Introduction
Acute cholecystitis is common in the emergency department, and the diagnosis is based on clinical signs and radiological findings.1-3 However, different acute systemic diseases (heart failure, cirrhosis, hepatitis) can produce symptoms and even alterations in complementary diagnostic studies such as gallbladder wall thickening that resemble cholecystitis.4,5 In acute systemic diseases, surgical treatment can produce a higher systemic inflammatory response, increasing morbidity and mortality.6-8 Despite this, many of these pathologies are still confused with cholecystitis and continue to be presented to the surgery department for emergency cholecystectomy, representing a challenge for the surgeon.7 Despite this, few articles explain this entity, persisting the gallbladder edema misdiagnosed as cholecystitis.
The objective of this study is to identify and analyze the patients presented for cholecystectomy with gallbladder edema secondary to acute diseases, confused as cholecystitis in the emergency department of a Regional Reference Center.
Material and Methods
Study design: a retrospective study in a Regional Reference Center was conducted from December 2016 to November 2019. Patients admitted to the emergency department due to suspected acute cholecystitis were analyzed. All patients underwent radiological studies (abdominal ultrasound and CT-scan) and acute cholecystitis was ruled out. Inclusion criteria were patients older than 18 years, with signs, symptoms (colic pain in the right hypochondrium, nausea, vomiting), and radiological findings similar to cholecystitis but without cholecystitis. Patients with radiological findings compatible with lithiasic cholecystitis according to Tokyo 2018 guidelines criteria, like micro lithiasis, anatomical gallbladder alterations (polyps, scleroatrophic, in a Phrygian cap, etc.) or increased gallbladder diameters were excluded.9
Clinical evaluation: the patient’s files with surgical assessment for suspected cholecystitis were retrospectively reviewed. In all patients, comorbidities, medical history, clinical symptoms, laboratories were evaluated, as well as radiographic signs in the abdominal ultrasound or in the abdominal tomography. Surgical indication for suspected cholecystitis, histopathological findings after surgery, the primary cause of gallbladder edema, hospital stay, follow-up, morbidity, and mortality were evaluated.
Statistical analysis: We use descriptive statistics, as well t-student, for continuous variables, χ2, and non-parametric proofs for categorical variables to perform the analysis. A p-value ≤ 0.05 (confidence interval of 95%) was considered statistically significant. The statistical analysis was performed using the program IBM Statistical Package for Social Sciences (SPSS, Statistics version 24.0, Inc, Chicago, IL).
Results
Of 3,393 patients analyzed, 31 patients were presented for cholecystectomy with gallbladder edema confused as cholecystitis, representing 0.91% of the total population. The average age was 43.94 years (range, 18-81), most of them being males (51%, n = 16). Ten patients (32.3%) presented comorbidities, the majority due to diabetes and systemic arterial hypertension. Of these, two patients (6.5%) with type II diabetes, four with type II diabetes, and systemic arterial hypertension (12.9%), one with cerebral vascular disease and arterial hypertension (3.2%), and one patient with antiphospholipid syndrome (3.2%). The rest 21 patients (67.7%) without comorbidities. The characteristics of our population are shown in Table 1.
Table 1: Characteristics of our population (N = 31).
| Variable | n (%) |
|---|---|
| Age (years)* | 43.94 ± 18.28 |
| Gender (male) | 16 (51.6) |
| Comorbidities | |
| DM | 2 (6.5) |
| DM, AH | 4 (12.9) |
| AH, CVA | 1 (3.2) |
| APS | 1 (3.2) |
| Operated patients | 7 (22.5) |
* Mean ± standard deviation.
DM = diabetes mellitus; AH = arterial hypertension; CVA = cerebrovascular accident; APS = antiphospholipid syndrome.
Upon admission, all patients underwent imaging studies for suspected acute cholecystitis (abdominal ultrasonography and or abdominal tomography). In all patients, the gallbladder wall thickening of more than 5 mm (mean: 8.96 mm, range: 5-16 mm) was corroborated, and signs of acute cholecystitis (criteria TG-18) or structural alterations were ruled out. Differences between acute cholecystitis and gallbladder edema in the abdominal ultrasound are shown in Figure 1, and differences in the CT scan are shown in Figure 2, respectively.

Figure 1: Abdominal ultrasound shows differences between acute cholecystitis and gallbladder wall thickening without cholecystitis. A) Wall thickening of the gallbladder due to acute cholecystitis with multiple lithiasis. B) Simple gallbladder edema due to dengue without cholecystitis.
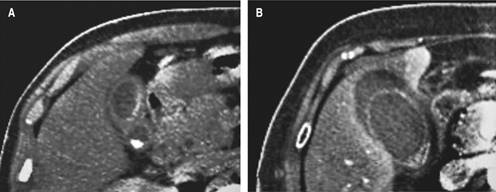
Figure 2: Tomographic differences between typical cholecystitis and simple gallbladder wall thickening. A) Typical cholecystitis gallbladder wall thickening. B) Gallbladder edema in a patient with viral disease without cholecystitis.
The admission diagnoses of these patients were mostly liver diseases (55%, n = 17). Ten patients presented with acute viral hepatitis corroborated by elevated transaminase levels and hepatic viral profile. Five patients presented with decompensated cirrhosis, Child-Pugh B, one patient with non-alcoholic liver disease, and one patient with a left lobe liver tumor who subsequently found a diagnosis of left lobe hepatocellular carcinoma (HCC). Ten patients (32.25%) presented hemorrhagic dengue with abdominal involvement corroborated later in their hospitalization for IgM and IgG antibodies. Two patients presented for cardiovascular diseases, confirming an acute myocardial infarction. One patient presented with fungal pneumonia and one patient with severe acute non-biliary pancreatitis Balthazar D.
After surgical assessment in these 31 cases, in seven patients emergency surgical treatment was performed (22.58%). These patients underwent emergency cholecystectomy for suspected acute cholecystitis. Of these, four patients underwent open cholecystectomy, and three patients underwent laparoscopic cholecystectomy, and one of these patients, also a liver biopsy, was performed due to elevated transaminase in the presence of negative viral panel. In operated patients, the primary diagnosis that produced the gallbladder edema was viral hepatitis in four patients (12.9%), cirrhosis Child-Pugh A in one patient (3.2%), non-alcoholic liver disease in one patient (3.2%), and non-biliary pancreatitis (3.2%) in one patient. In Table 2, we show a definitive diagnosis of our patients who underwent cholecystectomy.
Table 2: Definitive diagnosis of our patients underwent cholecystectomy.
| Diagnosis | Surgery, n (%) |
|---|---|
| Viral hepatitis | 4 (12.9) |
| Cirrhosis | 1 (3.2) |
| Non-alcoholic liver disease | 1 (3.2) |
| Hepatocellular carcinoma | 0 |
| Hemorrhagic dengue | 0 |
| Acute myocardial infarction | 0 |
| Pneumonia | 0 |
| Non-biliary pancreatitis | 1 (3.2) |
| Total | 7 (22.5) |
After surgery, two patients presented complications (6.5%), and none died. Complications were hemoperitoneum and abortion secondary due to transuterine bleeding. The patient with hemoperitoneum was secondary to open cholecystectomy, with 1,500 cc of hepatic bleeding. In this patient reoperation for hemostatic control was needed. Clinical evolution after reoperation was satisfactory, and the patient was discharged without any other complication. The other patient presented transuterine bleeding with the subsequent abortion of 9 weeks gestation. This patient was managed by the gynecology service for hemostatic control and subsequently discharged without other complication. In the histopathological study, no signs of cholesterolosis, or lithiasic inflammation secondary to gallstones were founded. During the hospital follow-up, two patients without surgical treatment died (6.5%). One patient was secondary to acute transmural myocardial infarction and the other patient due to multiorgan failure after massive hemorrhagic dengue with antiphospholipid syndrome.
In the rest of the patient’s misdiagnosis as cholecystitis, presented for cholecystectomy, the gallbladder edema was revalued, and no indication for surgical treatment was found. Subsequently, the patients evolved satisfactorily and were discharged. The average hospital stay was 9.38 days (range, 3-21 days). In patients, without surgical treatment, the hospital stay was 8.7 days (range: 3-12 days), and with surgical treatment was 17 days (range: 14-21 days). The causes of gallbladder edema misdiagnosed as cholecystitis were analyzed with the different diagnosis and pre-surgical variables, and no significance was found. Besides, post-surgical complications were analyzed with the pre-surgical diagnosis without finding significance. In operated patients, the analyst of hospital stay was significantly larger than patients without surgery, finding statistical significance (p = 0.004). No complications after 30 days of follow-up were found.
Discussion
Different systemic diseases can produce gallbladder wall thickening due to edema demonstrated by ultrasound or tomography, and this could be confused with acute cholecystitis. Some of these diseases are self-limited such as hepatitis A or dengue, but other diseases become fatal, and recognizing them on time can improve the prognosis of these patients.6,7,10,11 The presentation of these diseases is sometimes not so clear, and experience is required to rule out surgical treatment. In addition to all this, there is a lack of evidence worldwide, especially in Latin America, where this diagnostic confusion has been less reported, making recognition of this situation more difficult.
Lithiasic cholecystitis is a prevalent disease reported in up to 10% of the population. Unlike lithiasic cholecystitis, gallbladder edema without lithiasis is a rare condition. In our series, the frequency of gallbladder wall thickening without cholecystitis was only 0.95% of all patients presented for cholecystectomy. Due to this low frequency of presenting wall thickening in patients with typical symptoms, many surgical teams prefer to perform cholecystectomy due to the risk of not detected silent lithiasis, with its subsequent complications.12-14
Unlike the mechanism in lithiasic cholecystitis where the luminal obstruction of the cystic duct produced mucous distention, ulceration, and infiltration of leukocytes, in patients with non-lithiasic gallbladder edema the mechanism occurs due to vascular permeability, inflammation, and increased portal venous pressure although the exact pathophysiology is not clear identified.7,15
In viral diseases such as hepatitis, viral infiltrations, as well as direct cellular liver damage, are the cause of gallbladder edema. Hepatitis A, a common cause of acute viral disease, causes acute liver failure in 0.5% as well as thickening of the gallbladder wall as an extrahepatic involvement. In our patients, the pathologies that were most confused with acute cholecystitis were liver diseases. In these cases, viral hepatitis was mostly self-limited, but in 12.9%, they received surgical treatment, two presented complications, and one patient presented a severe complication due to 1,500 cc hemoperitoneum.16
In other viral diseases like dengue, it has been reported that in the early stages, capillary plasma leakage occurs, leading to thickening of the gallbladder wall in up to a third of them.17 In our series, dengue cases occurred with a frequency of 32.25% in all of them with thrombocytopenia and the presence of spontaneous hemorrhage, and one patient with dengue hemorrhagic fever and antiphospholipid syndrome died. In these patients, the indication of surgical treatment was not presented, probably due to the high risk of spontaneous hemorrhage induced by severe thrombocytopenia in the initial stage of the disease. In all these patients, gallbladder edema decreased after the initial stage, and indication for surgical treatment was not subsequently presented.
Cardiovascular diseases also occur due to hepatic venous congestion. However, their relationship has not been fully established. In most cases, a relationship between cardiovascular diseases and gallbladder edema has been reported.18 In our series, we only found two patients without surgical treatment in whom acute infarction occurred, one of them died from acute transmural myocardial infarction, and the other patient presented sequel of congestive heart failure. In addition, one of our patients presented fungal pneumonia. This etiology has not been reported as a cause of gallbladder wall thickening until now.
After the statistical analysis, the gallbladder wall thickening was evaluated, and no relation to surgical treatment was found. Regarding this finding, some studies show gallbladder thickening due to edema as a direct indicator of plasma capillary leakage, especially in patients with dengue.17 In this study, the relationship between the wall thickening had no significance with other variables.
In some cases of silent lithiasis, surgical treatment is indicated, which could be the cause of deterioration in these patients. In this series, there was no direct relationship between morbidity and mortality after surgical treatment, but we find statistical significance with the hospital stay in post-surgical patients. In our experience, the indication of cholecystectomy must be very careful when dealing with these types of patients because the most important is the attention of its underlying pathology. More prospective studies are required to increase information in this regard.











 nueva página del texto (beta)
nueva página del texto (beta)


