Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Archivos de cardiología de México
versão On-line ISSN 1665-1731versão impressa ISSN 1405-9940
Arch. Cardiol. Méx. vol.71 no.2 Ciudad de México Abr./Jun. 2001
Comunicaciones breves
Wolff-Parkinson-White syndrome associated to scimitar syndrome. Percutaneous radiofrequency catheter ablation previous to surgical repair
Syndrome de Wolff-parkinson-White asociado a síndrome de cimitarra. Ablación percutánea por radiofrecuencia previo a reparación quirúrgica
Elsa Silva Oropeza,* Arturo Martínez Sánchez,** Carlos Meléndez López,*** Guillermo Valero Elizondo****
Hospital de Cardiología CMN, Siglo XXI, IMSS. México, D.F.
* Department of Cardiology and Electrophysiology.
** Department of Pediatric Cardiology.
*** Department of Cardiovascular Surgery.
**** Department of Pathology.
Correspondencia
Elsa Silva Oropeza.
Ejército Nacional 475, 3er piso, 11520 México, D.F.
(esilva@starnet.net.mx)
Aceptado: 11 de abril de 2001
Abstract
Scimitar syndrome and Wolff-Carkinson-White association has not been reported during the era of catheter ablation. We present our personal experience with percutaneous radiofrequency ablation, a technical challenge related with Scimitar's anatomical variants and follow-up after surgical repair of the latter.
Key words: Catheter ablation, Tachycardia, WCW syndrome, Scimitar syndrome.
Resumen
La asociación de los síndromes de Wolff-Carkin-son-White y de cimitarra no ha sido reportada en la era de la ablación transcatéter. Presentamos nuestra experiencia en torno a la ablación percutánea con radiofrecuencia, un reto particular ante las modificaciones cardiacas propias del síndrome de cimitarra, y el seguimiento posquirúrgico para esta última.
Palabras clave: Ablación por radiofrecuencia. Taquicardia. Síndrome de W-C-W. Síndrome de cimitarra.
Introduction
We describe the case of a 24 year-old female whit a very unusual association of WPWS and Scimitar syndrome, who underwent conventional percutaneous catheter ablation, followed by surgical repair two months later. This unusual association has not been reported before and some comments on the technical catheter ablation approach are made.
Case report
A 24 year-old female was studied due to tachycardia. She had a history in infancy of frequent respiratory infections and heart failure. At that time, her first cardiac catherization revealed partial anomalous venous drainage, mild pulmonary artery hypertension, hypoplasia of the right lung, and dextroposition of the heart.
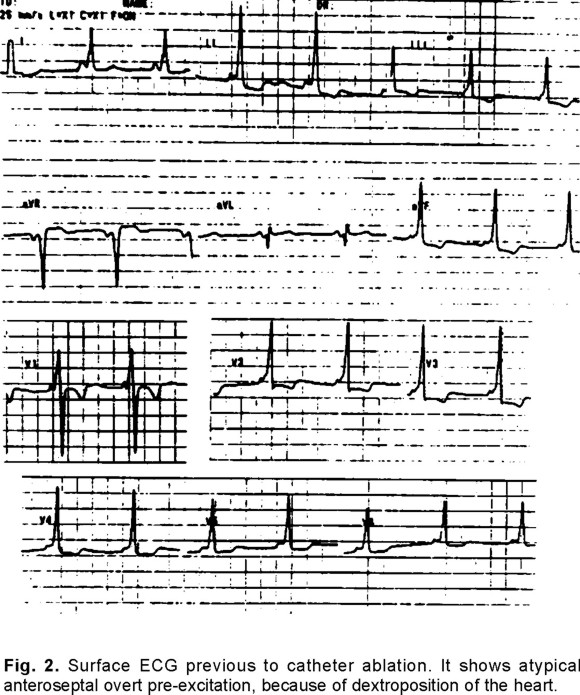
She underwent frequent episodes of supraventricular tachycardia that were partially controlled by oral dysopiramide or propafenone, but she abandoned medical treatment due to gastric intolerance 3 years before admission. Tachycardia episodes were well tolerated, but occasionally she complained of dysnea and dizziness. Eventhough physical examination was irrelevant, it was not clear if symptoms were strictly imputable to tachycardia or because of Scimitar syndrome (Fig. 1). Surface ECG in sinus rhythm (Fig. 2) showed an atypical WPWS pre-excitation pattern with negative delta wave in VL lead, normal QRS axis in the frontal plane, and early RS transition in V1 (RS complexes in V1 and predominant wide R-complexes through V2-6); during tachycardia, narrow QRS complexes, 160 bpm, and no evidence of retrograde P wave were recorded. An echocardiogram concluded ASD sinus venous defect, no pulmonary hypertension, AV and VA concordance and dextrocardia. She refused to continue on medical treatment as well as surgical repair, and underwent an electrophysiologic study (EPS), disclosing the presence of right anteroseptal atrioventricular (AV) accessory pathway (AP). Induced sustained orthodromic atrioventricular reciprocating tachycardia (AVRT) showed earliest retrograde atrial activation just above the His catheter recording. This was followed by an unsuccessful radiofrequency (RF) ablation session, and intracardiac mapping lasted more than 3 h due to abnormal anatomy. A new cardiac catheterization study following EPS was done and detailed: all right pulmonary veins connected to the inferior vena cava (IVC); dilatation of right cardiac cavities; atrial septal defect (ASD) with bi-directional shunt (Qp/Qs 3.4:1); mild tricuspid regurgitation, dextrocardia and the absence of anomalous systemic arterial blood supply to the right lung (Fig. 3). At this time, surgical repair was seriously considered.


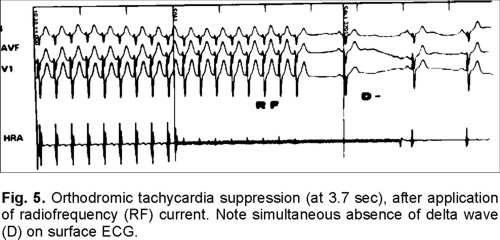
A second EPS, mapping the AP prior to surgical ablation, was performed. Induced AVRT facilitated mapping of AP localization more accurately, with almost continuous VA complexes and a probable intermediate Kent potential (Fig. 4), followed by successful catheter ablation (Mansfield-Webster Catheters. Boston Scientific, MA, USA) achieved after 24 RF applications (Radionics RFG-3D). After the last two applications, mean power was reduced to 24 watts, due to chest pain, delta wave was negative, but early recurrence required another RF application, which yielded permanent results and no more tachycardia was inducible (Fig. 5).

Two months later, the patient underwent surgical correction in which ASD was repaired and right pulmonary vein baffled to the left atrium. We intentionally looked for RF catheter lesions, identifiedasjustminimalpalechangesdifficult to distinguish from healthy tissue, using anatomical references from the ablation region to identify these lesions. Postoperatively, the patient suffered respiratory distress and long artificial ventilatori support. After 10 days, the patient did not need additional mechanical ventilation and was finally discharged 21 days after surgery.
Two years after catheter ablation and surgery, the patient remains arrhythmia-free as well as cardiovascular-asymptomatic. During follow-up, serial surface ECG (Fig. 6) and Holter monitoring no delta wave and permanent sinus rhythm were found. Stress test showed NYHA functional class I. Echocardiography revealed 44 mmHg systolic pulmonary pressure and LVEF 70%. Respiratory and functional evaluation showed no changes with respect to the pre-surgical test.

Discussion
The present case is particulary interesting and original because of the unusual association of WPWS to any other congenital heart disease. In fact, AV AP is commonly related to Ebstein's anomaly, a very uncommon congenital heart defect.1 At our laboratory, we have seen other rare congenital heart associations to WPWS. These include hypertrophyc cardiomyopathy, bicuspid aortic valve stenosis, and patent ductus arteriosus, in addition to Ebstein's anomaly.2
In congenital heart diseases, supraventricular tachycardias (SVT) are usually present late in life, and have been identified as atrial flutter and/or fibrillation secondary to intrinsic structural and hemodynamic changes. However in the present case, the only clinical and inducible SVT was secondary to an AP.
As far as we know, WPWS associated to Scimitar Sx has not been reported and, for the ablation era, we did not find any previous report in the medical literature in English in the last 10 years.3 Nevertheless, other unusual cases of SVT on Scimitar Sx, have been reported, identified as atrio-ventricular nodal reentrant tachycardia, which seems to be independet from the natural evolution of the Scimitar Sx, and where catheter ablation has been practiced.4,5 Technically speaking AP mapping was particularly complicated in the present case atributable not only to the dilatated right cavities but also to dextroposition and rotation on the heart; in fact, the pre-excitation pattern on the surface ECG resembled a left-lateral AP location, imputable to dextrorotation of the heart. We also assumed that contact of the ablation catheter to the tissue was uncertain due to such a large intracardiac shunt. This explains the prolonged time of ablation sessions, with a cumulative radiation exposure of 2.16 h.
Another original contribution of this case to our experience was the AP ablation percutaneous catheter technique, because the patient originally rejected any surgical procedure, that would allow either ablation or structural repair of defects. The principal indication for surgery in this case was pulmonary-systemic blood flow ratio (Qp/Qs) as large as 3.4:1, when the established surgical Qp/ Qs ratio is < 2; on the other hand, the associated, symptomatology which originally could have been mixed, certainly was aggravated by episodes of SVT.6-8
We are certain that the prior catheter ablation reduced surgical time and potentially prevented frequent post-operative respiratory complications. We also looked for lesion characteristics at the time of surgery. They were discrete in size and minimal changes were appreciated, and confirmed that lesions caused by RF-catheter ablation warrants minimal tissue damage. The final results in the present case allow us to think seriously on the convenience of percutaneous catheter ablation even in complex congenital cardiac defects, especially when total surgical repair is not feasible or until optimal corrective surgery time is defined.
In summary, WPWS and Scimitar syndrome coexistence appears to be a very unusual association. Successful RF-catheter ablation results confirmed feasibility and safety, despite this rare congenital heart disease association.
Percutaneous catheter ablation also contributes to decrease hospital morbidity and mortality rates related with surgical repair of Scimitar syndrome itself, reducing the technical approach to repair just one anomaly.
References
1. Cappayo R, Schlüter M, Weiβ C, Antz M, Koschyk DH, Hofmann T, Kuck KH: Radiofrequency current catheter ablation of accessory atrioventricular pathways in Ebstein's anomaly. Circulation 1996; 94: 376-83.
2. Martínez Flores JE, Silva Oropeza E: Estudio de frecuencia, diagnóstico y tratamiento de arritmias y trastornos de la conducción cardiacos de origen congénito o adquiridos, en edad pediátrica. Creación de una base de datos [Abstr]. Arch Inst Cardiol Mex 1997; 67: 376. [ Links ]
3. Silva E, Escalante F, Martínez A, Meléndez C, Jiménez S: Ablación transcatéter de Sx de Wolff-Parkinson-White en Sx de Cimitarra. Una presentación inusual. [Abstr]. Arch Inst Cardiol Mex 1997; 67: 440. [ Links ]
4. Bakker R, de Weerd G: Electrophysiologic mechanisms and electrocardiographic findings in atrioventricular-nodal reentrant tachycardia in a patient with the scimitar syndrome. Heart Lung 1997; 26: 45-51. [ Links ]
5. Bruinsma GJ, Wever EF, Robles de Medina EO: Radiofrequency catheter ablation of AV nodal reentrant tachycardia in scimitar syndrome. Int J Cardiol 1997; 58: 395-7. [ Links ]
6. Canter CE, Martin TC, Spray TL, Weldon CS, Strauss AW: Scimitar syndrome in childhood. Am J Cardiol 1986; 58: 652-4. [ Links ]
7. Kirklin JW: Atrial septal defect and partial anomalous pulmonary venous connection. In: Kirklin JW, Barratt BB, editors. Cardiac surgery. New York, NY, Churchill Livingstone; 1993; 609-644. [ Links ]
8. Wilson WR Jr, Dbawi MN, Deleon SY, Quiñones JA, Arcilla RA, Sulayman RE, Idriss ES: Technical modifications for improved results in total anomalous pulmonary venous drainage. J Thorac Cardiovasc Surg 1992; 103: 861-70. [ Links ]














