: atrial emptying index. Am J Cardiol 1981; 47: 1087–1090. [ Links ]
6. INOUYE I, MASSIE B, LOGE D, TOPIC N, SILVERSTEIN D, SIMPSON P, TUBAU J: Abnormal left ventricular filling: an early finding in mild to moderate systemic hypertension. Am J Cardiol 1984; 53: 120–126. [ Links ]
7. HESS OM, SCHNEIDER J, KOCH R, BAMERT C, GRIMM J, KRAYENBUEHL HP: Diastolic function and myocardial structure in patients with myocardial hypertrophy. Circulation 1981; 63: 360–371. [ Links ]
8. VASAN RS, LARSON MG, BENJAMIN EJ, EVANS JC, REISS CK, LEVY D: Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population–based cohort. J Am Coll Cardiol. 1999; 33: 1948–1955. [ Links ]
9. DAHLOF B, PENNERT K, HANSSON L: Reversal of left ventricular hypertrophy in hypertensive patients: a meta–analysis of 109 treatment studies. Am J Hypertens 1992; 5: 95–110. [ Links ]
10. SCHMIEDER R, MARTUS P, KLINGBEIL A: Reversal of left ventricular hypertrophy in essential hypertension: a meta–analysis of randomized double–blind studies. JAMA 1996: 275: 1507–1513. [ Links ]
11. GOTTDIENER JS: Measuring diastolic function. J Am Coll Cardiol 1991; 18: 83–84. [ Links ]
12. TRIMARCO B, DELUCA N, ROSIELLO G, RICCIARDELLI B, BETOCCHI S, FILARDI PP, ET AL: Improvement of diastolic function after reversal of left ventricular hypertrophy induced by long–term antihypertensive treatment with tertalol. Am J Cardiol 1989; 64:745–751. [ Links ]
13. MUIESAN ML, AGABITI–ROSEI E, ROMANELLI G, BESCHI M, CASTELLANO M, ALARI G, ET AL: Improved left ventricular systolic and diastolic function after regression of cardiac hypertrophy, treatment withdrawal, and redevelopment of hypertension. J Cardiovasc Pharmacol 1991; 17 (Suppl 2): S179–S181. [ Links ]
14. WHITE WB, SCHULMAN P, KARIMEDDINI, MK, SMITH VE: Regression of left ventricular mass is accompanied by improvement in rapid left ventricular filling following antihypertensive therapy with metoprolol. Am Heart J 1989; 117: 145–150. [ Links ]
15. MOTZ W, STRAUER BE: Left ventricular function and collagen content after regression of hypertensive hypertrophy. Hypertension 1989; 13: 43–50. [ Links ]
16. INOUYE IK, MASSIE BM, LOGE D, SIMPSON P, TUBAU JF: Failure of antihypertensive therapy with diuretic, beta–blocking and calcium channel–blocking drugs to consistently reverse left ventricular diastolic filling abnormalities. Am J Cardiol 1984; 53: 1583–1587. [ Links ]
17. SEN S, BUMPUS FM: Collagen synthesis in development and reversal of cardiac hypertrophy in spontaneously hypertensive rats. Am J Cardiol 1979; 44: 954–958. [ Links ]
18. CASALE PN, DEVEREUX RB, MILNER M, ZULLO G, HARSHFIELD GA, PICKERING TG, ET AL: Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann lntern Med 1986; 105: 173–178. [ Links ]
19. NISHIMURA RA, ABEL MD, HATLE LK, TAJIK AJ: Assessment of diastolic function of the heart: background and current applications of Doppler echocardiography. Part II. Clinical studies. Mayo Clin Proc 1989; 64: 181–204. [ Links ]
20. SAHN DJ, DEMARIA A, KISSLO T: Committee on M–mode standardization of the American Society of Echocardiography: recommendations regarding quantitation in M–mode echocardiographic measurements. Circulation 1978; 58: 1072–1083. [ Links ]
21. DEVEREUX RB: Detection of left ventricular hypertrophy by M–mode echocardiography. Anatomic validation, standardization, and comparison to other methods. Hypertension 1987; 9 (Suppl II): II19–II26. [ Links ]
22. SHAHI M, THOM S, POULTIER N, SEVER PS, FOALE RA: Regression of hypertensive left ventricular hypertrophy and left ventricular diastolic function. Lancet 1990; 336: 458–461. [ Links ]
23. HABIB G, MANN DL, ZOGHBI WA: Normalization of cardiac structure and function after regression of cardiac hypertrophy. Am Heart J 1994; 128: 333–343. [ Links ]
24. SZLACHCIC J, TUBAU JF, VOLLMER C, MASSIE B: Effect of diltiazem on left ventricular mass and diastolic filling in mild to moderate hypertension. Am J Cardiol 1989; 63: 198–201. [ Links ]
25. SOLOMON SD, JANARDHANAN R, VERMA A, BOURGOUN M, DALEY WL, PURKAYASTHA D, ET AL: Effect of angiotensin receptor blockade and antihypertensive drugs on diastolic function in patients with hypertension and diastolic dysfunction: a randomized trial. Lancet 2007; 369: 2079–2087. [ Links ]
26. ZAKYNTHINOS E, PIERUTSAKOS CH, KONSTANTINIDIS K, ZAKYNTHINOS S, PAPADOGIANNIS D: Losarían reduces left ventricular hypertrophy proportionally to blood pressure reduction in hypertensives, but does not affect diastolic cardiac function. Angiology 2004; 55: 669–678. [ Links ]
27. BARRIOS V, ESCOBAR C, CALDERÓN A, TOMÁS JP, RUIZ S, MOYA JL, ET AL: Regression of left ventricular hypertrophy by a candesartan–based regimen in clinical practice. The VIPE study. J Renin Angiotensin Aldosterone Syst. 2006; 7: 236–42. [ Links ]
28. VILLARI B, VASSALLI G, MONRAD ES, CHIARIELLO M, TURINA M, HESS OM: Normalization of diastolic dysfunction in aortic stenosis late after valve replacement. Circulation 1995; 91: 2353–2358. [ Links ]
29. BEZANTE G P, CHEN X, MOLINARI G, VALBUSA A, DEFERRARI L, SEBASTIANI V, ET AL: Left ventricular myocardial mass determination by contrast enhanced colour Doppler compared with magnetic resonance imaging. Heart 2005; 91: 38–43. [ Links ]
30. FOPP M, DUNCAN BB, ROHDE LEP: Echocardiography–based left ventricular mass estimation. How should we define hypertrophy? Cardiovascular Ultrasound 2005; 3: 17. [ Links ]
31. LANG RM, BIERIG M, DEVEREUX RB, FLACHSKAMPF FA, FOSTER E, PELLIKKA PA: Recommendations for chamber quantification. Eur J Echocardiography 2006; 7: 79–108. [ Links ]














